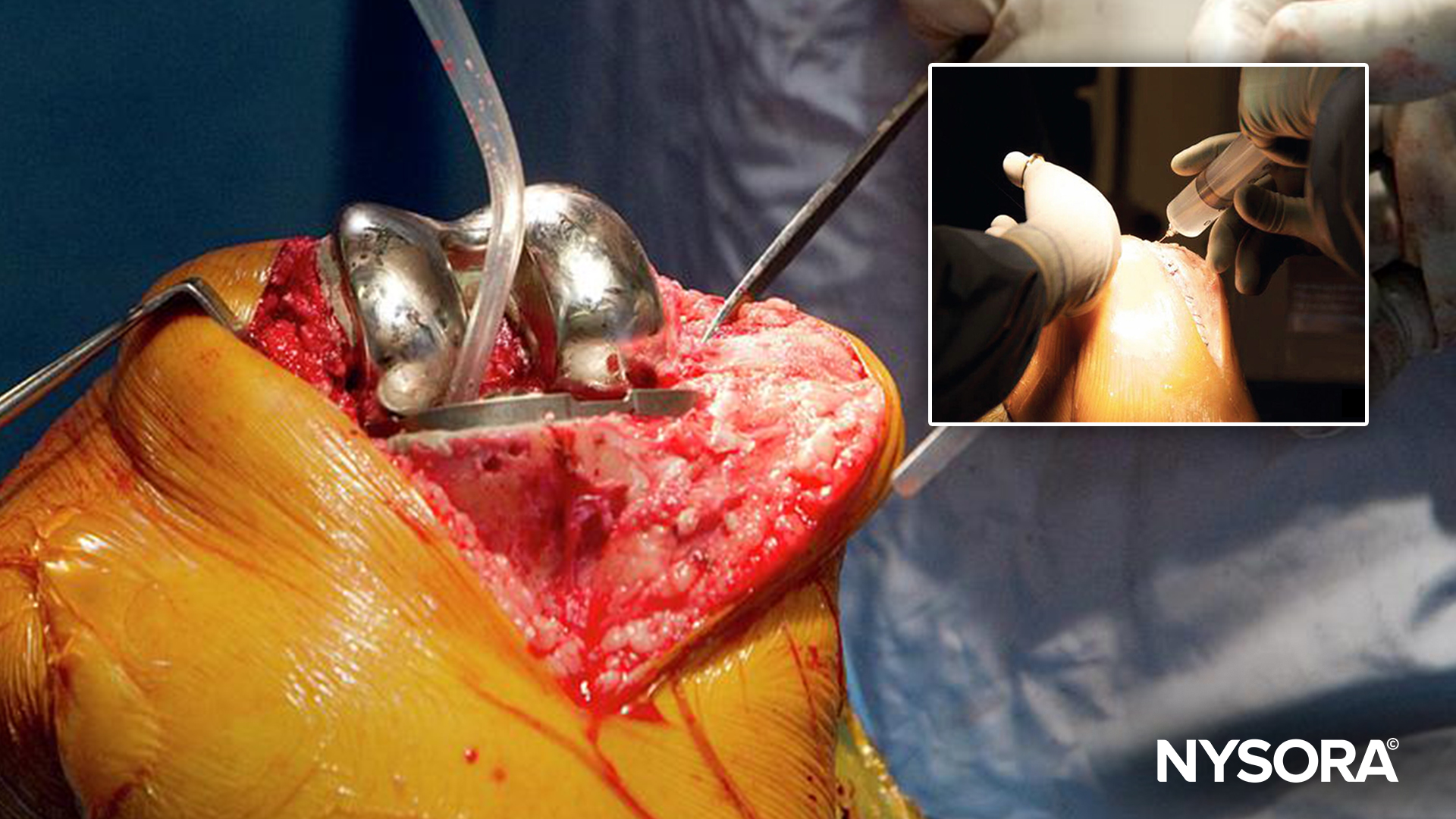
Total knee arthroplasty (TKA) is a common surgical procedure for patients with severe knee osteoarthritis, aimed at alleviating pain and improving function. Effective postoperative pain management is critical for patient recovery, mobility, and satisfaction. Traditional multimodal analgesia for TKA often includes periarticular injections (PAI) of local anesthetics. However, a recent study by YaDeau et al., published in the Anesthesia & Analgesia journal, explores whether PAI is necessary when combined with adductor canal block (ACB) and infiltration between the popliteal artery and capsule of the knee (IPACK) blocks, questioning the necessity and efficacy of these injections.
