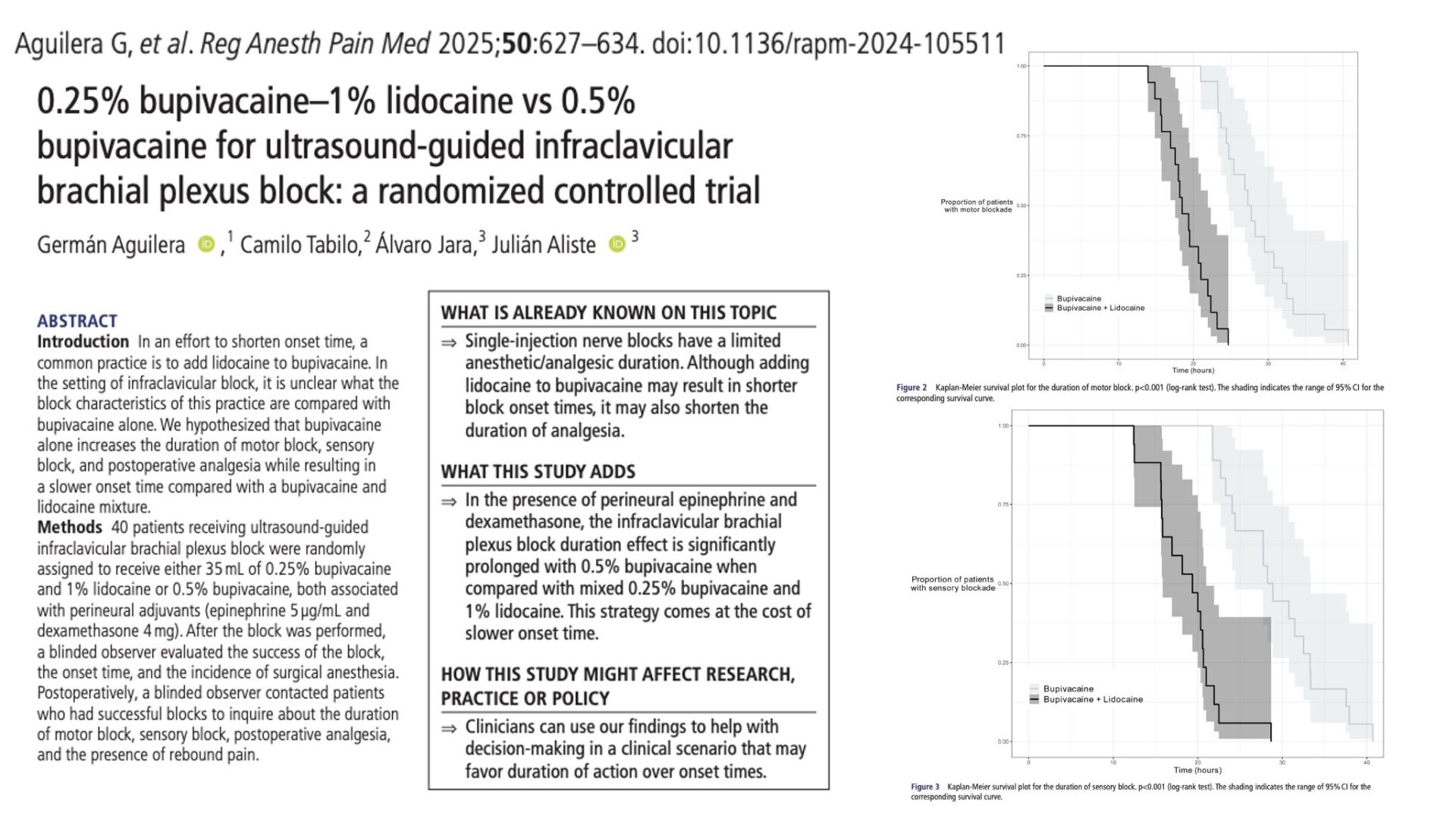
A recent randomized study explored the comparative effectiveness of using 0.5% bupivacaine alone versus a mixture of 0.25% bupivacaine and 1% lidocaine in ultrasound-guided infraclavicular brachial plexus blocks for upper extremity surgeries. The study involved 40 patients who were randomly assigned to receive either the bupivacaine-lidocaine mixture or bupivacaine alone, with both groups receiving perineural adjuvants, specifically epinephrine (5 µg/mL) and dexamethasone (4 mg). A blinded observer evaluated block success, onset time, and the incidence of surgical anesthesia. Postoperatively, the duration of motor and sensory blocks, postoperative analgesia, and the presence of rebound pain were assessed through patient follow-up.
