Blown veins: Causes, management, and best practices
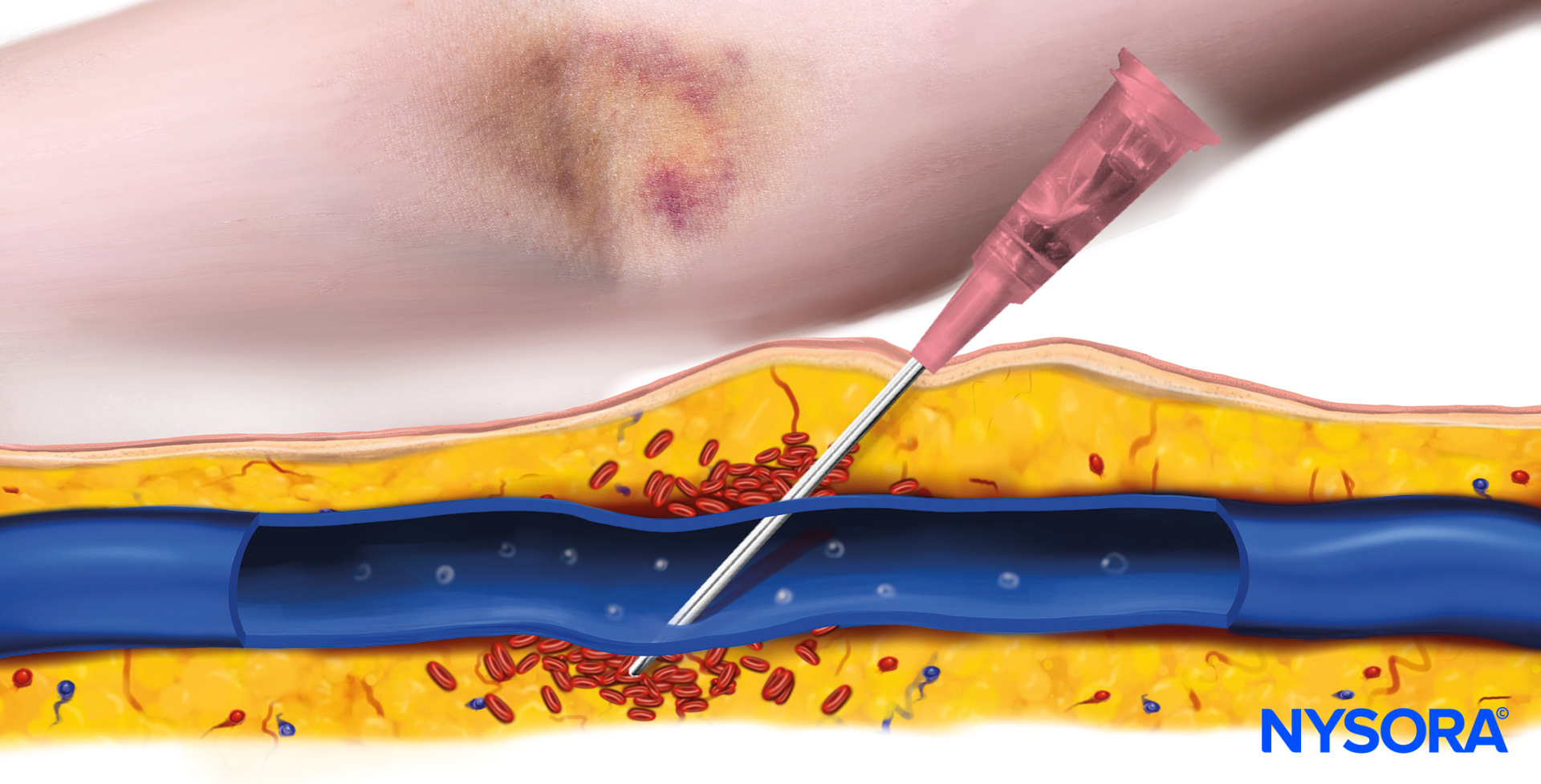
Blown veins are a common complication during intravenous (IV) catheter insertion, often occurring when the needle pierces through the vein wall or causes it to burst. This issue results in blood leaking into the surrounding tissue, causing bruising, discomfort, and potentially more serious complications if not managed promptly. This article explores the causes, symptoms, and effective strategies for managing blown veins, with practical advice for healthcare professionals.