Study objective and methods
The study objective was to evaluate the efficacy of PAI in reducing postoperative pain in patients undergoing TKA who were already receiving a multimodal analgesia regimen that included ACB and IPACK blocks.
This randomized, blinded, placebo-controlled noninferiority trial enrolled 94 patients undergoing primary unilateral TKA. Participants were randomly assigned to receive either an active PAI (a mixture of bupivacaine, morphine, methylprednisolone, cefazolin, and saline) or a saline PAI (sham). All patients received a standardized multimodal analgesic protocol that included spinal anesthesia, ACB and IPACK blocks, intraoperative ketamine and ketorolac, and postoperative medications such as meloxicam, acetaminophen, duloxetine, and oral opioids.
The primary outcome was pain with ambulation on postoperative day 1 (POD1), while secondary outcomes included opioid consumption, pain at rest, worst pain, pain interference, quality of recovery, patient satisfaction, length of hospital stay, chronic pain, and orthopedic outcomes.
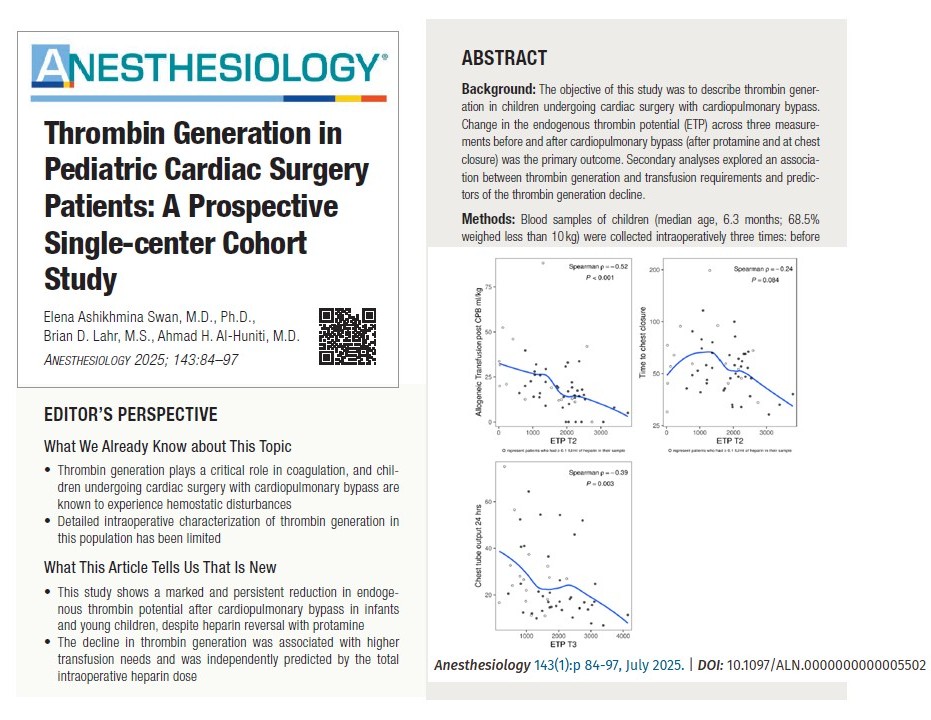
Key findings
- Primary outcome: Pain with ambulation on POD1 was not significantly different between patients receiving active PAI (with local anesthetic) and those receiving a saline PAI (sham) (4.26 ± 3.03 vs 4.55 ± 2.7, p=0.120).
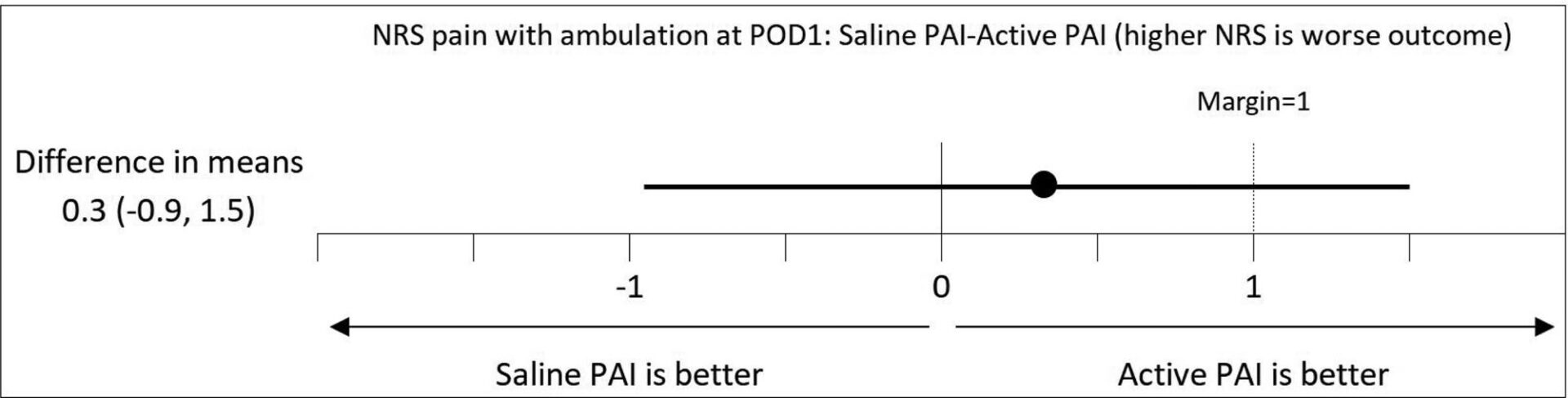
Postoperative pain: a noninferiority graph. NRS pain with ambulation at POD1; mean and 95% confidence intervals. NRS indicates numeric rating scale; PAI, periarticular injection; POD1, postoperative day 1.