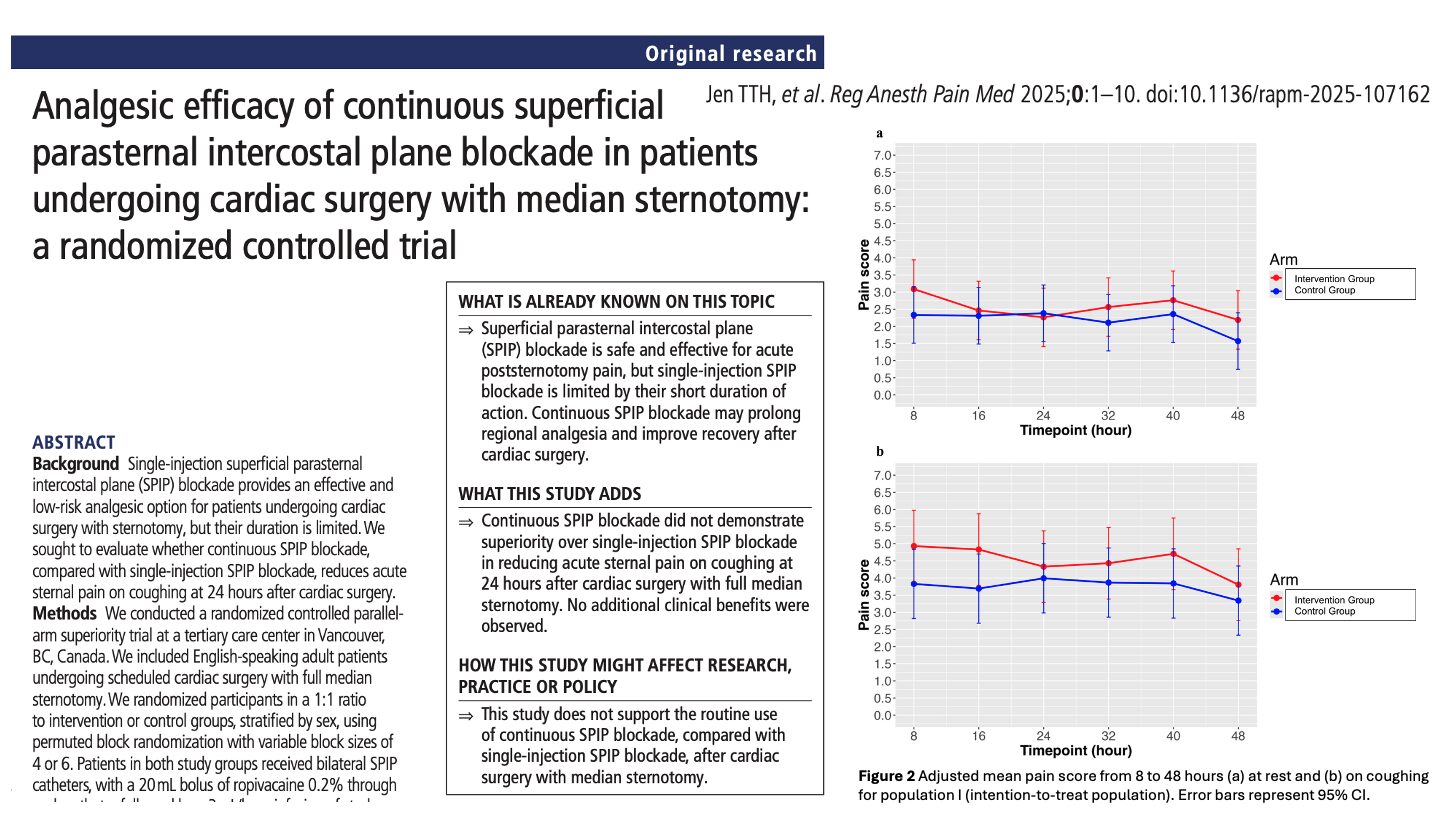
The results demonstrated significant differences between the two groups. The mean motor block duration for the bupivacaine-alone group was 28.4 hours, compared to 18.9 hours for the bupivacaine-lidocaine mixture, representing a mean difference of 9.5 hours.
