More Protein Is Not Better in Critically Ill Patients
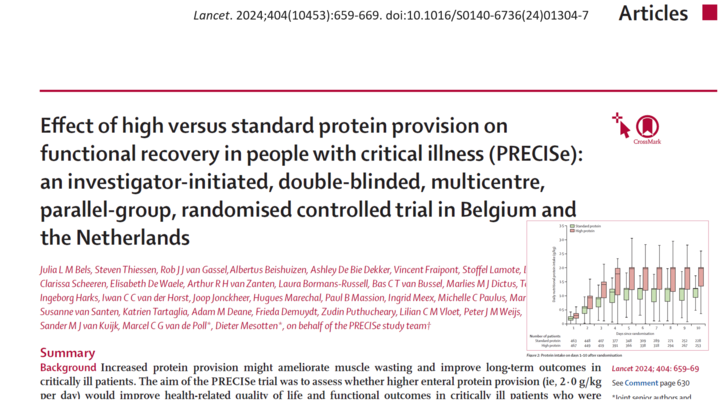
A recent landmark study published in The Lancet has brought new insights into the impact of high-protein nutrition in critically ill patients. The PRECISe Trial, a multi-center, randomized controlled trial, investigated whether higher enteral protein provision (2.0 g/kg per day) could improve functional outcomes and health-related quality of life (HRQoL) compared to standard protein provision (1.3 g/kg per day).
Surprisingly, patients who received high-protein nutrition fared worse in terms of health-related quality of life and functional recovery after an intensive care unit (ICU) stay.
Let’s break down the findings of this study and what they mean for critically ill patients.
Why does protein matter in critical illness?
- Patients in the ICU often suffer from muscle wasting and weakness, which can significantly reduce their quality of life and functional ability after discharge. Protein is thought to play a crucial role in preserving muscle mass, and some previous studies suggested that higher protein intake might lead to better recovery outcomes.
- However, the optimal protein intake for critically ill patients remains uncertain, with clinical guidelines recommending between 1.2 and 2.0 g/kg per day.
The PRECISe Trial set out to determine whether pushing protein intake to the higher end of this range would lead to better health outcomes.
Study Design
- Type of Study: Double-blinded, randomized controlled trial
- Locations: Conducted in 10 hospitals across Belgium and the Netherlands
- Participants: 935 critically ill patients requiring mechanical ventilation
- Intervention:
- High-protein group: 2.0 g/kg/day of enteral protein
- Standard-protein group: 1.3 g/kg/day of enteral protein
- Primary Outcome: EQ-5D-5L health utility score (a measure of HRQoL) at 30, 90, and 180 days post-randomization
- Secondary Outcomes: Mortality, physical function, hospital stay duration, and muscle-related outcomes
Key findings
1. Worse quality of life in the high-protein group
Patients who received higher protein intake had lower health-related quality of life scores during follow-up at 30, 90, and 180 days. The mean difference was -0.05, indicating a clinically and statistically significant decline in HRQoL compared to the standard-protein group.
2. No improvement in functional recovery
Despite the expectation that more protein would preserve muscle mass, the trial found no significant differences in muscle strength, handgrip strength, or walking ability between the two groups.
3. Increased gastrointestinal intolerance
Patients in the high-protein group experienced more gastrointestinal issues, such as vomiting, diarrhea, and bloating. The use of prokinetic drugs (to improve digestion) was higher in this group as well.
4. No significant difference in mortality, but a concerning trend
- The probability of death was slightly higher in the high-protein group (42%) compared to the standard-protein group (38%).
- While this difference was not statistically significant, the trend raises questions about whether excess protein intake could have unintended harmful effects in critically ill patients.
What does this mean for ICU nutrition?
The PRECISe Trial challenges the common assumption that more protein is always better for critically ill patients. Current clinical guidelines recommending protein intake up to 2.0 g/kg/day may need to be re-evaluated.
Key takeaways for clinicians:
- A standard protein intake of 1.3 g/kg/day appears sufficient to support recovery without worsening HRQoL.
- Higher protein intake does not improve muscle strength or functional recovery.
- Gastrointestinal complications are more common with high-protein feeding, which may hinder patient recovery.
- A personalized approach to protein provision is needed, considering factors like the patient’s medical history, nutritional status, and ability to tolerate enteral feeding.
Final thoughts
The PRECISe Trial is a game-changer in ICU nutrition research. It provides strong evidence that high-protein enteral feeding (2.0 g/kg/day) does not improve functional recovery or quality of life—and may actually be detrimental for critically ill patients.
These findings highlight the importance of individualized nutrition strategies rather than a one-size-fits-all approach.
Clinicians and researchers must continue investigating how to optimize nutrition in the ICU, balancing the need for protein with patient tolerance and long-term recovery goals.
For more information on protein recommendations, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the Anesthesia Assistant app today and experience the future of anesthesia education and decision-making.