Mastering the Ultrasound-Guided Rectus Sheath Block
Initially sparingly utilized due to risks of vascular injury, the rectus sheath block has gained popularity for providing postoperative pain relief for midline abdominal incisions, especially with the introduction of ultrasound guidance. Administered bilaterally, it efficiently anesthetizes the anteromedial abdominal wall and periumbilical area, targeting spinal dermatomes T9, T10, and T11.
Although the rectus sheath block is effective and perceived as safe, risks are involved, as with any medical procedure. Therefore, the study of Kwon et al. 2023 aimed to identify the incidence of complications associated with rectus sheath blocks and to outline best practices to minimize these risks.
Study design
- The study retrospectively analyzed data from 4,033 patients who underwent real-time ultrasound-guided rectus sheath blocks between February 2017 and February 2021.
- The procedures were primarily performed for perioperative pain control in laparoscopic surgeries with an umbilical port.
Key Findings
- The overall complication rate observed in the study was 2.4%. While this might appear low, the study highlights that even procedures considered basic, like a rectus sheath block, can lead to significant complications.
- The most common complication, occurring in 2.2% of the cases, was extrarectus sheath injection. This included injections of preperitoneal (0.9%) and intraperitoneal (1.3%). These errors can reduce the effectiveness of the block and, in severe cases, lead to organ damage.
- Vascular injuries were rare but serious, with an incidence of 0.2%. All cases resulted in hematomas, primarily from injuries to the inferior epigastric artery. There was also one case involving the inferior mesenteric artery, which led to a retroperitoneal hematoma.
- Notably, the study reported no cases of bowel injury or local anesthetic systemic toxicity (LAST), which are potential risks associated with this procedure.
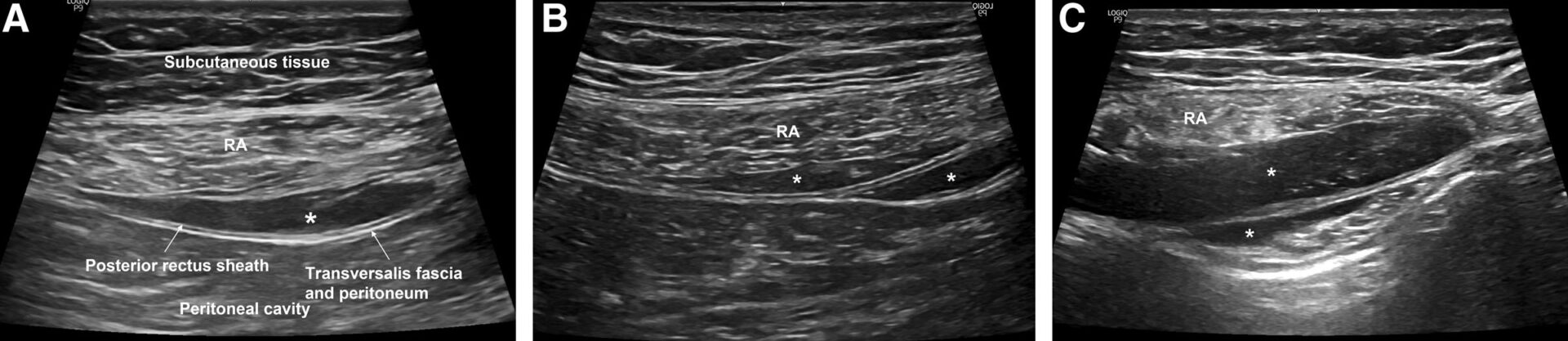
Asterisk (*) indicates a deposit of local anesthetics. A) Accurate position of local anesthetics in a rectus sheath block. B) Inadequate deposit of local anesthetics in a preperitoneal injection in a rectus sheath block. C) Inadequate deposit of local anesthetics in an intraperitoneal injection in a rectus sheath block. Both (B) and (C) represent extrarectus sheath injections in a rectus sheath block. RA indicates rectus abdominis muscle; RSB, rectus sheath block. Source of the image: Kwon et al. Anesthesia & Analgesia. 2023. 136(2):365-372.
