Case study: Carotid endarterectomy completed under a cervical plexus block
Case description
A 70-year-old female patient received a diagnosis of severe stenosis of the right internal carotid artery, necessitating a carotid endarterectomy to remove the atherosclerotic plaque. Due to her age and history of stroke, the surgical team opted for regional anesthesia to facilitate neurological monitoring throughout the procedure.
Nerve block technique
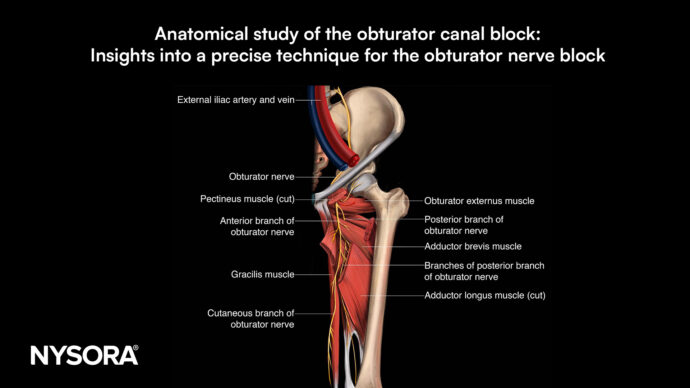
The patient was positioned supine with the neck slightly extended and rotated away from the side to be blocked. Using a high-frequency linear ultrasound transducer, the cervical plexus was visualized along the posterior border of the sternocleidomastoid muscle. Under ultrasound guidance, a 22-gauge, 50 mm needle was inserted in-plane. After negative aspiration and confirming correct needle placement, 10 mL of 0.25% bupivacaine was injected incrementally around the cervical plexus, while monitoring for signs of intravascular or intrathecal injection.
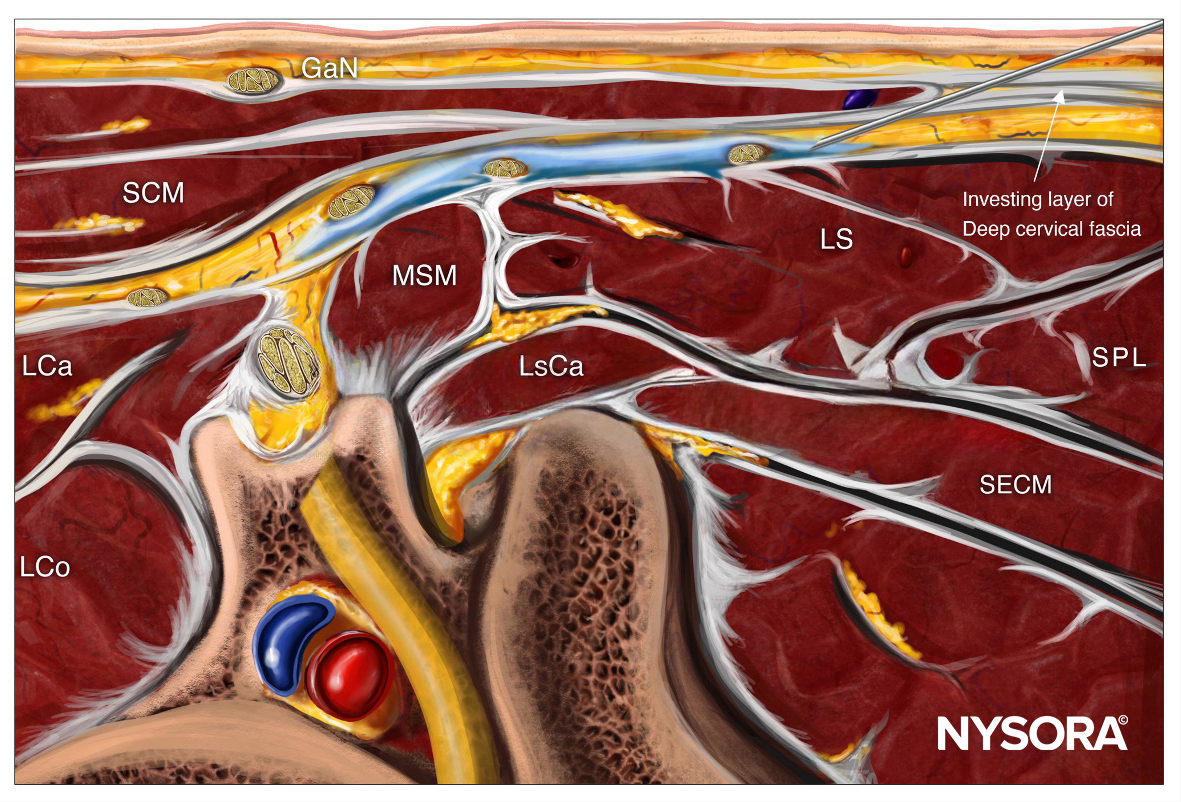
Reverse Ultrasound Anatomy for a cervical plexus block with needle insertion in-plane and local anesthetic spread (blue). GaN, greater auricular nerve; SCM, sternocleidomastoid muscle; LCa, longus capitis muscle, LCo, longus colli muscle; MSM, middle scalene muscle; LsCa, longissimus capitis muscle; LS, levator scapulae muscle; SPL, splenius capitis muscle; SECM, semispinalis capitis muscle.
