HPI: Helpful or Just More Data?
Postoperative acute kidney injury (AKI) remains a serious complication following major abdominal surgery. In efforts to improve outcomes, predictive technologies like the Hypotension Prediction Index (HPI) have been introduced, aiming to guide intraoperative hemodynamic interventions preemptively.
But does HPI make a clinical difference?
A landmark multicenter randomized clinical trial published in Anesthesiology (April 2025) sought to answer that question. The trial evaluated whether HPI-guided management reduces moderate-to-severe AKI incidence in patients undergoing moderate-to-high-risk elective abdominal surgeries compared to standard care.
Let’s explore what the study found, why it matters, and what questions remain unanswered.
What is the Hypotension Prediction Index (HPI)?
- Developed by Edwards Lifesciences, HPI is a machine-learning algorithm that predicts intraoperative hypotension minutes before it occurs.
- It uses real-time arterial waveform data to generate a predictive score (0–100), with scores ≥ 80 prompting intervention.
- The system integrates with Edwards’ Hemosphere platform and Acumen sensors to trigger fluid and/or vasopressor administration when thresholds are exceeded.
Study design
- Study period: October 2022 – February 2024
- Participants: 917 adults undergoing major abdominal surgery at 28 hospitals (Spain and Jordan)
- Inclusion: Age ≥ 65 or ASA Physical Status III–IV undergoing ≥2-hour surgery
- Exclusion: Emergency surgery, nephrectomy, preexisting dialysis, minor laparoscopic procedures
- Groups:
- HPI-guided therapy group: Protocol-driven interventions when HPI > 80
- HPI-guided therapy group: Protocol-driven interventions when HPI > 80
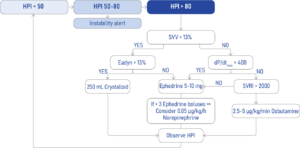
SSV, stroke volume variation; Eadyn, Dynamic arterial elastance; dP/dtmax, Maximum rate of the arterial pressure rise during systole (mmHg/s); SVRI, Systemic vascular resistance index.
- Standard care group: Real-world hemodynamic management without HP
Key findings
Primary outcome: Moderate-to-severe AKI (within 7 days)
- HPI group: 6.1% (28/459)
- Standard care: 7.0% (32/458)
Secondary outcomes
- Overall AKI (any stage): 22.2% (HPI) vs. 25.6% (Standard)
- Renal replacement therapy: 1.1% in both groups
- 30-day mortality: 1.1% (HPI) vs. 0.9% (Standard)
- Overall complication rate: 31.9% (HPI) vs. 29.7% (Standard)
- Hospital stay: Median 6 days in both groups
Subgroup insight
A trend toward reduced AKI in patients without hypertension was observed in the HPI group, but this did not retain significance after correction for multiple comparisons.
Critical insights
Vasopressor use
- HPI patients received more vasopressors, especially ephedrine and norepinephrine
- No phenylephrine was used in the HPI group, but 23.5% received it in the control group
- Aggressive vasopressor therapy may have blunted renal benefits
Predictive power vs. Clinical utility
- HPI accurately predicts hypotension
- But prediction ≠ improved outcomes unless paired with effective, personalized treatment responses
Conclusion: HPI is not a silver bullet—yet
While the Hypotension Prediction Index can enhance hemodynamic insight, this large multicenter trial found no significant reduction in postoperative AKI or complications when using HPI-guided therapy versus standard intraoperative management.
This underscores the complexity of perioperative care and suggests that predictive tools alone are not enough—they must be embedded in nuanced, individualized clinical strategies.
Reference: Ripollés-Melchor J. et al. Anesthesiology. 2025;142(4):639-654.
For more information on hypotension and AKI, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.