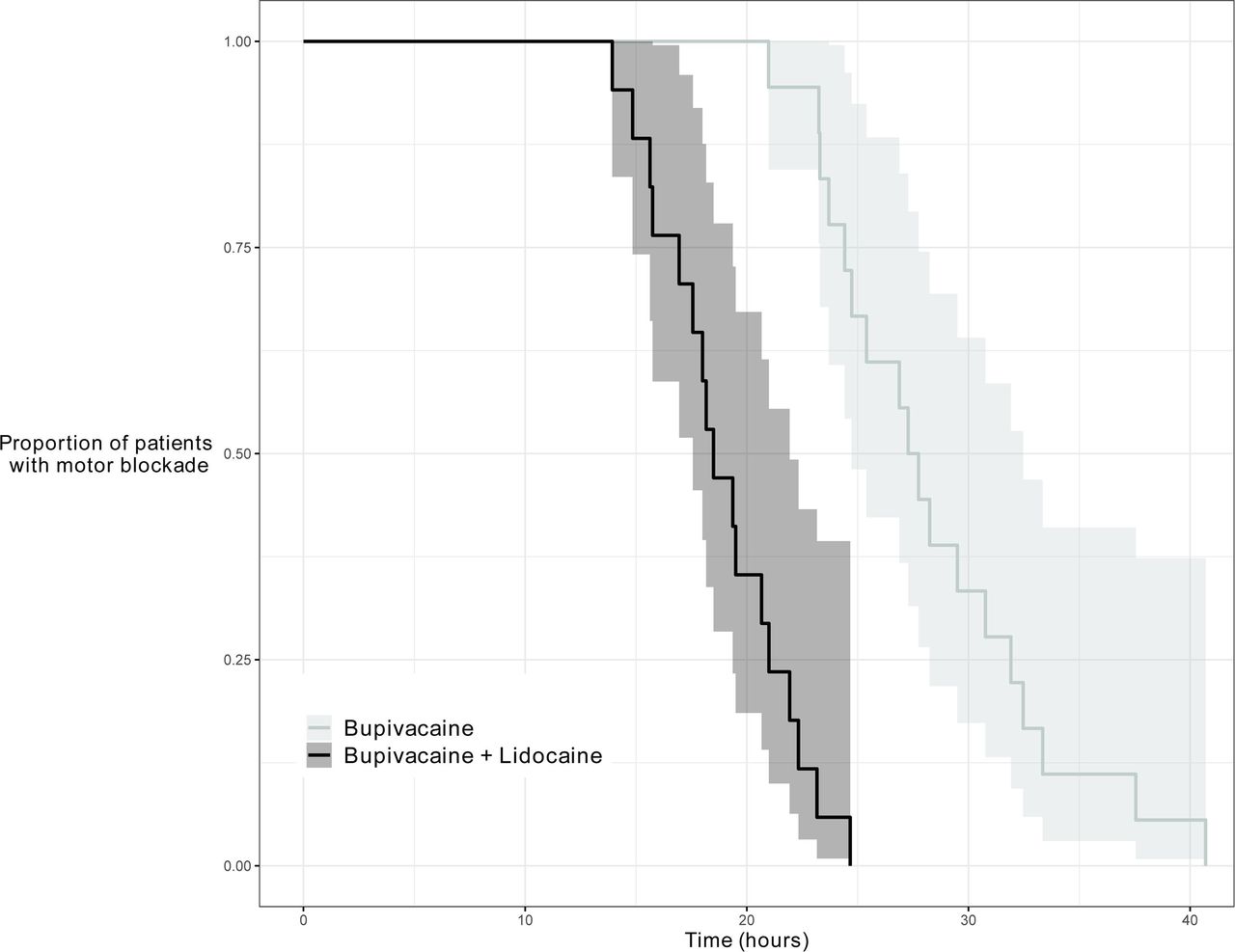
Kaplan-Meier survival plot for the duration of motor block. p<0.001 (log-rank test). The shading indicates the range of 95% CI for the corresponding survival curve.
