Sugammadex in CICV Emergencies
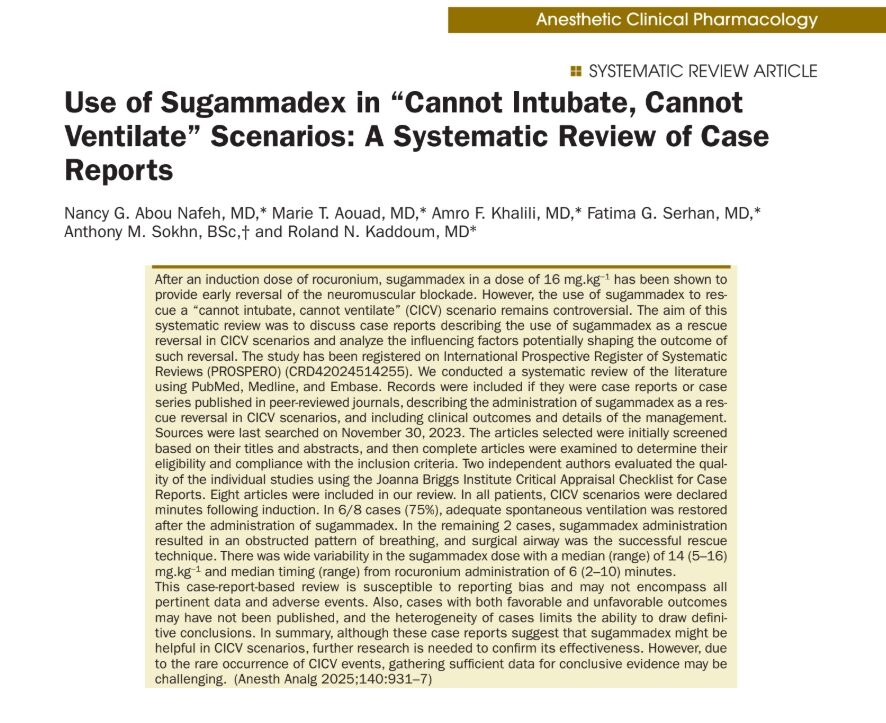
When anesthesiologists encounter a “Cannot Intubate, Cannot Ventilate” (CICV) scenario, every second counts. The situation is dire—oxygen levels plummet, airway access is blocked, and the clock is ticking. A recent systematic review published in Anesthesia & Analgesia explores whether sugammadex, a drug known for its rapid reversal of neuromuscular blockade, can serve as a reliable rescue strategy in such high-stakes emergencies.
Researchers led by Dr. Nancy Abou Nafeh and colleagues conducted a systematic review of eight published case reports detailing the use of sugammadex in real-world CICV scenarios. These reports span over a decade (2010–2021) and involve both adult and neonatal patients. The core question: Can sugammadex be an effective “rescue reversal” agent in critical CICV events?
Understanding Sugammadex
Sugammadex is a modified gamma-cyclodextrin that binds tightly to aminosteroid neuromuscular blocking agents (NMBAs) like rocuronium and vecuronium, reversing their effects rapidly. It is commonly used to:
- Reverse residual neuromuscular blockade after surgery.
- Avoid the side effects of traditional reversal agents like neostigmine.
- Allow for rapid NMBA reversal in neuromonitoring or allergic reaction settings.
In theory, reversing paralysis might help a patient resume spontaneous breathing during a CICV crisis. But does this hold true in practice?
Key findings
Out of the eight CICV cases:
- 6 patients (75%) regained adequate spontaneous ventilation after receiving sugammadex.
- 2 patients (25%) experienced airway obstruction despite reversal, requiring emergency surgical airways.
- Median dose of sugammadex: 14 mg/kg (range: 5–16 mg/kg).
- Time between rocuronium administration and sugammadex: 6 minutes (range: 2–10 minutes).
- All patients received rocuronium and propofol; 75% also received opioids.
Why does Sugammadex work sometimes but not always?
- Timing: Delays in administering sugammadex ( > 6–8 minutes) may result in critical hypoxia.
- Dose: While the standard rescue dose is 16 mg/kg, many successful cases used lower doses.
- Residual drug effects: Propofol and opioids can suppress respiration, even after NMBA reversal.
- Upper airway obstruction: Recovery of the diaphragm without upper airway muscle tone can worsen airway collapse.
- Multiple intubation attempts: Trauma from repeated laryngoscopies can cause edema and laryngospasm.
Best practices for Sugammadex use in CICV:
- Administer early: Aim to give sugammadex as soon as a CICV situation is suspected.
- Prepare preemptively: Ensure the drug is ready and dosed appropriately before induction.
- Avoid repeated intubation attempts: These increase the risk of swelling and airway trauma.
- Monitor TOF: Use Train-of-Four monitoring to assess neuromuscular function post-reversal.
- Manage upper airway obstruction: Be ready with airway adjuncts or surgical backup if obstruction persists.
- Prioritize oxygenation: Follow existing airway algorithms and consider FONA when ventilation fails.

Final thoughts
While sugammadex shows promise as a pharmacologic tool in the dreaded CICV scenario, its success is highly context-dependent. Early administration, correct dosing, and rapid clinical decision-making are critical. But it is not a magic bullet; airway obstruction, hypoxia, and sedation must still be actively managed.
This review provides an important step in understanding the role of sugammadex in airway emergencies, but more data are needed. Given the rarity of CICV cases, anesthesiologists are urged to report outcomes, favorable or not, to contribute to this evolving field.
For more information on this topic, check out Anesthesia Updates on the NYSORA Anesthesia Assistant App.
Get access to step-by-step management algorithms, the latest research, and peer-reviewed insights—all in one place. Download the app today and experience the future of anesthesia education and decision-making.