Case study: Ultrasound-guided intercostal nerve block for post-herpetic neuralgia
Case presentation
A 48-year-old male patient presented with severe pain localized to the left thoracic region, consistent with post-herpetic neuralgia following a recent episode of shingles involving the left T6 dermatome. The patient had no other significant medical history. The pain was described as sharp, burning, and significantly impacting the patient’s daily activities. Conventional analgesic medications provided limited relief, prompting the consideration of an ultrasound-guided intercostal nerve block for targeted pain management.
Nerve block technique
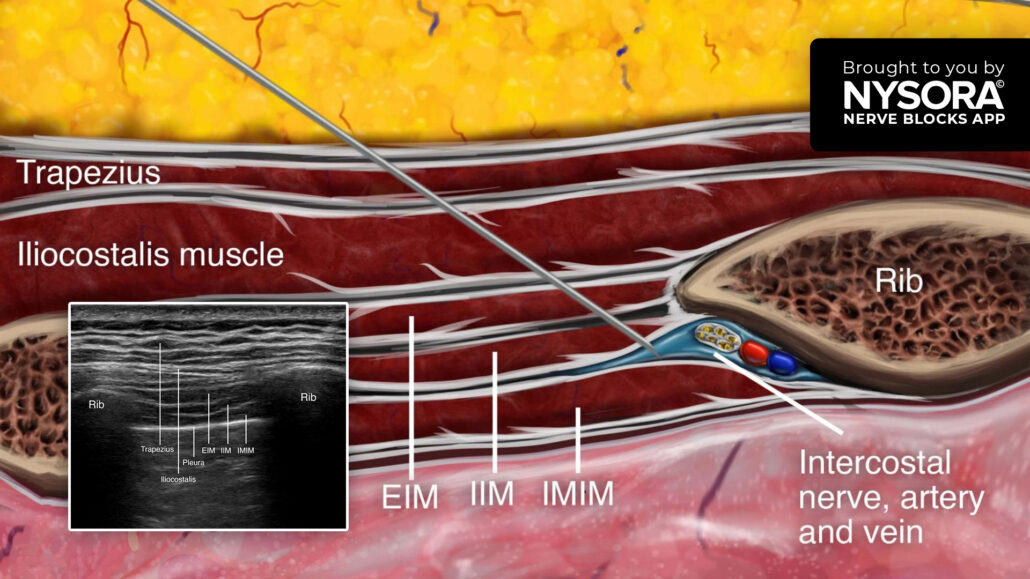
A high-frequency linear transducer was used to scan the left thoracic region, focusing on the intercostal spaces. Real-time ultrasound imaging provided identification of the targeted intercostal space, ribs, and underlying neurovascular structures.
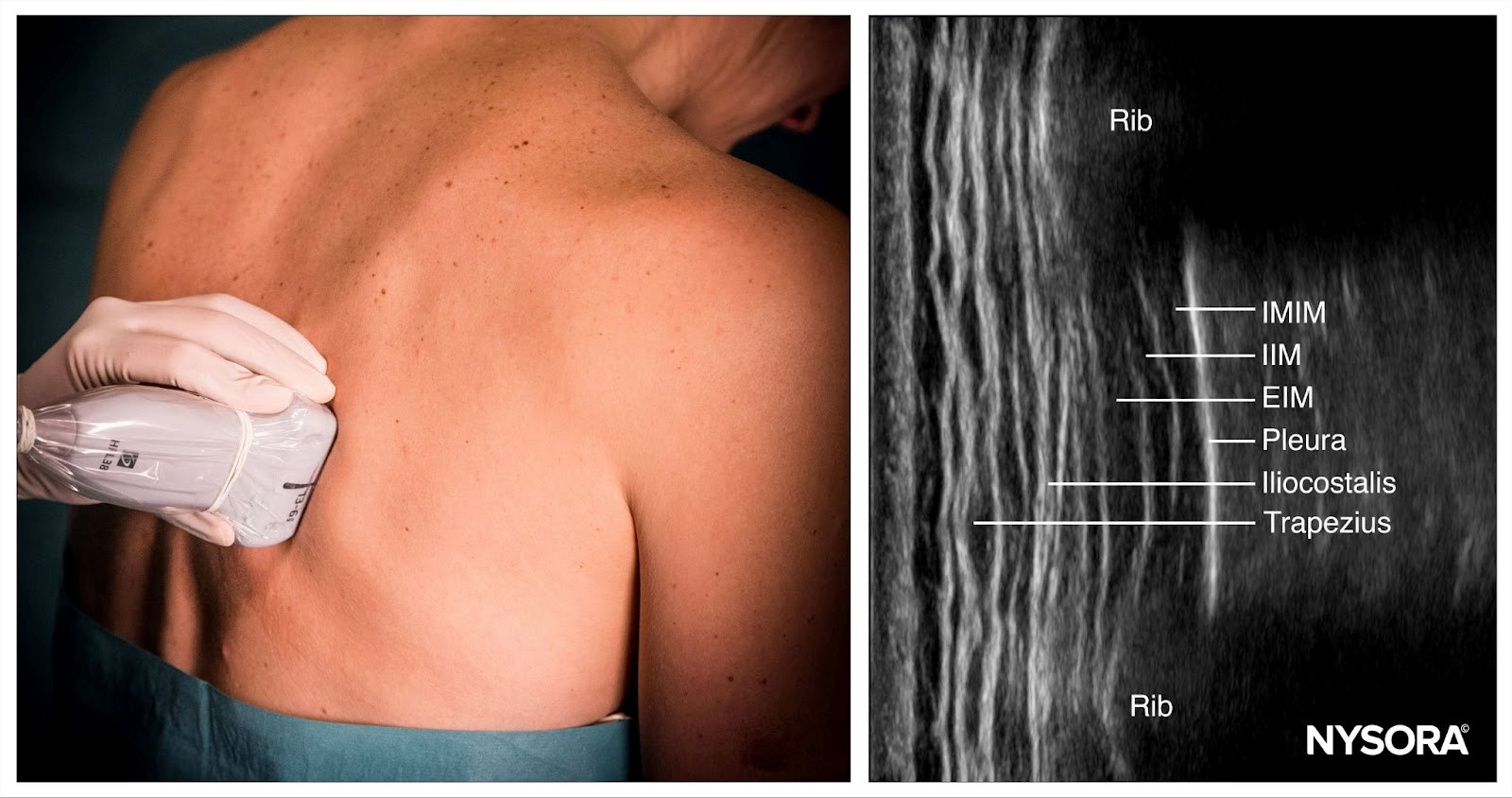
Intercostal nerve block; transducer position and sonoanatomy. IMIM, innermost intercostal muscle; IIM, internal intercostal muscle; EIM, external intercostal muscle.