Similarly, the mean sensory block duration was 29.3 hours for bupivacaine alone versus 18.7 hours for the mixture, with a mean difference of 10.6 hours.
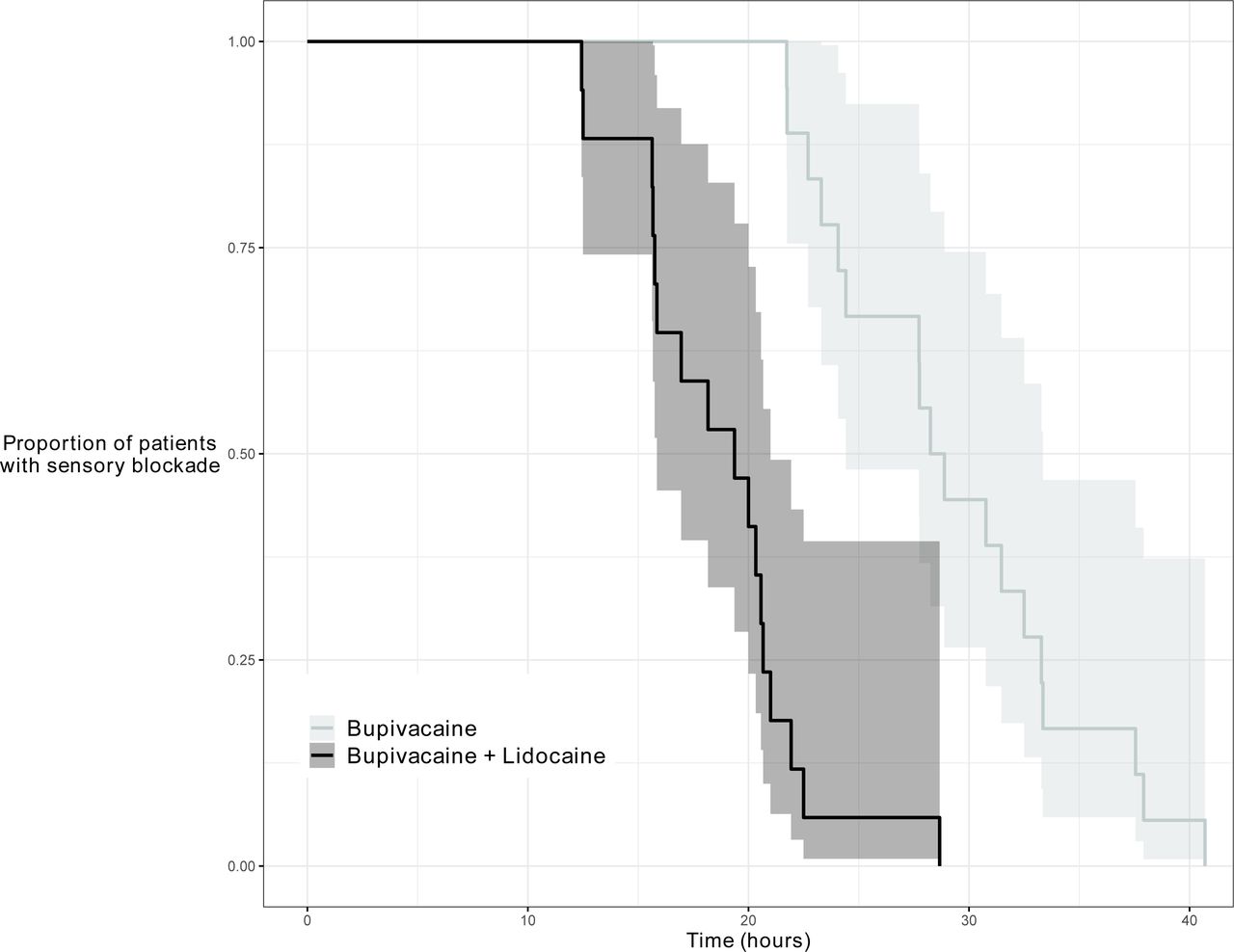
Kaplan-Meier survival plot for the duration of sensory block. p<0.001 (log-rank test). The shading indicates the range of 95% CI for the corresponding survival curve.
