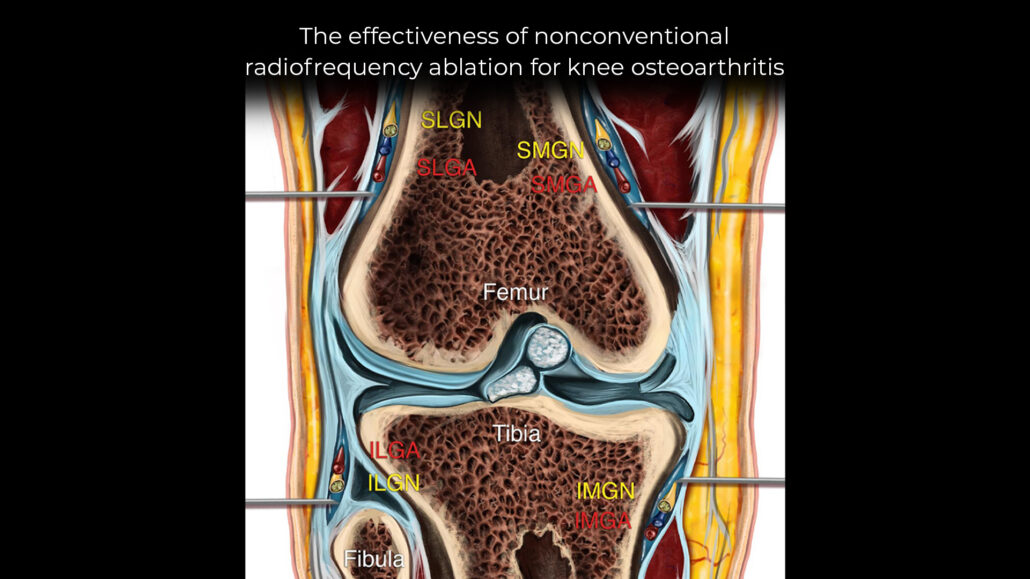
The effectiveness of nonconventional radiofrequency ablation for knee osteoarthritis
Knee osteoarthritis (OA) is a common, degenerative joint condition that leads to chronic pain and functional limitations. While conventional treatments such as physiotherapy, medications, and surgery offer temporary relief, more advanced pain management options like radiofrequency ablation (RFA) have shown promising results. This article delves into the effectiveness of nonconventional RFA techniques—specifically pulsed and cooled RFA—targeting the genicular nerves for knee OA pain management based on recent research findings.
What is radiofrequency ablation?
Radiofrequency ablation (RFA) is a minimally invasive procedure that uses thermal energy to disrupt nerve signaling, thereby reducing pain. The technique has evolved, with pulsed and cooled RFA emerging as alternatives to the traditional high-temperature probe method. These newer techniques minimize damage to surrounding tissues while offering long-lasting pain relief.
- Cooled RFA: This method pumps water inside the probe to maintain lower temperatures (60°C – 70°C) while targeting larger areas of neuronal tissue. This reduces thermal damage to surrounding tissues, leading to prolonged pain relief.
- Pulsed RFA: Pulsed RFA uses intermittent high-voltage bursts to limit tissue heating (maximum 42°C), thus preventing permanent nerve damage. This technique reduces the risk of complications and may provide reversible pain relief.
Meta-analysis study: Evaluating effectiveness
A recent meta-analysis by Soetjahjo et al. (Pain Physician, 2024) examined the effectiveness of pulsed and cooled RFA in treating knee OA pain. The study included 11 publications and assessed both pain relief and physical function improvement.
Key findings
- Pain reduction: Both cooled and pulsed RFA led to significant pain reduction at 1, 3, and 6 months post-procedure. There was no significant difference in pain relief between the two techniques.
- Physical function: Pulsed RFA showed greater improvement in physical function at the 1-month and 3-month follow-ups, while cooled RFA did not demonstrate significant functional gains.
- Adverse effects: Few adverse effects were reported, primarily minor issues such as post-procedure swelling and stiffness.
Pain and function outcomes
The primary goal of RFA in knee OA is to alleviate pain and improve joint function. Here’s a breakdown of the study’s findings:
- Pain reduction over time:
- 1-Month follow-up: Significant pain relief was observed in both pulsed and cooled RFA groups, with an average standardized mean difference (SMD) of 3.42.
- 3-Month follow-up: Pain reduction persisted, with similar SMD values. Cooled RFA continued to show effectiveness, though some heterogeneity was noted between studies.
- 6-Month follow-up: Pain levels remained significantly lower than baseline, but the rate of improvement began to plateau.
- 12-Month follow-up: No significant pain improvement was observed, suggesting that the effectiveness of both techniques may diminish over time as nerves regenerate.
- Physical function (WOMAC Score):
- 1- and 3-Month follow-ups: Pulsed RFA demonstrated significant functional improvement at early follow-ups, improving the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score.
- 6-Month follow-up: Both pulsed and cooled RFA had limited impact on long-term functional recovery.
- 12-Month follow-up: Functional improvements diminished, aligning with the waning pain relief observed at this stage.
Step-by-step: Patient journey during RFA
- Consultation and evaluation: The patient’s knee condition is evaluated, potentially using imaging tests to identify the genicular nerves responsible for pain.
- Procedure preparation: The procedure is usually performed under local anesthesia. Fluoroscopy or ultrasound may be used to guide the placement of the RFA probe.
- Nerve ablation: Depending on the chosen technique (cooled or pulsed), the probe will deliver thermal energy to the targeted nerves.
- Recovery: The procedure typically takes 30-45 minutes, and patients can go home the same day. Mild swelling and discomfort may be experienced for a few days.
- Follow-up: Pain relief can begin within days, with maximum effect seen within a few weeks.
Who is a candidate for RFA?
RFA is ideal for patients who:
- Have knee osteoarthritis with chronic pain that hasn’t responded well to other treatments.
- Are not candidates for knee replacement surgery.
- Seek a minimally invasive solution with minimal downtime.
Conclusion
Nonconventional RFA techniques like pulsed and cooled RFA show significant promise in reducing knee OA pain with minimal adverse effects. Both methods effectively alleviate pain for up to 6 months, with pulsed RFA offering better functional outcomes at early follow-ups. However, more research is needed to explore their long-term efficacy and functional impact beyond 12 months.
For individuals suffering from debilitating knee OA pain, RFA offers a potential solution that bridges the gap between conservative treatments and surgery, providing lasting pain relief with minimal risks.
For more details, read the full article in Pain Physician.
Soetjahjo B, Adriansyah D, Yudistira MB, Rahman AN, Herman H, Diwan S. The Analgesic Effectiveness of Genicular Nerve-targeted Cooled and Pulsed Radiofrequency Ablation for Osteoarthritis Knee Pain: A Systematic Review and Meta-analysis. Pain Physician. 2024;27(7):357-373.
Eager to learn more about genicular nerve blocks and other pain management techniques? Download NYSORA’s US Pain App for 30+ step-by-step guides!