Fascial plane blocks: Understanding their microanatomy and clinical applications
In recent years, advancements in the study of fascial tissues have significantly impacted anesthesia and pain management practices. One area where these developments are particularly noteworthy is the use of fascial plane blocks (FPBs). These blocks have gained popularity due to their safety profile, ease of performance, and effectiveness in various clinical settings. This article dives into the microscopic anatomy of fasciae and the role this plays in optimizing FPBs for clinical applications.
What are fascial plane blocks?
Fascial plane blocks (FPBs) are a type of regional anesthesia that involves injecting local anesthetics (LAs) into the potential space between two fascial layers. The goal is to block the nerves that travel within or cross through these layers, providing pain relief. These blocks are highly versatile, being used for both surgical and nonsurgical procedures, particularly in areas such as the torso and extremities. Their popularity has been bolstered by the relative ease with which physicians can learn and perform them, especially with the use of modern ultrasound imaging techniques.
Fascial microanatomy
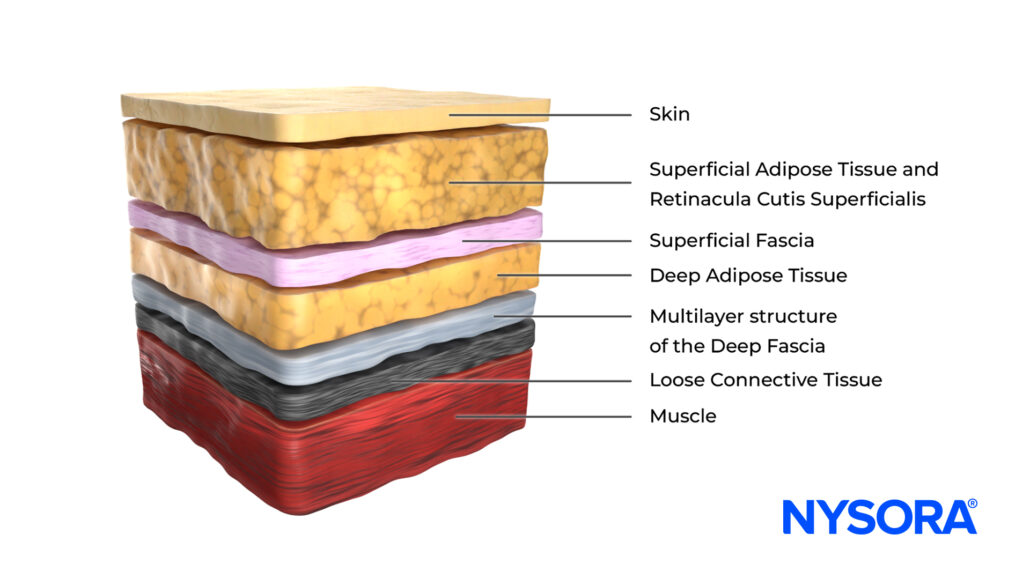
Fasciae are complex connective tissues that support and separate muscles, nerves, and other structures in the body. From a microscopic perspective, fasciae are composed of various cell types embedded within an extracellular matrix (ECM) rich in collagen and hyaluronan. This structure allows fasciae to serve as an effective medium for the spread of LAs during FPBs.
Key components of fascia
- Fibroblasts are the most abundant in fascial tissues and play a key role in maintaining the ECM. They help produce collagen and other fibers that provide structural support.
- Fasciacytes are specialized cells that are primarily responsible for producing hyaluronan (HA), a glycosaminoglycan that facilitates the gliding of fascial layers. This function is crucial for the spread of LAs during FPBs.
- Myofibroblasts are fibroblasts with contractile abilities, helping regulate the basal tone of fascial tissues. Their density varies depending on the anatomical location, and they play an important role in tissue repair and fibrosis.
- Telocytes: These newly identified cells possess long, thin extensions called telopodes that form networks within the fascia. Telocytes are believed to assist in tissue repair and signaling, contributing to regulating pain and proprioception.