Patient outcome
The carotid endarterectomy was completed under the cervical plexus block, with the patient remaining alert and responsive throughout the surgery. Neurological monitoring during carotid artery clamping revealed no changes, underscoring the advantage of regional anesthesia. Postoperative pain was effectively controlled, and the procedure was free from complications.
Exploring the Use of Intermediate Cervical Plexus Block in Carotid Endarterectomy: A Case Series
Introduction
Stroke is a leading cause of mortality worldwide, with carotid artery disease contributing to 10-20% of cases. Carotid endarterectomy is the recommended treatment for symptomatic patients with significant carotid stenosis to prevent embolic strokes. Traditionally, this procedure is carried out under general anesthesia or deep cervical plexus block (DCPB), both of which have their own set of complications. However, a recent case series by Ratnayake et al. 2024 highlights the potential of intermediate cervical plexus block (ICPB) combined with superficial cervical plexus block (SCPB) as a safer and more effective alternative.
Materials and Methods
- This case series involved five patients with symptomatic carotid stenosis who underwent carotid endarterectomy between June 2023 and March 2024.
- All patients were classified as American Society of Anesthesiologists (ASA) class 2, indicating the presence of well-controlled comorbidities.
- The patients were administered a combination of SCPB and ICPB using 2% lignocaine and 0.5% plain bupivacaine.
- The SCPB was performed first, followed by the ICPB, both under ultrasound guidance.
- Surgeries were initiated 10-20 minutes after the completion of the blocks.
- The patients’ higher neurological functions were assessed using predefined memory, speech, and motor function tests throughout the procedure.
Results
- Adequate anesthesia was achieved in four out of five patients. One patient required additional local anesthetic infiltration.
- Two patients experienced hoarseness of voice postoperatively, which resolved within two hours. Hemodynamic fluctuations were observed in all patients, but these were managed effectively without serious complications.
- All five patients had uneventful recoveries and were discharged from the high dependency unit (HDU) within 24 hours post-surgery.
Discussion
The case series highlights several advantages of using ICPB in combination with SCPB for CEA:
- The ICPB is easier to perform compared to DCPB, requiring fewer injections and posing less risk of severe complications such as intravascular or epidural injections.
- The ICPB avoids the complications associated with DCPB, such as phrenic nerve palsy and accidental puncture of major vessels. This makes it a safer option, particularly in patients who are at higher risk for complications under GA or DCPB.
- The combination of SCPB and ICPB provides sufficient anesthesia for the duration of the surgery, as evidenced by the minimal need for supplemental anesthesia in the case series.
However, the study also points out the need for further research:
- While hemodynamic changes were observed in all patients, the significance of these fluctuations compared to those under GA remains unclear. A randomized controlled trial would be beneficial in determining whether these changes have clinical implications.
- Further studies are needed to evaluate the long-term outcomes of patients undergoing CEA under ICPB compared to those under DCPB or GA.
Conclusion
The findings of this case series suggest that the combination of SCPB and ICPB is a viable and potentially safer alternative to DCPB for CEA. It provides adequate anesthesia, is easier to perform, and is associated with fewer complications. While further research is necessary to confirm these findings and explore the long-term outcomes, the use of ICPB in CEA represents a promising advancement in regional anesthesia techniques.
For more detailed information, refer to the full article in BMC Anesthesiology.
Ratnayake A, Abeysundara A, Samarasinghe B, et al. Use of intermediate cervical plexus block in carotid endarterectomy -an alternative to deep cervical plexus block: a case series. BMC Anesthesiol. 2024;24(1):288.
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App in book format – the perfect study companion with the Nerve Blocks app!