Case study: Upper limb complex regional pain syndrome (CRPS)
Case study: Upper limb complex regional pain syndrome (CRPS)
Complex Regional Pain Syndrome (CRPS) is a challenging and often debilitating condition characterized by prolonged pain and inflammation following injury. This case study highlights a multidisciplinary approach to diagnosing and managing CRPS in a patient with a history of trauma. Focusing on the innovative use of stellate ganglion blocks and an oblique fluoroscopic approach, this article provides an in-depth understanding of the techniques and outcomes.
Case presentation
Patient profile:
- Age: 59 years
- Gender: Male
- History: Left wrist fracture following a traffic accident, complicated by infection and neuropathic pain.
Key medical history
- Comorbidities: Coeliac disease.
- Injury: Left wrist fracture treated with surgical fixation.
- Complications: Wound infection requiring debridement and persistent neuropathic pain.
Symptoms
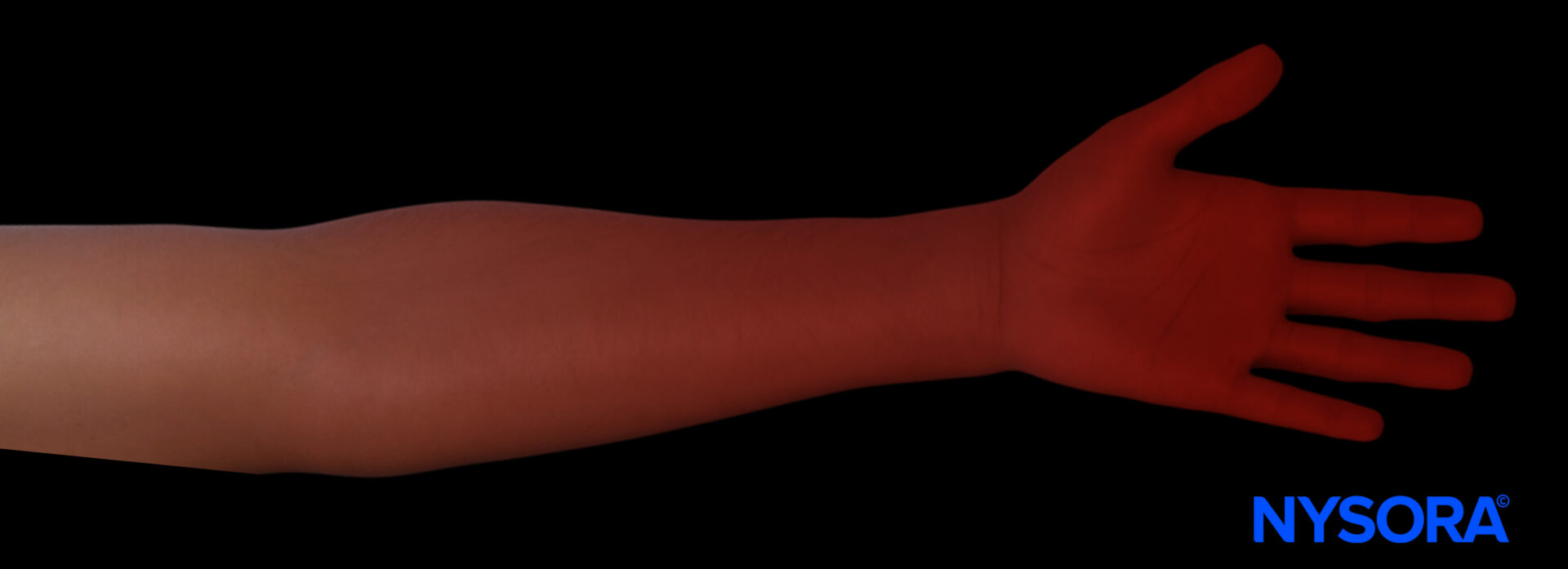
- Persistent left-hand pain radiating to the forearm and arm.
- Pain exacerbation with intermittent swelling and discoloration.
- Neuropathic pain with allodynia (pain from non-painful stimuli).
- Pain scores: Baseline NRS 5, peaking at 8.
Physical examination
- Mild trophic changes and erythema of the left hand.
- No dystonia or overt motor deficits.
- Blood tests: No leukocytosis or elevated inflammatory markers.