Postoperative analgesia also lasted longer with bupivacaine alone, averaging 38.3 hours compared to 24.3 hours for the mixture, a mean difference of 14 hours.
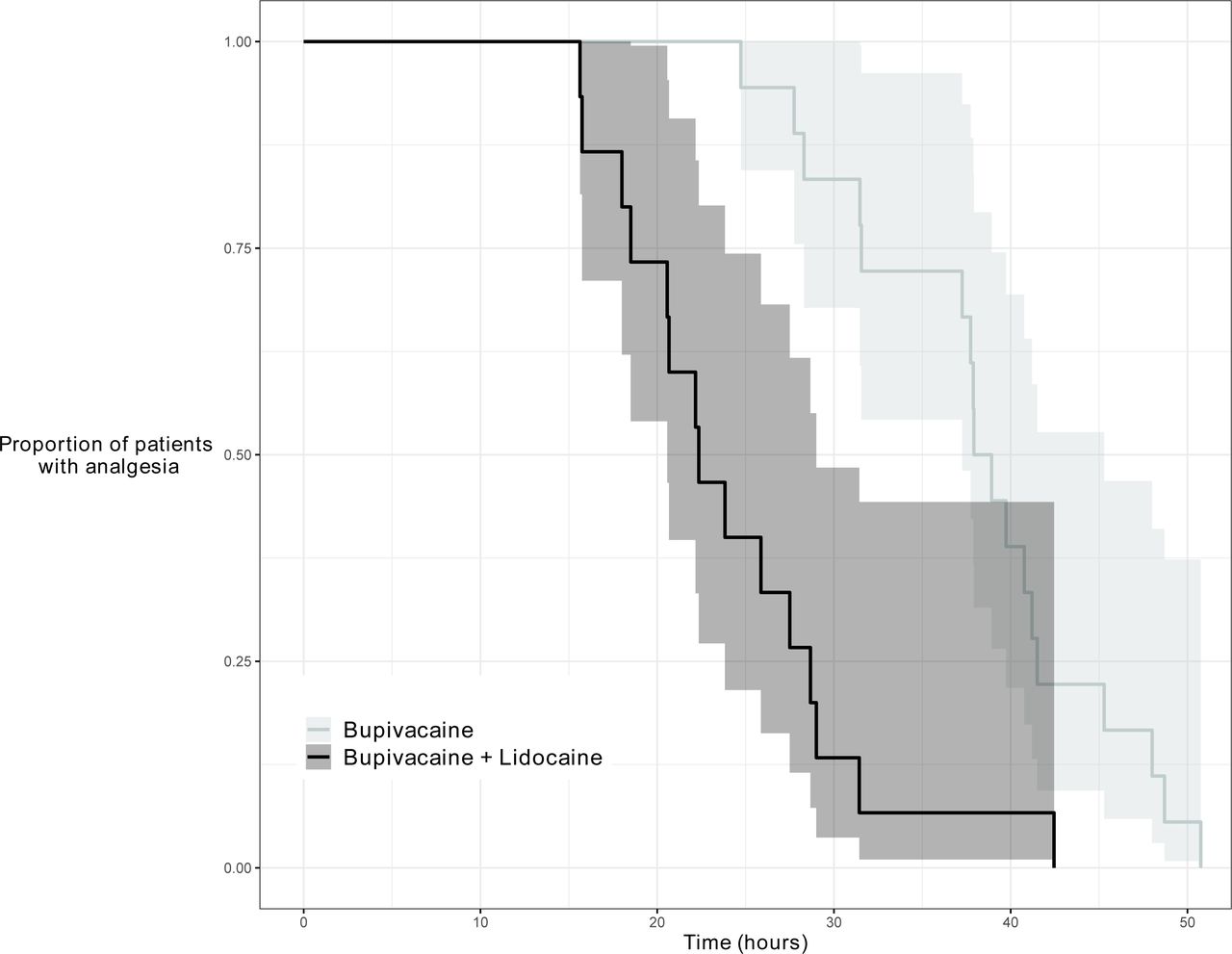
Kaplan-Meier survival plot for the duration of postoperative analgesia. p<0.001 (log-rank test). The shading indicates the range of 95% CI for the corresponding survival curve.
