Extravascular Injection of Neuromuscular Blocking Agents: Understanding Risks and Management
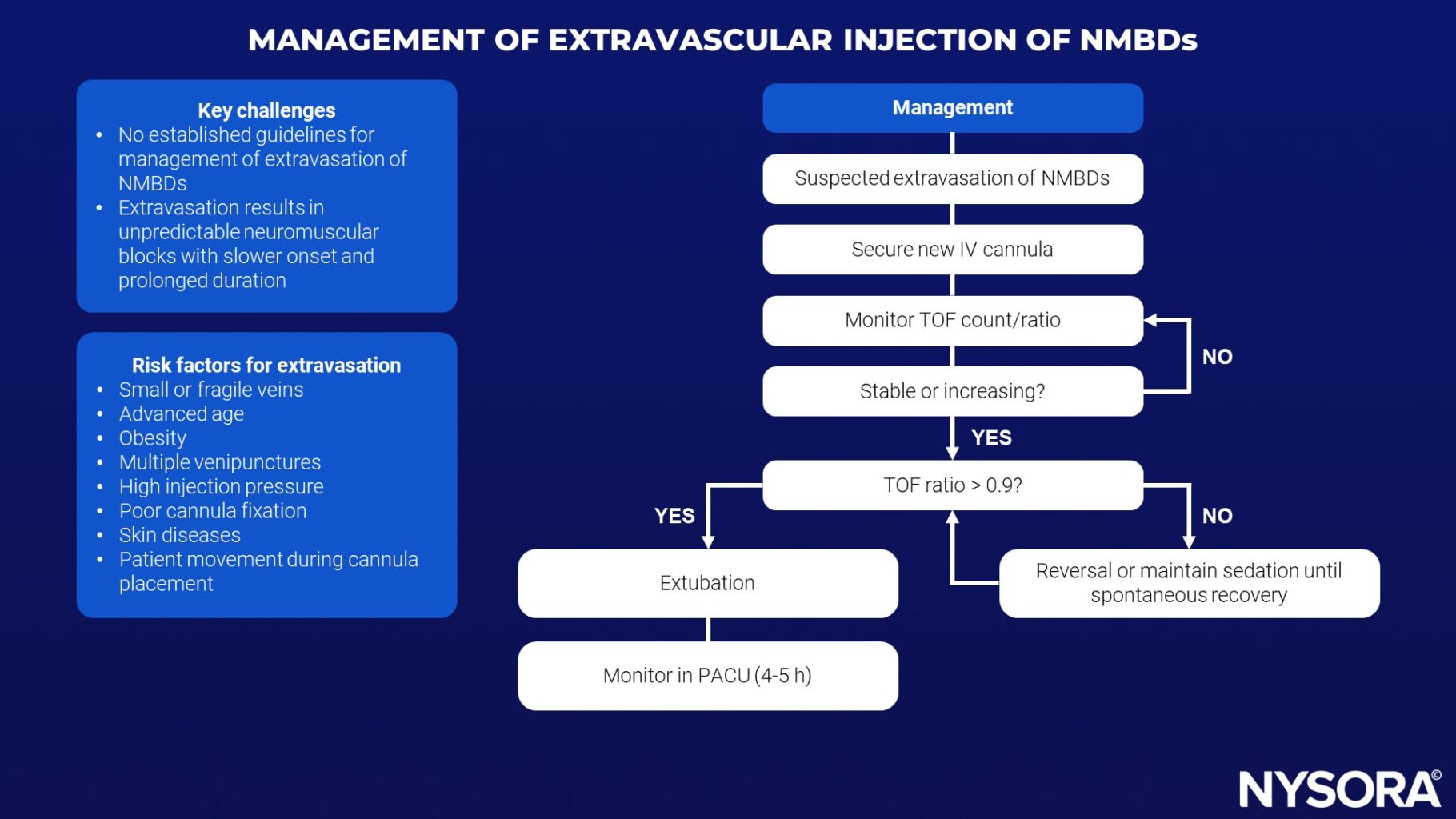
Neuromuscular blocking drugs (NMBDs) are typically administered intravenously to facilitate muscle relaxation during surgical procedures. However, accidental extravasation (injection outside the vein) can occur, leading to unpredictable and prolonged neuromuscular block due to the formation of a subcutaneous depot and subsequent slow systemic absorption. This article reviews the current literature on the extravasation of NMBDs and proposes a clinical pathway for managing this complication.
