Learning objectives
- Getting familiar with an evidence-based, structured approach to managing a difficult airway
Signs and symptoms
- Failure to ventilate or intubate a patient
- Airway edema from repeated intubation attempts
- Desaturation and subsequent hypoxia
- Absent or minimal end-tidal CO2
- Insufficient tidal volumes
- Cyanosis
- Cardiac arrest
Complications contributing to difficult airway management
- History of difficult intubation
- Distorted airway anatomy
- Snoring
- Obstructive sleep apnea
- Diabetes mellitus
- Increasing Mallampati and modified Mallampati scores
- Thyromental distance < 6 cm
- Sternomental distance <12.5 cm
- Interincisor distance < 4 cm
- Large neck circumference
- Reduced neck mobility
- Acquired or congenital disease states:
- Ankylosing spondylitis
- Degenerative osteoarthritis
- Treacher–Collins
- Klippel–Feil syndrome
- Down syndrome
- Face-mask ventilation:
- Obesity
- Large tongue
- Beard
- Toothless mouth
- Distorted facial anatomy
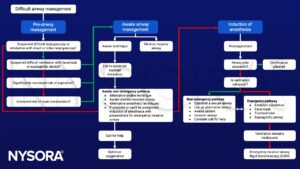
Guidelines
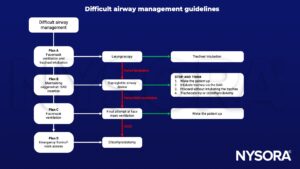
Management
Keep in mind
- Always screen and anticipate a suspected difficult airway
- Decide whether awake intubation is indicated
- Planning for a failed intubation should be part of every pre-induction briefing
- Ensure proper positioning of the patient
- Preoxygenation is recommended for all patients, apnea time without desaturation (SaO2 <90%) is generally limited to 1-2 minutes, and with proper preoxygenation, this period can be extended to 8 minutes
- All anesthesiologists should be trained to use, and have immediate access to a video laryngoscope
- In case of a failed intubation, a supraglottic airway is recommended to maintain adequate oxygenation
- In case of a failed intubation or ventilation, consider calling for help early
- If both endotracheal intubation and ventilation with an SGA fail after having ensured adequate depth of anesthesia and relaxation, the safest option is to attempt mask ventilation and when successful, wake the patient up and postpone surgery
- In a CICO (can’t intubate can’t oxygenate) situation, scalpel cricothyroidotomy is recommended as the preferred rescue technique
Suggested reading
- Apfelbaum JL, Hagberg CA, Connis RT, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136(1):31-81.
- Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827-848.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