The extracellular matrix (ECM)
The ECM within fascial tissues is a dynamic and vital structure. It comprises collagen fibers (primarily types I and III), elastin, and a water-rich ground substance that contains glycosaminoglycans like hyaluronan. This combination of fibers and fluids allows the fascia to be strong and flexible, facilitating movement and the spread of substances like local anesthetics.
Variations in collagen fiber content and HA levels between different types of fascia (superficial, deep/muscular, etc.) can influence how effectively an FPB works. For example, deep muscular fascia, which is thicker and more structured, is better suited for FPBs than thinner, more fragile epimysial fascia.
How do fascial plane blocks work?
Despite their widespread use, the exact mechanism behind how FPBs work remains somewhat unclear. Researchers agree that the structure of fascia plays a critical role in the spread of LAs. The permeable nature of fascia allows LAs to move through the tissue via two main processes:
- Bulk flow occurs when the LA spreads en masse through the fascial layers due to the pressure from the injection. The separation of fascial layers through hydro-dissection aids this process.
- Diffusion: Once the LA is inside the fascial plane, it diffuses from areas of higher concentration to areas of lower concentration. The ECM helps facilitate this movement, allowing the anesthetic to reach nerves within or near the fascial plane.
Variables affecting FPB success
Several factors can influence the effectiveness of an FPB, including:
- Patient anatomy: Variations in fascial thickness, density, and composition between individuals can impact how well the LA spreads.