Next, a 25-gauge needle was inserted in-plane to penetrate the external and internal intercostal muscles. The optimal target needle endpoint is the location just below the internal intercostal muscle to ensure that the needle tip remains superficial to the parietal pleura. Then, 4 mL of bupivacaine 0.5% with 1:300,000 epinephrine was injected into the intercostal sulcus around the intercostal nerve. The procedure was repeated for additional intercostal spaces, depending on the extent of the patient’s pain and response.
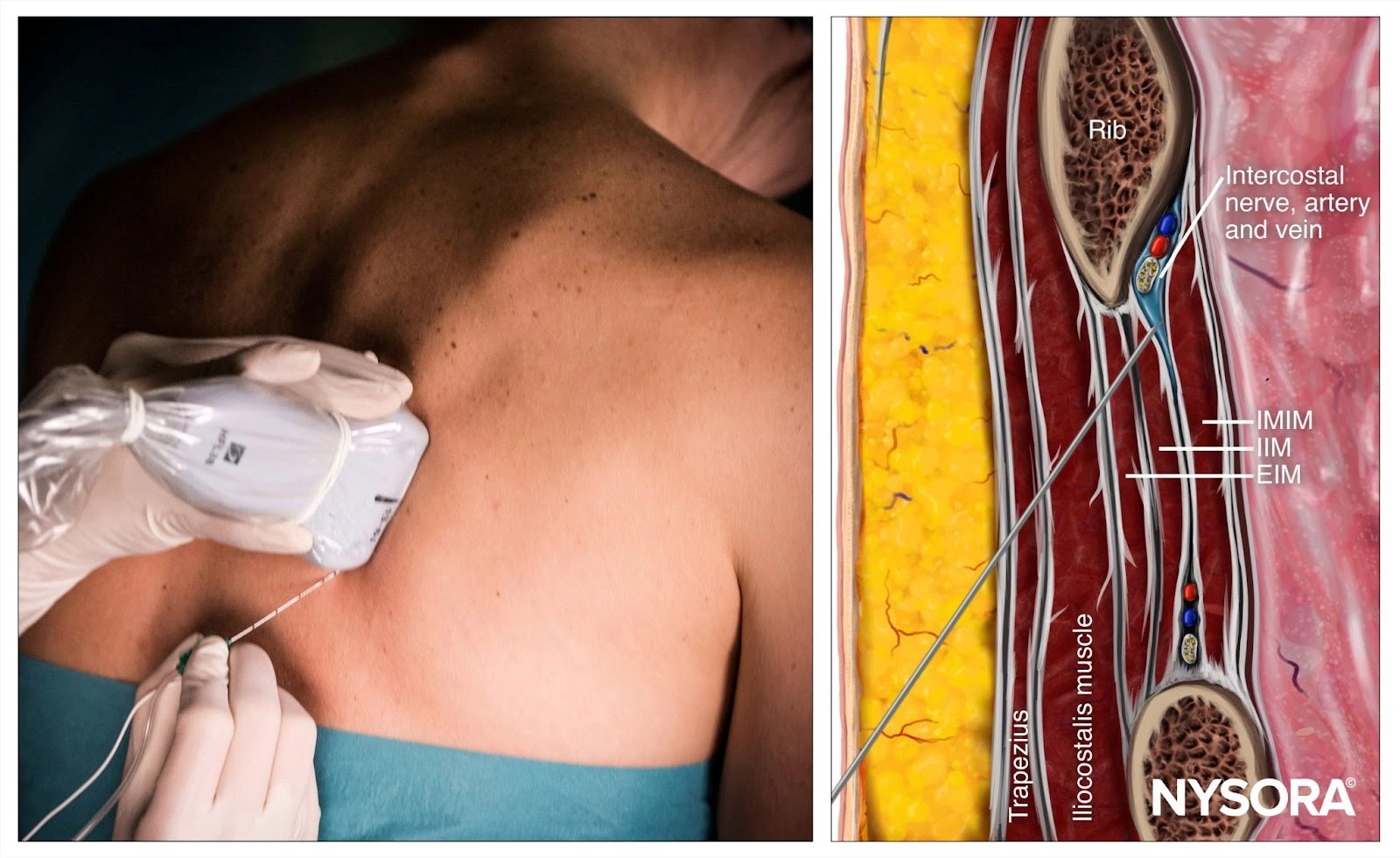
Intercostal nerve block; Reverse Ultrasound Anatomy with needle insertion in-plane and local anesthetic spread (blue). IMIM, innermost intercostal muscle; IIM, internal intercostal muscle; EIM, external intercostal muscle.
Patient outcome
Following the ultrasound-guided intercostal nerve block, the patient experienced significant pain relief within 30 minutes. The sharp, burning pain was reduced to a mild ache, allowing him to resume normal activities. Over the next few days, the pain continued to diminish, and the patient reported improved sleep and overall functionality. No adverse events or complications were observed.
Ultrasound-guided intercostal nerve block for acute herpes zoster: A promising approach for pain relief and PHN prevention
A painful, band-like vesicular rash along specific dermatomes characterizes herpes zoster. It results from the reactivation of the varicella-zoster virus, which remains dormant in the sensory ganglia after initial infection with chickenpox. Shingles are prevalent, affecting about 20% to 30% of the population, with the incidence rising significantly in those over 50. One of the most challenging complications of herpes zoster is postherpetic neuralgia (PHN), defined as pain that persists for more than 90 days after the rash has resolved. While PHN affects a smaller proportion of younger patients, it becomes more common with age, impacting up to 20% of individuals over 80 years old. Despite the availability of treatments for acute herpes zoster, PHN remains difficult to prevent and treat, making managing shingles-associated pain a critical area of research.
