Biceps tendon rupture completed under an axillary brachial plexus block
Case presentation
A 41-year-old man presented persistent left shoulder pain, weakness, and limited range of motion, especially during elbow flexion, linked to overuse and repetitive lifting at work. Despite conservative treatments like physical therapy and pain medications, his symptoms persisted, impacting daily life. The patient was diagnosed with a chronic, complete rupture of the long head of the biceps tendon at its insertion in the bicipital groove (distal biceps tendon rupture). Elective surgical repair was planned due to the injury’s chronic nature and the patient’s preference. An ultrasound-guided axillary brachial plexus block was scheduled for effective pain control during and after surgery.
Nerve block technique
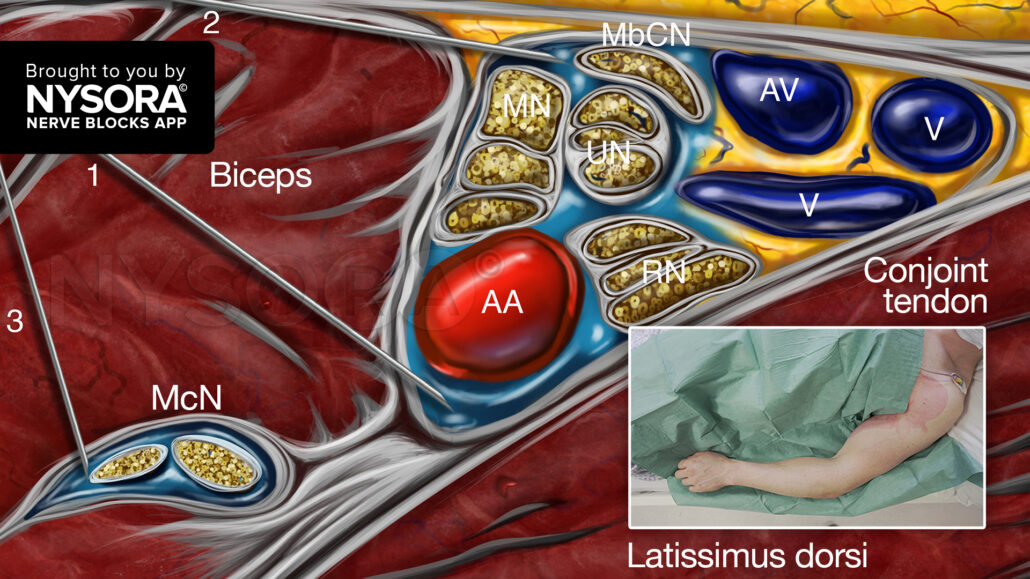
The patient was positioned in a supine manner with the left arm abducted and externally rotated to optimize access to the axillary region. Subsequently, a high-frequency linear ultrasound transducer was used to visualize the axillary artery and vein in the transverse plane. The axillary brachial plexus, comprising the radial, median, and