Diagnosis
Complex Regional Pain Syndrome (CRPS) of the left upper limb.
Key diagnostic features (Budapest criteria):
- Persistent pain disproportionate to the initial injury.
- Sensory changes: Allodynia and hyperalgesia.
- Vasomotor dysfunction: Intermittent swelling and discoloration.
- Exclusion of alternative diagnoses via clinical evaluation and imaging.
Understanding CRPS
What is CRPS?
CRPS is a chronic pain condition typically triggered by trauma or nerve injury. It involves:
- Excessive pain and inflammation.
- Changes in skin color, temperature, and texture.
- Joint stiffness and impaired mobility.
Pathophysiology
The exact cause of CRPS is unclear but may involve:
- Peripheral and central nervous system sensitization.
- Dysregulated inflammatory responses.
Treatment overview
A multidisciplinary approach is crucial for managing CRPS.
Pharmacological management
- Pregabalin: 75 mg twice daily for neuropathic pain.
- Amitriptyline: 25 mg nightly to address both pain and sleep disturbances.
- Intravenous ketamine infusion: Administered for acute pain relief.
Non-pharmacological strategies
- Graded motor imagery: Retraining the brain’s pain perception.
- Physiotherapy: Maintaining mobility and reducing stiffness.
- Mental health support: Addressing comorbid PTSD through counseling and psychotherapy.
Interventional techniques
- Stellate ganglion block (SGB): Performed using the oblique fluoroscopic approach for targeted pain relief.
Stellate Ganglion Block
The stellate ganglion block targets the cervical sympathetic chain to reduce pain and inflammation in CRPS and PTSD.
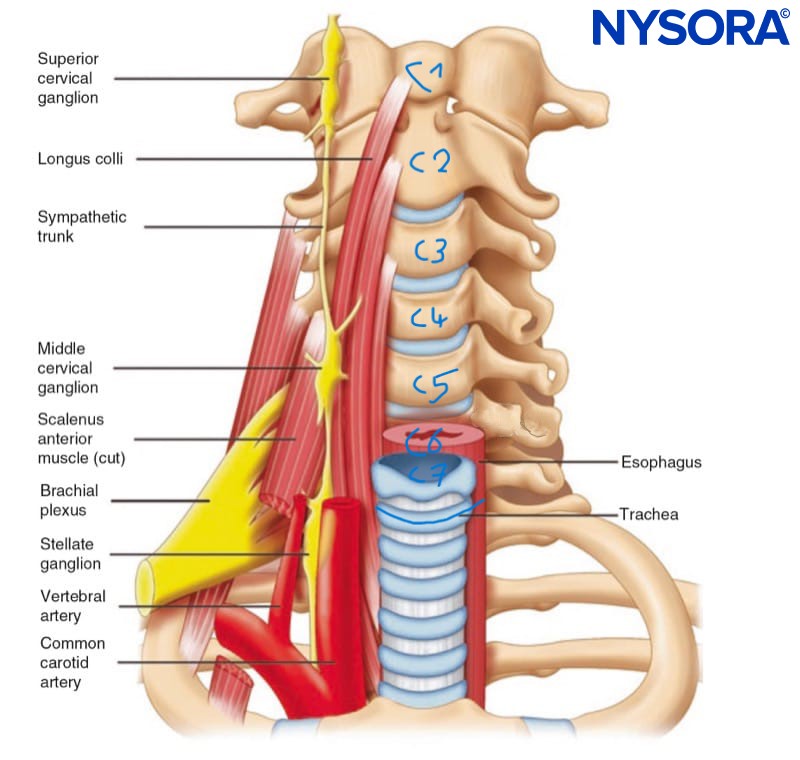
Anatomy
- The stellate ganglion comprises the inferior cervical ganglion and the first thoracic ganglion, located near the C7 vertebral body.
- It lies anterior to the transverse processes and prevertebral fascia, superior to the subclavian artery.
Indications
- CRPS of the upper limb.
- Post-traumatic stress disorder (PTSD).
Technique: Oblique fluoroscopic approach
- Patient preparation
- Position: Supine with the neck in a neutral or 20° contralateral tilt.
- Monitoring: ECG, blood pressure, and pulse oximetry.
- Premedication: Local infiltration with 1% lidocaine, optional IV sedation for anxious patients.