What happens during extravascular injection? When NMBAs are accidentally injected into tissues surrounding blood vessels instead of directly into the bloodstream, several adverse outcomes may occur:
- Prolonged Muscle Paralysis: The drug remains in the tissues longer, leading to extended muscle paralysis.
- Tissue Damage: Extravascular injection can cause local tissue necrosis, inflammation, and pain.
- Delayed Onset of Action: The effect of the drug becomes delayed and unpredictable, complicating surgical procedures.
Physiological Impact
The pharmacokinetics of NMBAs are altered during extravascular injection. These agents are designed for rapid onset and controlled duration of action when administered intravenously. When injected into muscle or subcutaneous tissue, the absorption rate slows significantly, leading to unpredictable and prolonged effects. This unpredictability can disrupt planned surgical procedures and necessitate prolonged ventilation support.
Common symptoms
Patients affected by extravascular NMBA injections may present with:
- Prolonged Muscle Weakness: This includes general muscle fatigue and inability to move limbs.
- Respiratory Distress: If respiratory muscles are involved, patients may have difficulty breathing.
- Localized Pain and Swelling: Injection sites may become painful and swollen due to inflammation or necrosis.
Risk Factors for Extravasation
- Small or fragile veins
- Advanced age
- Obesity
- Multiple venipunctures
- High injection pressure
- Poor cannula fixation
- Disseminated skin diseases
- Patient movement during cannula placement
Diagnostic approach
Diagnosis of extravascular NMBA injection is primarily clinical, supported by the patient’s symptoms and the history of NMBA administration. Key diagnostic steps include:
- Patient History: Review the administration technique and injection site.
- Physical Examination: Assess for localized swelling, tenderness, and muscle weakness.
- Neuromuscular Monitoring: Use a peripheral nerve stimulator to evaluate neuromuscular function and degree of paralysis.
Management Recommendations
- Prevention:
- Ensure correct labeling of NMBDs
- Assess intravenous line quality before administration
- Check for backflow or increased injection pressure
- Immediate Response to Extravasation:
- Secure a new intravenous line promptly
- Monitor Train-of-Four (TOF) count/ratio to assess neuromuscular block
- Monitoring and Reversal:
- Administer NMBD reversal agents (Sugammadex or Neostigmine) if TOF ratio shows improvement
- Prolonged monitoring in PACU (4-5 hours) with full ASA monitoring
- Postoperative Care:
- Extended observation in PACU for patients with long-acting NMBDs
Additional doses of reversal agents if necessary, particularly Sugammadex for aminosteroid NMBDs
Reversal Agents
Administering specific reversal agents can help counteract the effects of NMBAs. The choice of agent depends on the NMBA used:
- Neostigmine: This acetylcholinesterase inhibitor is commonly used to reverse non-depolarizing NMBAs. It increases the amount of acetylcholine at the neuromuscular junction, competing with the NMBA and reversing its effects.
- Sugammadex: This cyclodextrin compound specifically binds to rocuronium and vecuronium, forming a complex that is excreted renally. Sugammadex provides rapid and complete reversal of these agents, making it particularly useful in managing extravascular injections of rocuronium or vecuronium.
Prevention
Training and technique
To minimize the risk of extravascular NMBA injection, it is crucial to ensure proper training and technique among healthcare providers:
- Education: Regular training sessions on the correct administration of NMBAs.
- Simulation-Based Learning: Use simulation techniques to practice and perfect the injection procedure.
- Ultrasound Guidance: Employ ultrasound to visualize the injection site, ensuring accurate placement within the vascular system.
Double-checking procedures
Implementing a protocol for double-checking the injection site can further reduce the risk:
Verification: Have a second healthcare professional verify the injection site before administration.
- Site Marking: Clearly mark the intended injection site to avoid confusion and errors.
Conclusion
The extravasation of NMBDs can lead to serious complications, including delayed onset and prolonged neuromuscular block. This review highlights the importance of vigilance during NMBD administration and provides a clinical pathway to manage extravasation effectively. Further research is needed to establish comprehensive guidelines and optimize patient outcomes.
For further detailed information, please refer to the systematic review published in the European Journal of Anaesthesiology.
Nietvelt F, Van Herreweghe I, Godschalx V, Soetens F. Extravascular injection of neuromuscular blocking drugs: A systematic review of current evidence and management. European Journal of Anaesthesiology | EJA. 2024;41(5)
Want to learn more management strategies like this? Keep an eye out for our upcoming NEW book: Anesthesiology Manual: Best Practices and Case Management!