ulnar nerves, and the musculocutaneous nerve, were identified by utilizing proximal-distal movements. Under ultrasound guidance, a 22-gauge, 50 mm needle was inserted in-plane to inject 20 mL of 0.5% ropivacaine.
- 8 mL below the axillary artery.
- 8 mL above the axillary artery.
- 4 mL for the musculocutaneous nerve, essential for this surgery to allow relaxation of the biceps muscle.
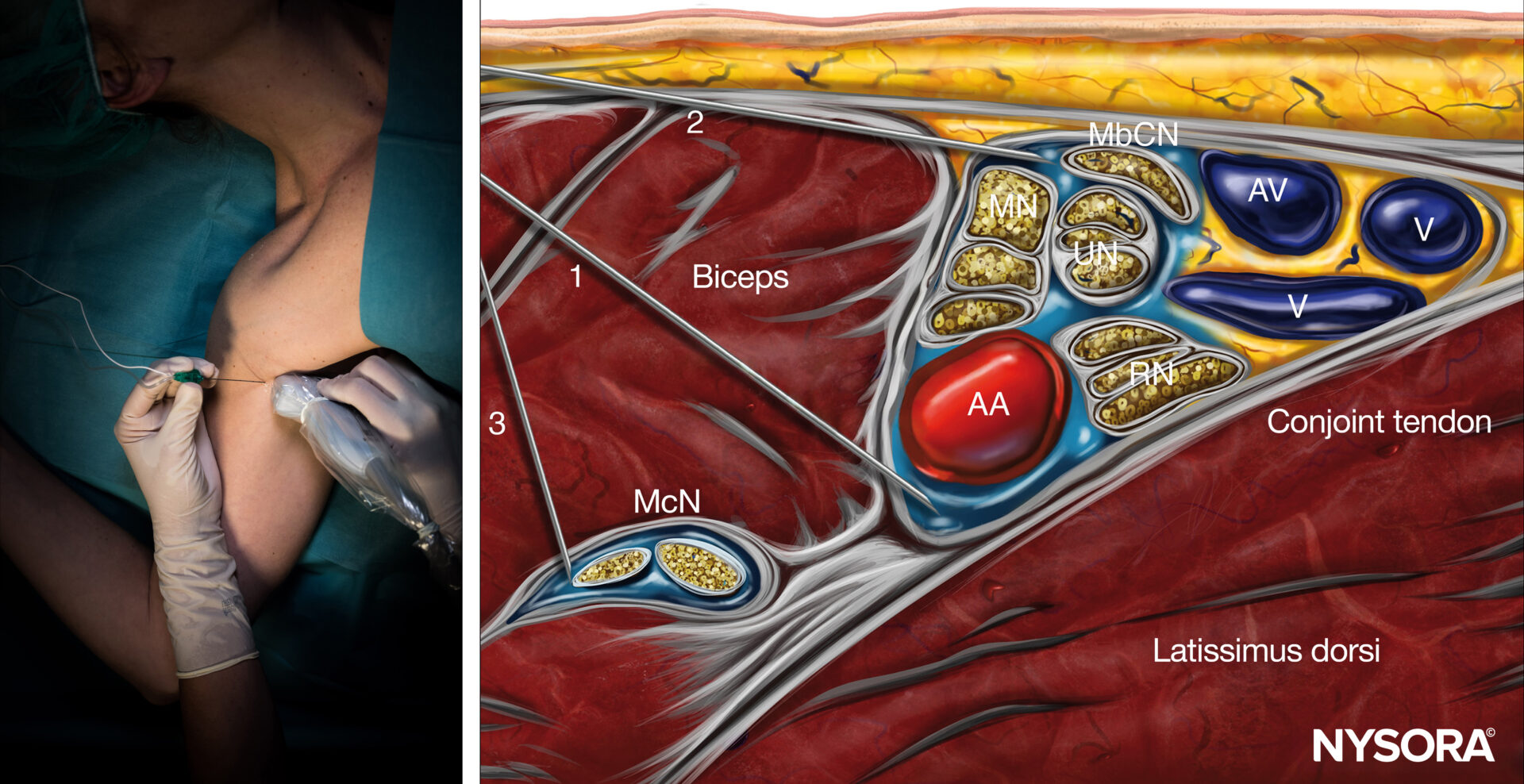
Axillary brachial plexus block; Reverse Ultrasound Anatomy with needle insertion in-plane and local anesthetic spread (blue). AA, axillary artery; AV, axillary vein; McN, musculocutaneous nerve; MN, median nerve; UN, ulnar nerve; RN, radial nerve; MbCN, medial brachial cutaneous nerve.
Patient outcome
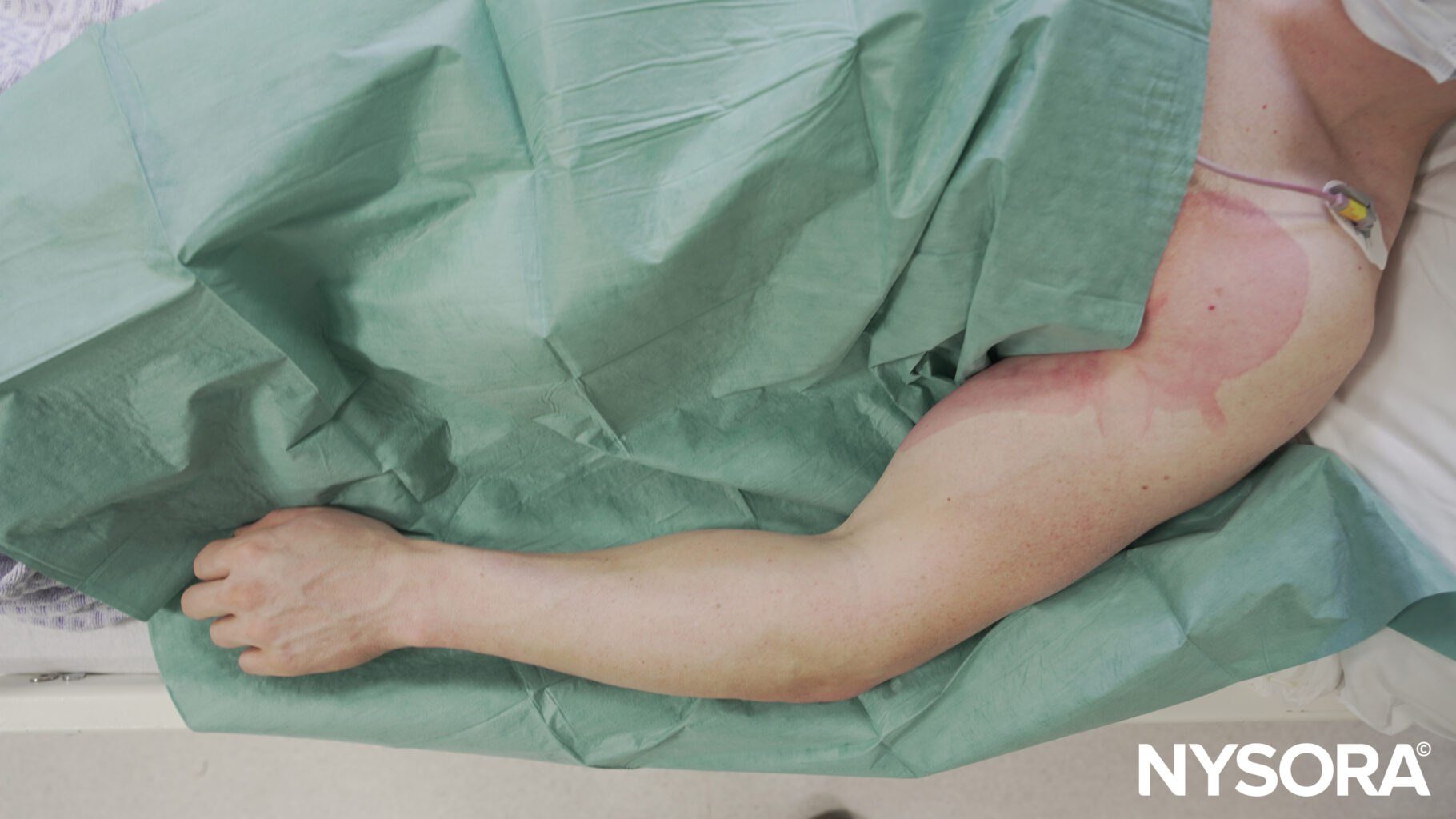
The axillary brachial plexus block provided excellent intraoperative and postoperative analgesia. The surgical procedure, which involved reattaching the ruptured biceps tendon to its anatomical insertion, proceeded seamlessly without any complications. The patient began a structured rehabilitation program under the guidance of a physical therapist to gradually restore function to the shoulder and elbow.