Technical Considerations
The study emphasizes several technical considerations that can help mitigate the risks of complications during a rectus sheath block:
- Needle tip tracking: Accurate needle tip visualization is crucial, particularly near the posterior rectus sheath. The study suggests that advancing the needle in small increments and ensuring clear hydrodissection can enhance safety.
- Preprocedural ultrasound scanning: Incorporating a preprocedural scan using color Doppler to identify vasculature is strongly recommended. This step is vital to avoid inadvertent vascular injuries, particularly in areas where vessels are closely positioned to the rectus sheath.
- Choice of needle and approach: The study utilized a 23-gauge Quincke needle with a medial-to-lateral in-plane approach. While this method ensures the local anesthetic reaches the lateral edge of the rectus sheath, the study acknowledges that different approaches might yield varying results.
- Timing of the procedure: Preoperative rectus sheath blocks are preferred over postoperative blocks. Preoperative administration allows for early detection of any adverse events and has been shown to reduce postoperative opioid consumption.
- Patient selection: The study predominantly involved patients with a low body mass index (BMI), which might limit the generalizability of the findings to populations with higher BMI. Nonetheless, the technical principles outlined are broadly applicable.
Conclusion
Although ultrasound-guided rectus sheath blocks are generally safe, they are not without risks. The findings underscore the importance of a meticulous technique and thorough preprocedural planning to minimize complications.
For more detailed information, refer to the full article in Anesthesia & Analgesia.
Kwon HJ, Kim YJ, Kim Y, et al. Complications and Technical Consideration of Ultrasound-Guided Rectus Sheath Blocks: A Retrospective Analysis of 4033 Patients. Anesth Analg. 2023;136(2):365-372.
For a successful rectus sheath block, adhere to the following 4 steps
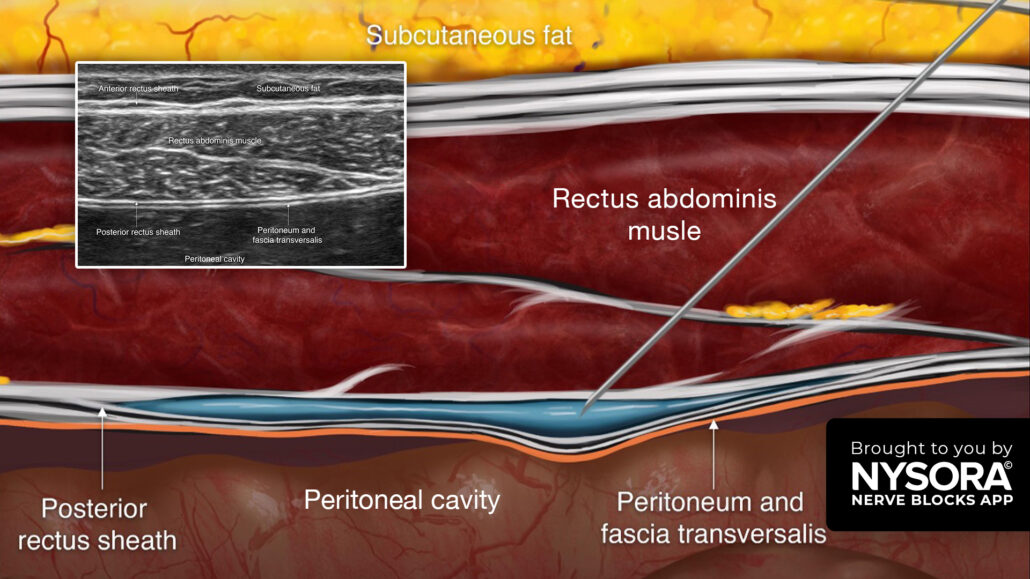
- Place the transducer transversely just above the umbilicus, 1 cm lateral to the midline.
- Identify the rectus abdominis muscle and posterior rectus sheath.
- Insert the needle in-plane through the rectus abdominis muscle until the tip reaches the space between the muscle and posterior rectus sheath, and inject 10-15 mL of local anesthetic.
- Repeat on the contralateral side for a bilateral block. Note: For optimal results, the block must be performed on both sides.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App in book format – the perfect study companion with the Nerve Blocks app!