- Injection technique: Precise placement of the LA is crucial for optimal results, and ultrasound guidance can help ensure accurate injections.
- Volume and concentration: Adequate volume and the appropriate concentration of the LA are necessary to ensure effective spread and nerve blockade.
Clinical applications of fascial plane blocks
FPBs have been applied in a variety of surgical and nonsurgical settings, from breast and cardiac surgeries to the management of chronic pain. Their opioid-sparing effect makes them particularly valuable in postoperative pain management. Some specific applications include:
- Interpectoral plane block (IPP): This block targets the plane between the pectoralis muscles, reducing the need for general anesthesia in breast surgeries.
- Pecto-serratus plane block (PSP): This block provides effective analgesia for the chest wall and is frequently used in cardiac and thoracic surgeries.
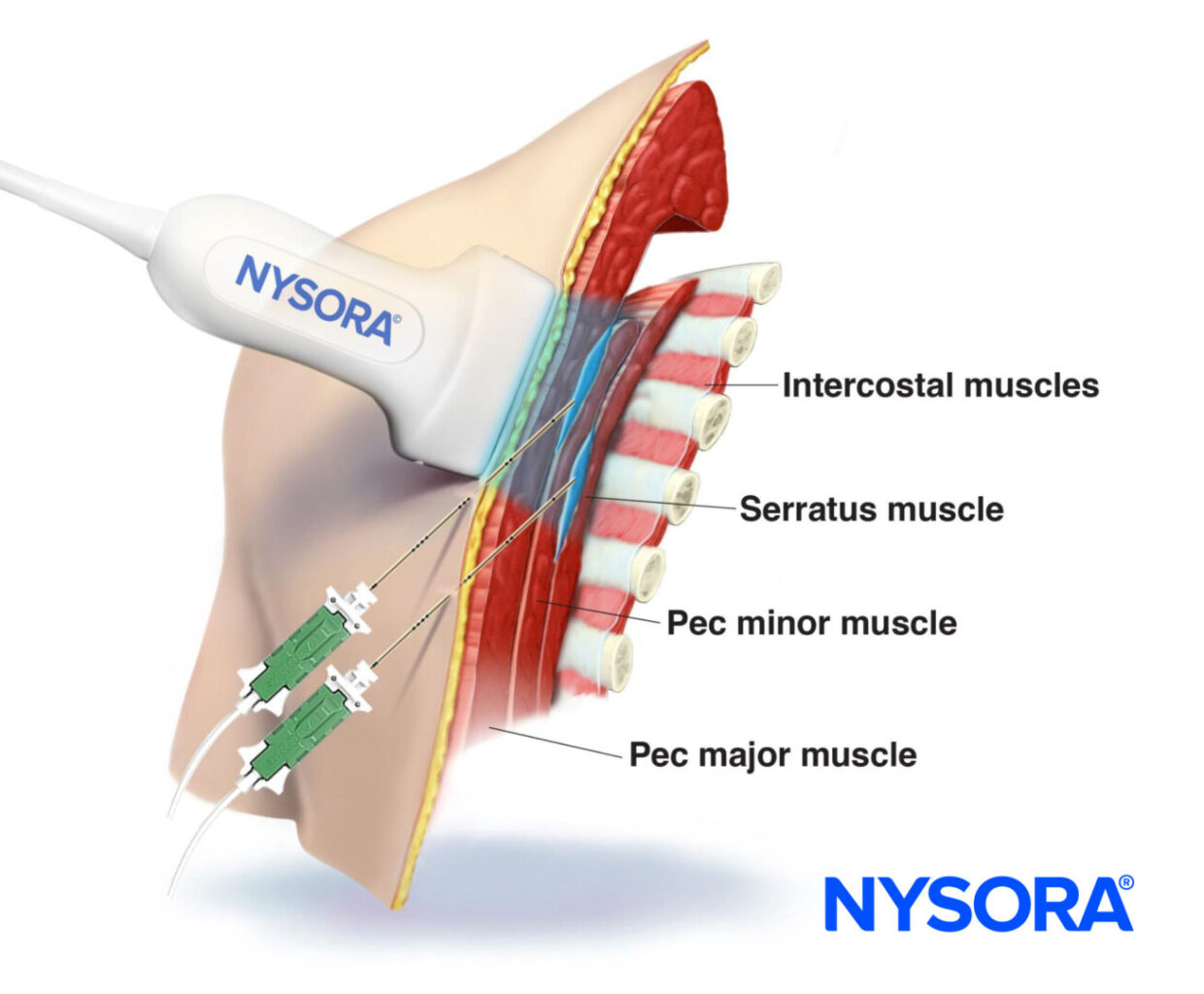
Transducer position and needle insertion in-plane with local anesthetic spread between the pectoralis major and minor muscles for a PEC I block and between the pectoralis minor and serratus anterior muscle for a PEC II block.
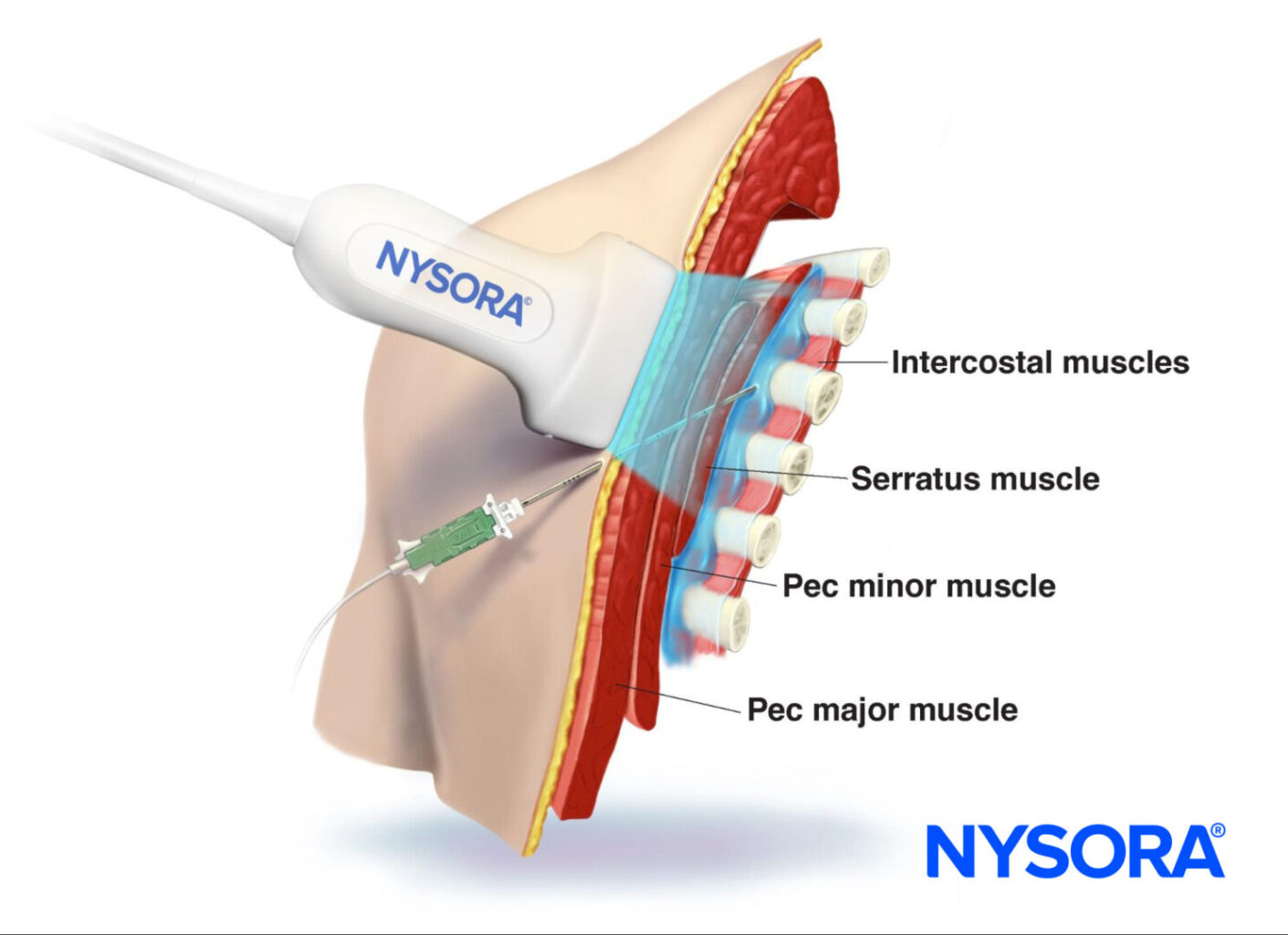
Transducer position and needle insertion in-plane with local anesthetic spread underneath the serratus anterior muscle for a serratus anterior plane block.
The role of hyaluronan in fascial gliding
Hyaluronan (HA) plays a critical role in the movement and distribution of LAs during FPBs. It acts as a lubricant within the ECM, allowing fascial layers to glide smoothly over one another. Variations in HA concentration between different fascial regions can affect the effectiveness of FPBs. For example, fascial regions with higher HA content, such as the thoracolumbar fascia, may offer better LA spread and more effective pain relief than regions with lower HA concentrations.