What is a blown vein?
A blown vein occurs when:
- The needle penetrates through the vein or causes it to rupture.
- Blood escapes into nearby tissues, forming a bruise or hematoma.
- The damage often results in swelling, pain, and discoloration around the insertion site.
Causes:
- Needle size: Using an incorrect needle size that doesn’t match the vein’s diameter can lead to perforation.
- Needle angle: Inserting the needle at an incorrect angle, particularly in veins that roll or are fragile, increases the risk.
- Vein condition: Fragile vein walls are common in elderly or chronically ill patients, making them susceptible to damage.
Symptoms of a blown vein
When a vein is blown, several symptoms may become noticeable:
- Bruising: A bruise (hematoma) develops around the insertion site, and it may be accompanied by a visible mark from a previous attempt.
- Swelling: The area may swell due to blood and fluids leaking into surrounding tissue.
- Discomfort: Pain or tenderness is common at the site of the injury.
- Discoloration: Extravasation of hemoglobin can cause discoloration, indicating multiple failed attempts.

Multiple failed attempts in a patient will lead to bruising and discoloration due to the extravasation of hemoglobin.
What to do when a vein blows
Addressing a blown vein promptly is crucial to prevent further complications, such as blood clot formation, tissue inflammation, infection, or interruptions in necessary IV treatments. Here are the key steps:
- Look proximally:
- Attempt to insert the IV catheter proximal to the blown vein (closer to the heart). This part of the vein remains intact and can still serve as a reliable route for IV access.
- Avoid inserting the catheter distal (further away from the heart) to the blown vein, as this may result in leakage due to the damaged section above.
- Seek alternative sites:
- If the vein is not viable or multiple attempts have already failed, choose a different vein or switch to another extremity altogether to ensure successful IV access.
- Use proper needle technique:
- Adjust needle size and insertion angle based on the patient’s vein type to minimize the risk of further damage.
Practical advice for preventing and managing blown veins
To reduce the risk of blown veins and manage them effectively when they occur, healthcare professionals should follow these practical tips:
- Start distally:
- Begin IV insertion at the most distal (furthest) part of the vein, especially if there is no hematoma present. This strategy preserves the proximal sections for later use if subsequent attempts are needed.
- Catheter replacement:
- Replace a functioning catheter every 3-4 days to prevent complications like phlebitis or infection. When replacing a catheter in the same vein, position it proximal to the previous site or, if needed, use a different vein entirely.
Complications of untreated blown veins
Failing to address blown veins can lead to further issues, such as:
- Blood clot formation: Damage to the vein wall can cause clot formation, posing a risk of deep vein thrombosis (DVT) or other complications.
- Infection: A damaged vein increases the risk of introducing bacteria, potentially leading to infection if not managed promptly.
- Delayed treatment: Multiple failed attempts or complications can result in delays in administering essential IV medications or fluids.
Best Practices for Healthcare Professionals
To minimize the risk of blown veins and ensure effective IV therapy, healthcare professionals should consider the following best practices:
- Vein Assessment: Evaluate the condition of veins before attempting insertion. In patients with known fragile veins, consider using ultrasound guidance to locate and access veins more precisely.
- Proper Equipment Selection: Choose the appropriate catheter size and needle based on the patient’s vein type and condition to avoid unnecessary trauma.
- Technique Training: Regular training and refreshers for healthcare workers on proper IV insertion techniques can significantly reduce the incidence of blown veins and improve patient outcomes.
- Patient Communication: Inform patients of the procedure and any risks associated with IV therapy. For patients with a history of difficult veins, consider discussing alternative access methods, such as a peripherally inserted central catheter (PICC) line, if appropriate.
Conclusion
Blown veins are a manageable complication with proper technique and quick intervention. Recognizing the symptoms early and taking the correct steps can prevent further complications and ensure that IV therapy is effective and comfortable for the patient. By adhering to best practices and continually improving techniques, healthcare professionals can reduce the incidence of blown veins and provide better care.
Explore many resources, including easy-to-follow algorithms, expert tips, and clinical videos, on NYSORA’s IV Access App! It’s perfect for healthcare professionals at any level. Download today and start improving your IV catheterization techniques! All this valuable content is also available in NYSORA’s comprehensive IV manual on Amazon.