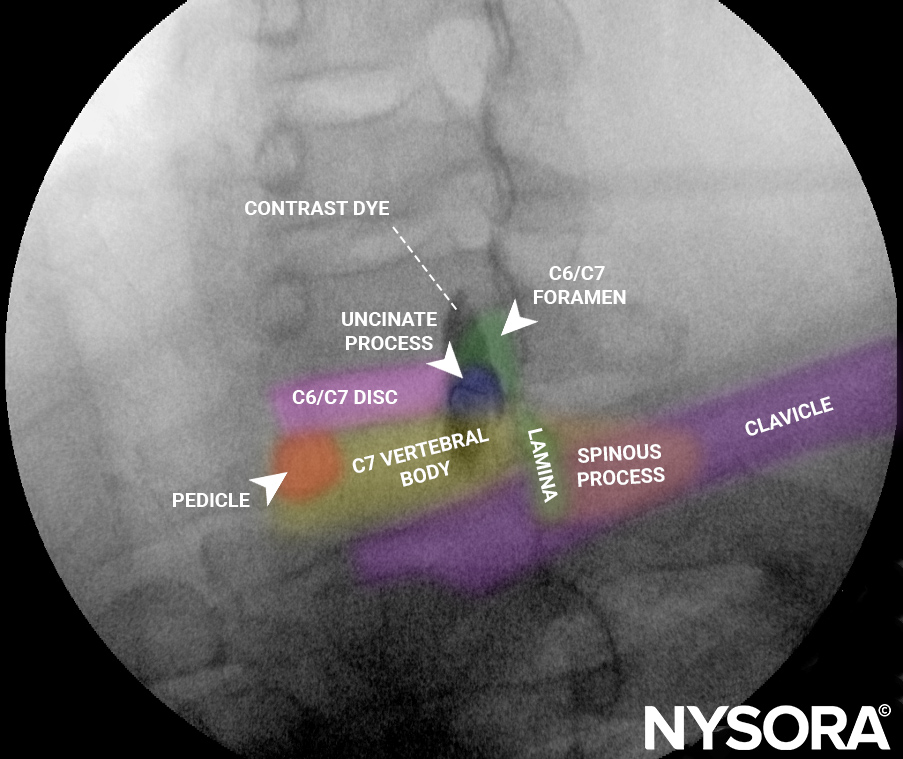
- Fluoroscopic imaging
- AP View: Identify the cervical spine.
- Oblique View: Angle the fluoroscope at 30-45° to visualize the uncinate process of the C6 or C7 vertebral body.
- Needle insertion
- Insert a 22-gauge, 90 mm Quincke needle under fluoroscopic guidance using a co-axial (tunnel vision) approach.
- Verify needle position with 0.5-1 mL of contrast dye (Omnipaque 300) to confirm safe placement.
- Administer 5-8 mL of 1% ropivacaine for the block.
- Confirmation
- Ensure contrast spread under fluoroscopy to the T1 level.
- Presence of Horner’s syndrome (e.g., ptosis, miosis) confirms block success.
Advantages of the oblique approach
- Avoids esophageal injury and eliminates the need for carotid artery displacement.
- Effective at targeting the stellate ganglion with smaller volumes of injectate.
- Minimizes risks of recurrent laryngeal nerve block.
Patient outcomes
- Immediate Relief: 70% pain reduction one hour post-procedure.
- Sustained Pain Relief: Lasted 3-4 months after subsequent SGB and ketamine infusions.
- Functional Improvement: Pain-free on hospital discharge with no complications.
- PTSD Relief: Secondary SGB performed with a positive response.
Tips for success
- Use the oblique approach to improve patient comfort and safety.
- Combine SGB with multidisciplinary pain management strategies for optimal outcomes.
- Monitor for complications such as hoarseness or vascular injury.
Conclusion
This case demonstrates the effectiveness of combining pharmacological, non-pharmacological, and interventional therapies in managing upper limb CRPS. The stellate ganglion block using the oblique fluoroscopic approach is a pivotal tool for providing targeted pain relief and improving quality of life in patients with CRPS and associated PTSD.
Read more about the treatment, patient outcome, and other case studies in the Pain Rx App. Click HERE and get the ultimate app for fluoroscopy-guided pain treatments.