Understanding acute herpes zoster pain (zap)
Acute herpes zoster pain originates from inflammation and nerve damage in the dorsal root ganglia and peripheral nerves. This pain can be debilitating and long-lasting, potentially leading to central sensitization, where the nervous system becomes hypersensitive to stimuli. If left untreated or poorly managed, acute herpes zoster pain can progress to PHN, which can significantly impact a patient’s quality of life. The standard treatment for acute herpes zoster involves antiviral therapy (AVT) aimed at reducing viral replication and minimizing the severity of the rash. However, AVT alone does not provide significant pain relief, nor does it effectively reduce the risk of developing PHN.
Novel approach: ultrasound-guided nerve blocks
Recent advancements in pain management have introduced ultrasound-guided nerve blocks, particularly the thoracic paravertebral and intercostal nerve blocks, as potential solutions for acute herpes zoster-associated pain and PHN prevention. The retrospective, case-controlled trial of Li et al. (2024) compared the efficacy of these two nerve block techniques combined with AVT in patients suffering from acute herpes zoster pain. This study aimed to determine which method was more effective in managing acute pain and preventing the transition to PHN.
Methods
- The trial enrolled 128 patients with moderate to severe thoracic herpes zoster pain, divided into three treatment groups:
- Control group: AVT alone.
- TPVB group: AVT combined with ultrasound-guided thoracic paravertebral block (TPVB).
- ICNB group: AVT combined with ultrasound-guided intercostal nerve block (ICNB).
- The primary endpoint was the herpes zoster-related burden of illness over 30 days, calculated from pain severity and the duration of symptoms.
- Secondary endpoints included procedure time, rescue analgesic requirements, incidence of PHN, and health-related quality of life.
Results
The thoracic paravertebral nerve block and intercostal nerve block demonstrated significantly better outcomes than AVT alone in reducing the burden of illness associated with herpes zoster. Here are the main results:
- Pain reduction: Both nerve block techniques significantly decreased acute herpes zoster pain compared to the control group.
- PHN prevention: The incidence of PHN was significantly lower in the TPVB and ICNB groups compared to the control group at 90 days and 180 days.
- Rescue analgesic requirements: Patients in the TPVB and ICNB groups required fewer rescue analgesics than those in the control group, further confirming the efficacy of nerve blocks in pain management.
- Quality of life improvements: Both intervention groups reported better scores on the assessment across various domains, including mobility, self-care, pain/discomfort, and anxiety/depression.
Advantages of the intercostal nerve block
While both thoracic paravertebral nerve block and intercostal nerve block were effective in reducing acute herpes zoster pain and preventing PHN, the intercostal nerve block offers several advantages over the thoracic paravertebral nerve block, making it an attractive alternative:
- Shorter procedure time: The intercostal nerve block procedure was quicker, with an average duration of 11.69 minutes compared to 16.47 minutes for the thoracic paravertebral nerve block. This time-saving aspect is particularly beneficial in busy clinical settings.
- Fewer side effects: Patients undergoing intercostal nerve block reported fewer side effects, particularly during the puncture phase.
- Lower risk of complications: Intercostal nerve block is considered a safer procedure, with a lower risk of complications such as pneumothorax or intravascular puncture due to its more superficial and lateral approach.
Ultrasound-guided nerve blocks: a new standard?
The thoracic paravertebral and intercostal nerve blocks have emerged as promising interventions for managing acute herpes zoster-associated pain and reducing the risk of PHN. Using ultrasound guidance is crucial, as it allows for real-time visualization of the needle and surrounding anatomical structures, ensuring accurate local anesthetic delivery and minimizing complications. Given the shorter procedure time, lower incidence of side effects, and comparable efficacy in preventing PHN, the intercostal nerve block is poised to become a preferred alternative to the thoracic paravertebral block for patients with thoracic herpes zoster.
Conclusion
Ultrasound-guided intercostal nerve block is a practical and effective intervention for managing acute herpes zoster pain and reducing the risk of postherpetic neuralgia. With its shorter procedure time and lower complication rate than thoracic paravertebral block, the intercostal nerve block is a promising alternative for clinicians looking to optimize pain management in patients with shingles.
For more detailed information, refer to the full article in The Korean Journal of Pain.
Li X, Yuan R, Yang Y, Qin Z, Fu R. Assessment of ultrasound-guided intercostal nerve block for acute herpes zoster and its’ possible prophylaxis for postherpetic neuralgia: a retrospective and case-controlled trial. Korean J Pain. 2024;37(4):343-353. doi:10.3344/kjp.24111
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!