Clinical effectiveness of intravenous dexamethasone to enhance the axillary brachial plexus block
The ADEXA trial by Clement et al. 2019 investigated the role of intravenous dexamethasone in prolonging the analgesic effects of axillary brachial plexus block (APB) when combined with ropivacaine. This placebo-controlled, randomized, and double-blinded trial provided robust evidence on dexamethasone’s impact on postoperative pain management.
Key highlights
Objective:
To assess whether intravenous dexamethasone enhances the duration of analgesia in APB administered with ropivacaine.
Design:
- Prospective, randomized, double-blind, placebo-controlled.
- Conducted at a single university hospital in compliance with the Declaration of Helsinki.
Population:
- Ninety-eight patients scheduled for hand or forearm surgeries under APB were included.
- Randomization allocated patients to either dexamethasone (8 mg/2 mL) or saline (control).
Methodology
- Anesthesia protocol: APB was performed under ultrasound and nerve stimulation guidance using 0.5 mL/kg of 0.475% ropivacaine.
- Drug administration: A blinded injection of either dexamethasone or saline was administered intravenously.
- Monitoring: Postoperative pain, and motor and sensory recovery were recorded, along with analgesic intake.
Primary outcome:
- Time to first analgesic intake after APB.
Secondary outcomes:
- Duration of motor and sensory recovery.
- Analgesic consumption during the first 48 hours.
- Blood glucose levels postoperatively.
Results
- Extended analgesia duration:
- Patients receiving dexamethasone experienced a significantly longer time to first analgesic intake (20.9 ± 9.3 hours) compared to the control group (14.7 ± 6.6 hours, p < 0.0004).
- Reduced postoperative analgesic use:
- Fewer patients in the dexamethasone group required rescue analgesics like paracetamol, ketoprofen, and tramadol.
- Delayed motor and sensory recovery:
- Sensory recovery occurred at 18.0 ± 5.1 hours in the dexamethasone group versus 14.7 ± 4.8 hours in controls.
- Safety profile:
- No significant nerve-related complications were reported.
- A moderate increase in blood glucose levels was observed but remained clinically insignificant.
- Long-term outcomes:
- Follow-up at six months showed no significant adverse effects, reinforcing dexamethasone’s safety.
Clinical implications
- Clinical utility: Intravenous dexamethasone effectively enhances the duration of analgesia, offering a practical alternative to perineural administration.
- Patient comfort: Delayed pain onset improves the perioperative experience and reduces dependency on postoperative opioids.
- Cost efficiency: Prolonged analgesia with reduced medication requirements may lower healthcare costs.
Study limitations
- Generalizability: The study’s findings are specific to ropivacaine and may not directly apply to other anesthetics.
- Dosing precision: Fixed dexamethasone dosage may not account for individual variability; further research is warranted for weight-adjusted dosing.
- Surgical scope: Focus on hand and forearm surgeries limits applicability to other procedures.
Conclusion
The ADEXA trial substantiates the efficacy of intravenous dexamethasone as an adjunct in regional anesthesia for prolonging the effects of ropivacaine in APB. This finding is particularly relevant for patients undergoing upper limb surgeries, offering an effective, safe, and convenient option for postoperative pain management.
For the full article, refer to Regional Anesthesia & Pain Medicine.
Clement JC, Besch G, Puyraveau M, Grelet T, Ferreira D, Vettoretti L, Pili-Floury S, Samain E, Berthier F. Clinical effectiveness of single dose of intravenous dexamethasone on the duration of ropivacaine axillary brachial plexus block: the randomized placebo-controlled ADEXA trial. Reg Anesth Pain Med. 2019 Mar;44(3):e100035.
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!