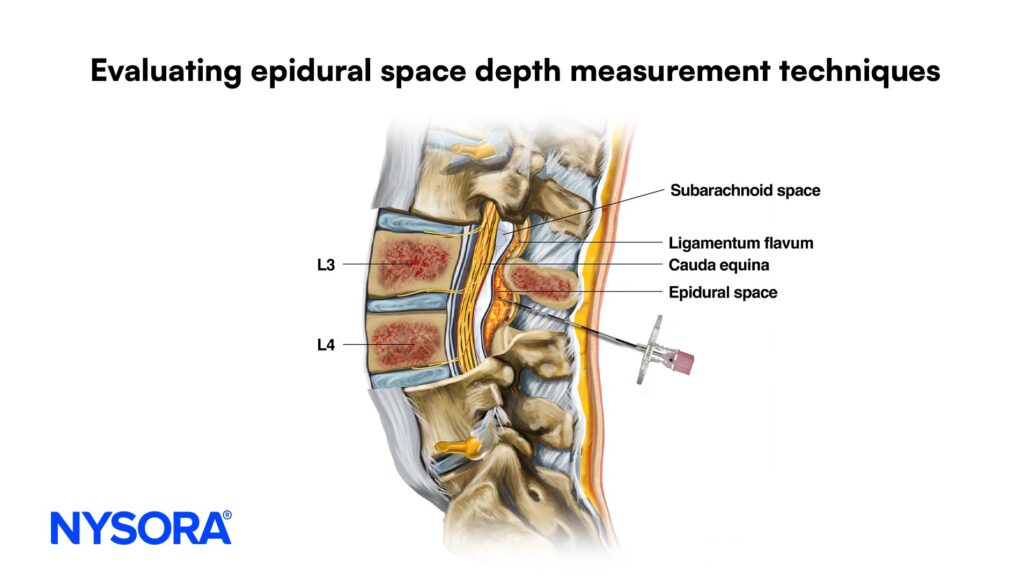
Evaluating Epidural Space Depth Measurement Techniques
Accurate measurement of the epidural space depth is crucial for the success and safety of lumbar epidural steroid injections (ESIs), a widely used procedure to manage radicular pain. A recent study by Singh et al., published in Regional Anesthesia and Pain Medicine, evaluates the effectiveness of ultrasound (US) and magnetic resonance imaging (MRI) as pre-procedural tools to predict the clinical loss of resistance depth (CLORD). This analysis highlights significant findings that could influence clinical practices in pain management.
Study design
- Participants:
- 60 patients undergoing lumbar ESIs were studied.
- Inclusion criteria included patients aged 18+ with recent lumbar MRI available.
- Exclusion criteria included pregnancy, poor-quality MRI, and non-midline injection approaches.
- Methods
- Measurements of the epidural space depth were taken using:
- MRI: Sagittal T2-weighted images.
- US: Transverse and parasagittal oblique views.
- Clinical loss of resistance Technique: The standard procedure for determining CLORD during injections.
- The results were statistically analyzed for equivalency, correlation, and reliability.
- Measurements of the epidural space depth were taken using:
Key findings
- MRI accuracy:
- MRI measurements closely matched CLORD, with a mean difference of –0.2 cm and an intraclass correlation coefficient of 0.85.
- MRI demonstrated higher accuracy and reliability than ultrasound, making it the preferred modality for pre-procedural planning.
- Ultrasound limitations:
- Transverse and parasagittal oblique US measurements underestimated CLORD, with mean differences of –0.98 cm and –0.79 cm, respectively.
- Variations in accuracy were more pronounced in patients with a body mass index (BMI) >30, where US measurements were less reliable.
- Clinical implications:
- While MRI provides precise preoperative assessment, its availability and cost limit its routine use in all clinical settings.
- Ultrasound, though less accurate, remains a practical, point-of-care option, particularly when MRI is unavailable.
Practical recommendations
- Use MRI as the gold standard for pre-procedural assessment when available.
- In settings without MRI access, employ US with an understanding of its limitations, particularly in patients with higher BMI.
- Focus on parasagittal oblique views over transverse US views for more reliable results.
Step-by-step guide for clinicians
- Pre-procedural assessment:
- Review the patient’s medical history and imaging (MRI or US).
- Ensure accurate identification of lumbar levels.
- Imaging protocol:
- For MRI: Obtain sagittal T2-weighted images.
- For US: Use curvilinear probes with transverse and parasagittal oblique orientations.
- CLORD measurement:
- Position the patient prone.
- Mark the lumbar level using fluoroscopy before US measurements.
- Use the clinical loss of resistance technique during needle insertion.
- Procedure:
- Use imaging guidance to minimize risk.
- Confirm the needle’s position with contrast dye if needed.
Conclusions and future directions
This study underscores the importance of accurate imaging techniques in predicting the depth of the epidural space. While MRI offers superior precision, the practicality of ultrasound ensures its continued relevance in clinical practice. Future research should focus on expanding these findings to other anatomical regions and patient populations, including those undergoing thoracic or cervical ESIs and obstetric anesthesia procedures.
By leveraging the strengths of each modality, clinicians can enhance procedural safety and efficacy, paving the way for improved patient outcomes in pain management.
For more detailed information, refer to the full article in RAPM.
Stay up to date with the latest advances in pain medicine with Pain Medicine Updates 2025, a concise, expertly curated resource designed to deliver actionable insights and streamline your clinical practice.