Challenges and considerations
While FPBs are generally considered safe, there are some challenges to consider:
- Anatomical variability: The thickness and composition of fasciae vary significantly among patients and even within different areas of the same patient. This variability can lead to inconsistent outcomes.
- Fascial densification: Conditions like chronic pain or previous surgeries can cause densification of the fascia, which may hinder the spread of LAs. Techniques like warm saline injections or massage therapy can help reduce this densification, improving the efficacy of FPBs.
- Scar tissue: Scar tissue from prior surgeries can complicate FPB performance by preventing the proper diffusion of the LA.
Conclusion
Fascial plane blocks represent a major advancement in regional anesthesia, offering reliable pain relief while minimizing motor impairment and opioid use. Understanding the microscopic anatomy of fascia and the variables that affect FPB success is crucial for clinicians aiming to optimize these techniques. By capitalizing on the unique features of fasciae, FPBs provide an effective means of managing both acute and chronic pain, improving patient outcomes across a wide range of clinical scenarios.
For more detailed information, refer to the full article in Current opinion in Anesthesiology.
Pirri C, Torre DE, Stecco C. Fascial plane blocks: from microanatomy to clinical applications. Curr Opin Anaesthesiol. 2024;37(5):526-532.
Learn more about opioid-free anesthesia with the Regional Anesthesia Manual e-Course. Access this valuable resource today on the NYSORA LMS website!