However, the onset time was slower for bupivacaine alone, with a median onset of 35 minutes versus 20 minutes for the mixture.
The study concluded that using 0.5% bupivacaine alone significantly prolongs both motor and sensory block durations and postoperative analgesia compared to a bupivacaine-lidocaine mixture, though it results in a slower onset time. This suggests that bupivacaine alone is more suitable for surgeries requiring extended postoperative pain relief, potentially reducing the need for perineural catheters in cases where prolonged analgesia is beneficial. The findings are particularly relevant for surgeries involving general anesthesia as the primary surgical anesthetic, where extended postoperative analgesia can enhance patient comfort and recovery. Further research is recommended to explore the effects of different adjuvants, local anesthetic types and concentrations, and various brachial plexus block approaches.
To read the full paper in RAPM, copy-paste this into your Google search:
Aguilera G, Tabilo C, Jara Á, et al. 0.25% bupivacaine–1% lidocaine vs 0.5% bupivacaine for ultrasound-guided infraclavicular brachial plexus block: a randomized controlled trial. Reg Anesth Pain Med. Published Online First: 16 May 2024.
https://rapm.bmj.com/content/early/2024/05/15/rapm-2024-105511
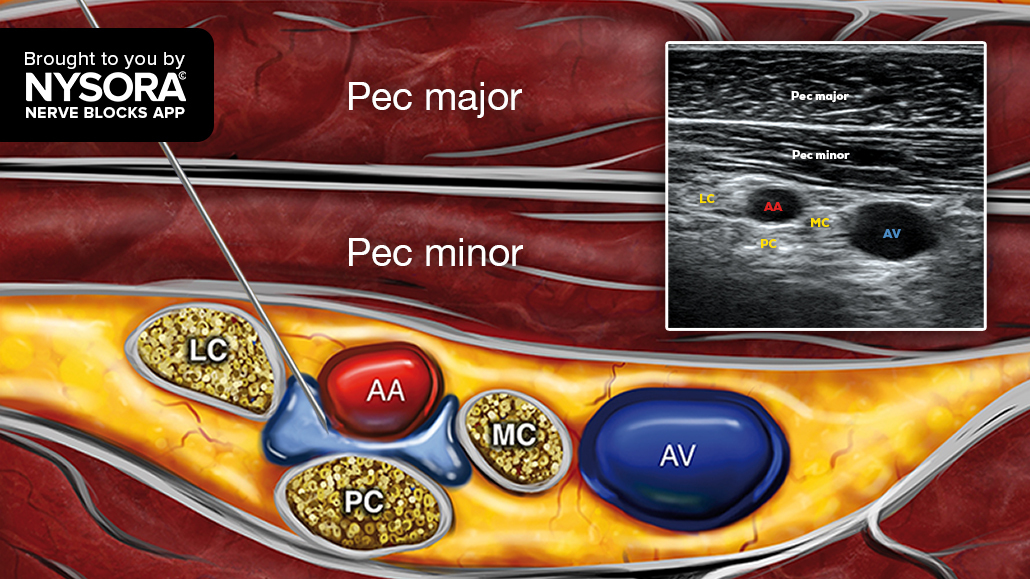
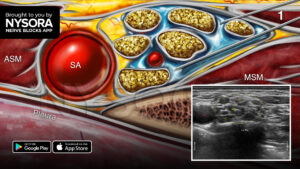
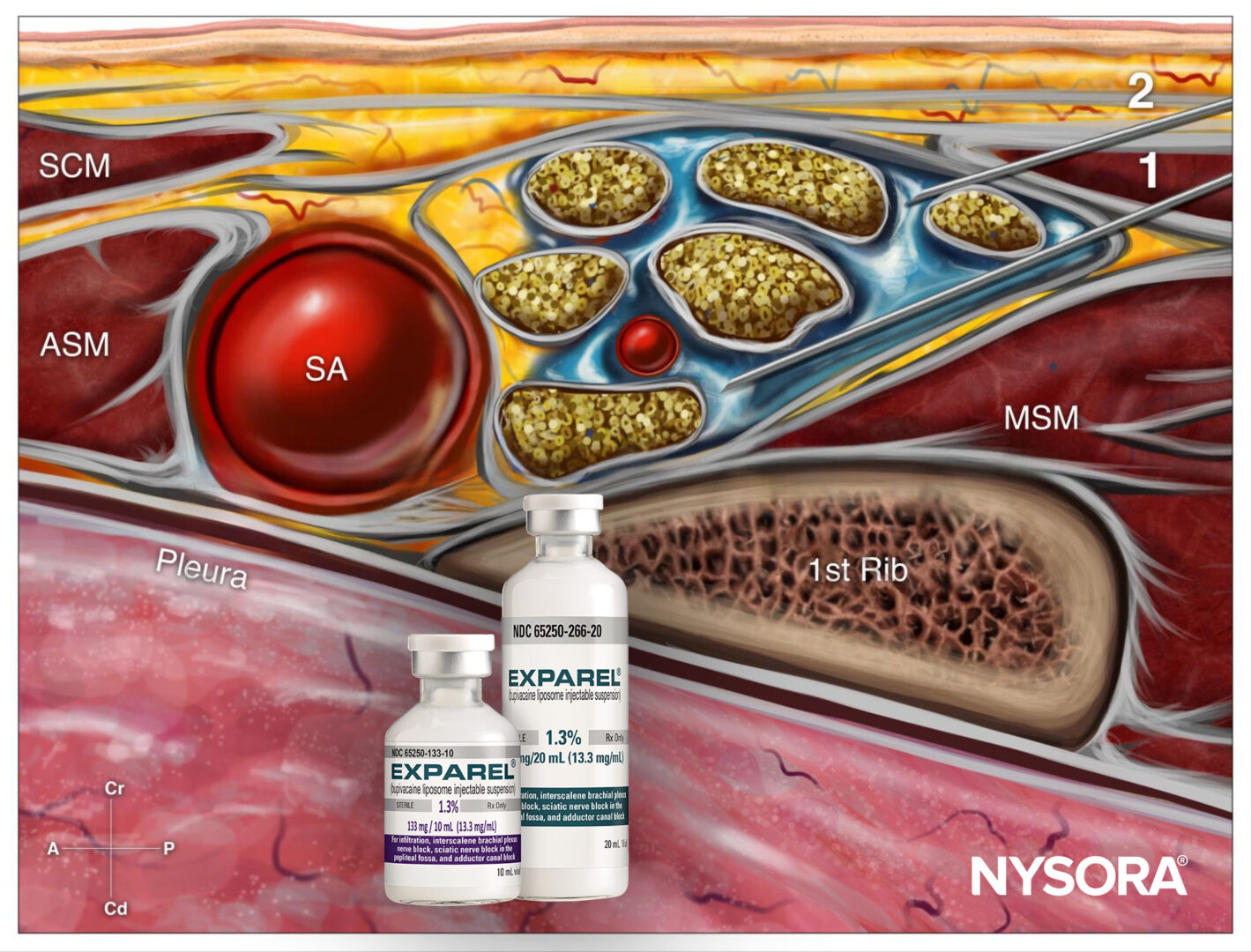
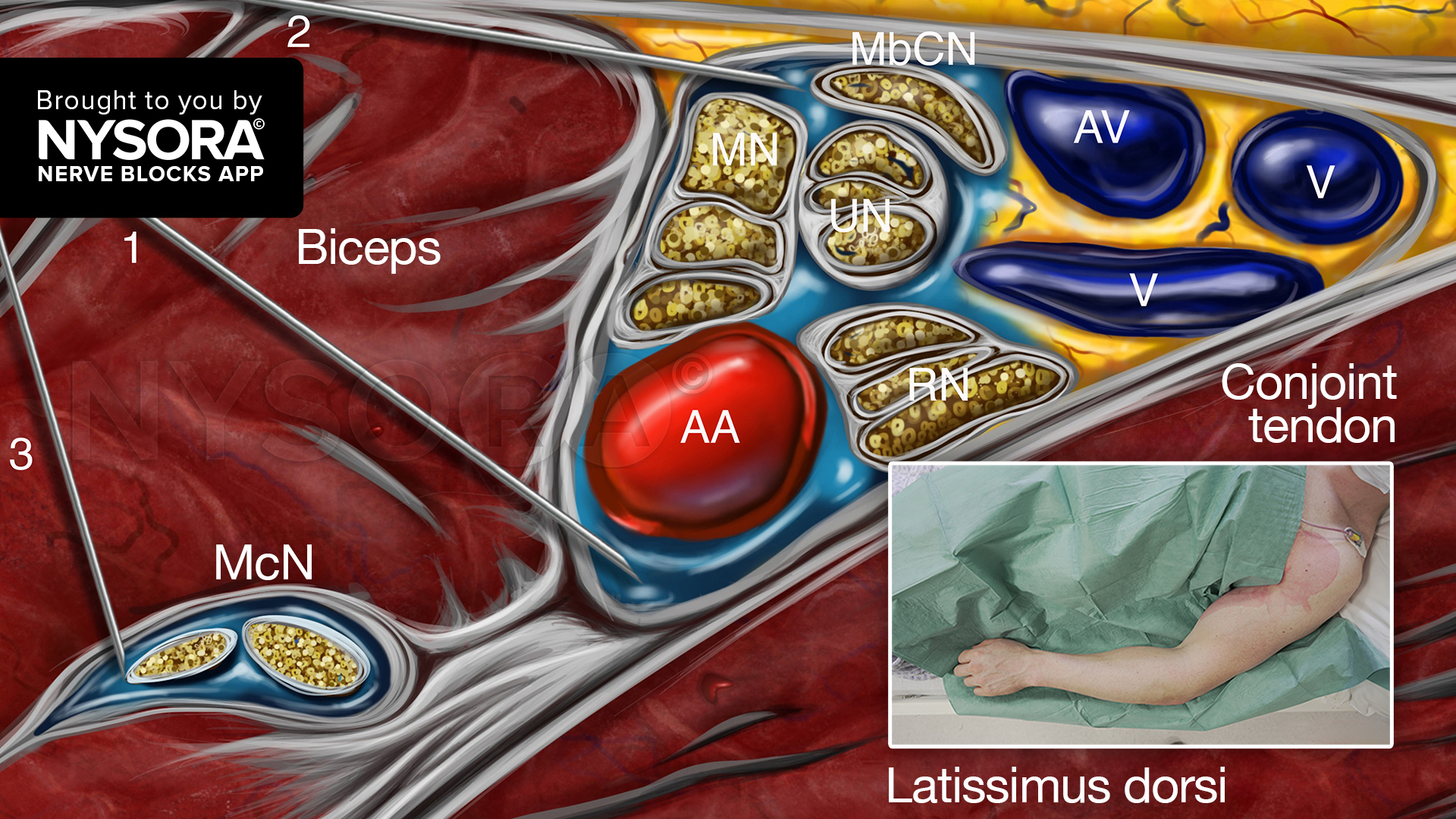
For more information on the infraclavicular brachial plexus block and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App in book format – the perfect study companion with the Nerve Blocks app!