Reviewing the Medico-Legal Cases: Patterns That Lead to a Higher Risk for Both Neurologic Complications and a Higher Risk of Being Named in a Lawsuit
Having published several standards textbooks in anesthesiology and over 200 scientific papers, it is no wonder that dr. Hadzic is often asked to consult as a medico-legal witness. He does not take on all cases he is asked to consult on; instead, he picks and chooses only the ones that he can learn something from and use what he learns in making recommendations for safer medical practice.
Check out dr. Hadzic’s thoughts on the complications in regional anesthesia, the increasing number of medico-legal cases, and patterns that lead to a higher risk for both neurologic complications and a higher risk of being named in a lawsuit.
One of my colleagues, also a medico-legal expert who is both a doctor and an attorney, recently voiced a concern that he has seen an increasing number of medico-legal cases and lawsuits involving regional anesthesia. Now, I do not think that regional anesthesia carries a higher risk of complications than general anesthesia, even with regard to the risk of nerve injury. However, being that regional anesthesia is becoming the standard of care in many institutions as a part of ERAS programs and multi-modal postoperative pain protocols, the complications in regional anesthesia, like in medicine at large, are a function of the number of procedures. Meaning – the more procedures violating skin integrity are being done, being that nerve blocks or surgical procedures – the higher the number of complications.
However, this does not mean that regional anesthesia has a higher risk of complications than general anesthesia. It simply means that the more nerve blocks you do – the higher the chance of complications. Although the risk is very low – likely 1 in 3,000 to 1 in 4,000, it is simply a number game. The question is how to further decrease the risk to the point at which you may never see a complication in your own practice.
In reviewing the medico-legal cases in which practitioners are being sued over nerve injury that potentially resulted from the regional anesthesia, I have identified several patterns that lead to a higher risk for both neurologic complications and a higher risk of being named in a lawsuit. In cases of nerve injury that may be related to nerve blocks, it is often the lack of monitoring and documentation that exposes the practitioners to the risk of being sued, and more importantly, possibly expose the patient to an injury.
Since NYSORA is one of the most prominent teaching organizations, I often see images and illustrations from NYSORA’s Nerve Block App, Nerve Block Manual, or the Compendium of Regional Anesthesia included in the legal documents. However, it is extremely interesting to see from these documents the lack of understanding of how the combination of existing, and ubiquitously available monitoring can be beneficial in avoiding these complications.
A closer look at the PENG or pericapsular nerve group infiltration block
As the PENG block is increasingly more often being used for the purpose of analgesia after total hip arthroplasty, we are also seeing an increase in the incidence of femoral nerve injury. In one occurrence I reviewed, the practitioners who were involved in the case adamantly claimed that femoral nerve injury in their case could not have been possibly caused by the PENG block because the PENG block procedure has nothing to do with the femoral nerve. While this is true, the involved practitioners are completely disregarding the fact that a very minor error in the needle insertion angle can easily lead to the needle path toward the femoral nerve. Let’s review this.
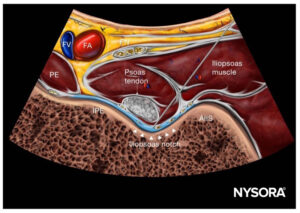
While many practitioners have completely abandoned any other monitoring methods but ultrasound, you can see how using nerve stimulation as a safety monitor can contribute useful safety information of benefits to both patients and the rigors of accurate, and objective medico-legal documentation. Although not using nerve stimulation during ultrasound-guided nerve blocks does not comprise a violation of standards of care, the documentation that states that quadriceps motor response was absent during PENG block assures everyone involved that the practitioner has invested additional, objective monitoring methods to prevent femoral nerve injury during PENG block.
LINK: Get the NYSORA Nerve Block Manual
NYSORA Nerve Block Manual is the definitive guide to ultrasound-guided peripheral nerve blocks (PNBs) and interventional analgesia injections. Here’s what you will find in it:
- All block techniques for head and neck, upper and lower extremities, and the newest inter-fascial injections
- Stepwise instruction on anatomy, block distribution, and local anesthetic selection
- NYSORA’s Highly didactic clinical images and Reverse Ultrasound Anatomy facilitate the understanding of sonoanatomy
- Practical tips immediately applicable in clinical practice
- Decision-making algorithms that simplify implementation to clinical practice