- Secondary outcomes: No significant differences were observed in opioid consumption, pain at rest, worst pain, pain interference, quality of recovery, satisfaction, length of stay, chronic pain, and orthopedic outcomes.
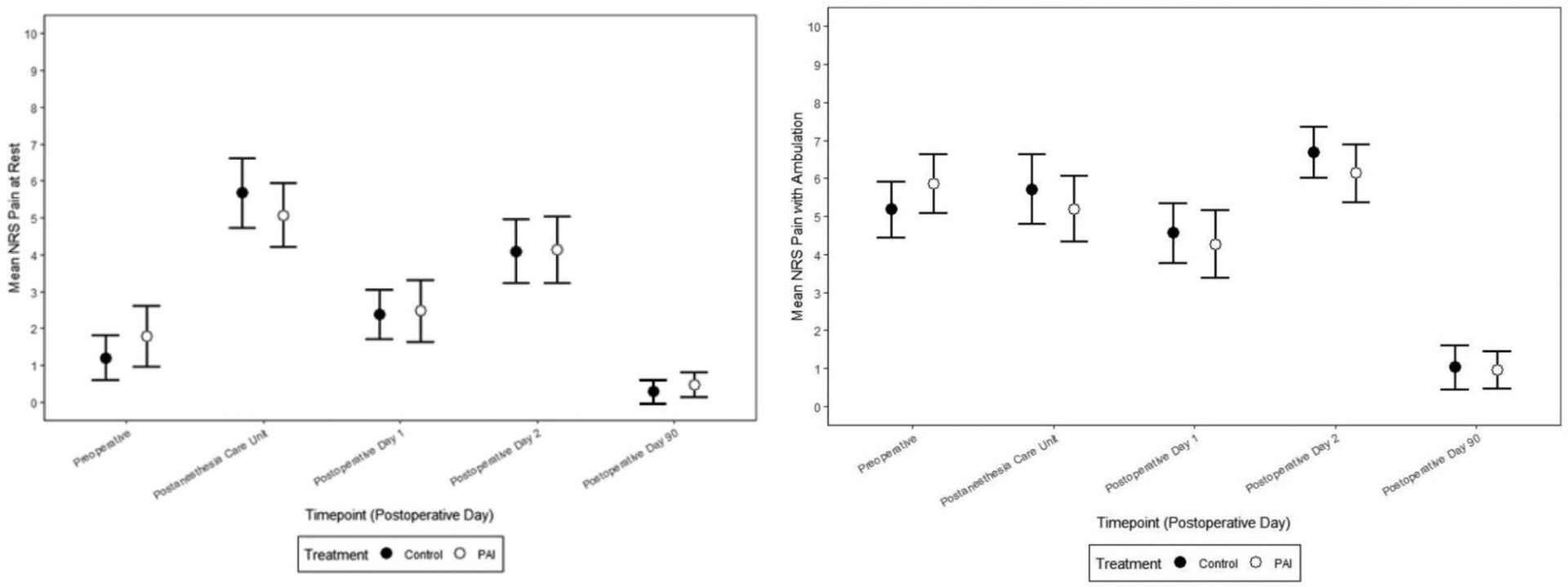
Pain scores over time (NRS for pain [0–10]), at rest and with ambulation. Mean NRS pain score with ambulation (A) and at rest (B) by randomized group over time. Data are plotted as mean and 95% confidence interval. NRS indicates numerical rating scale.
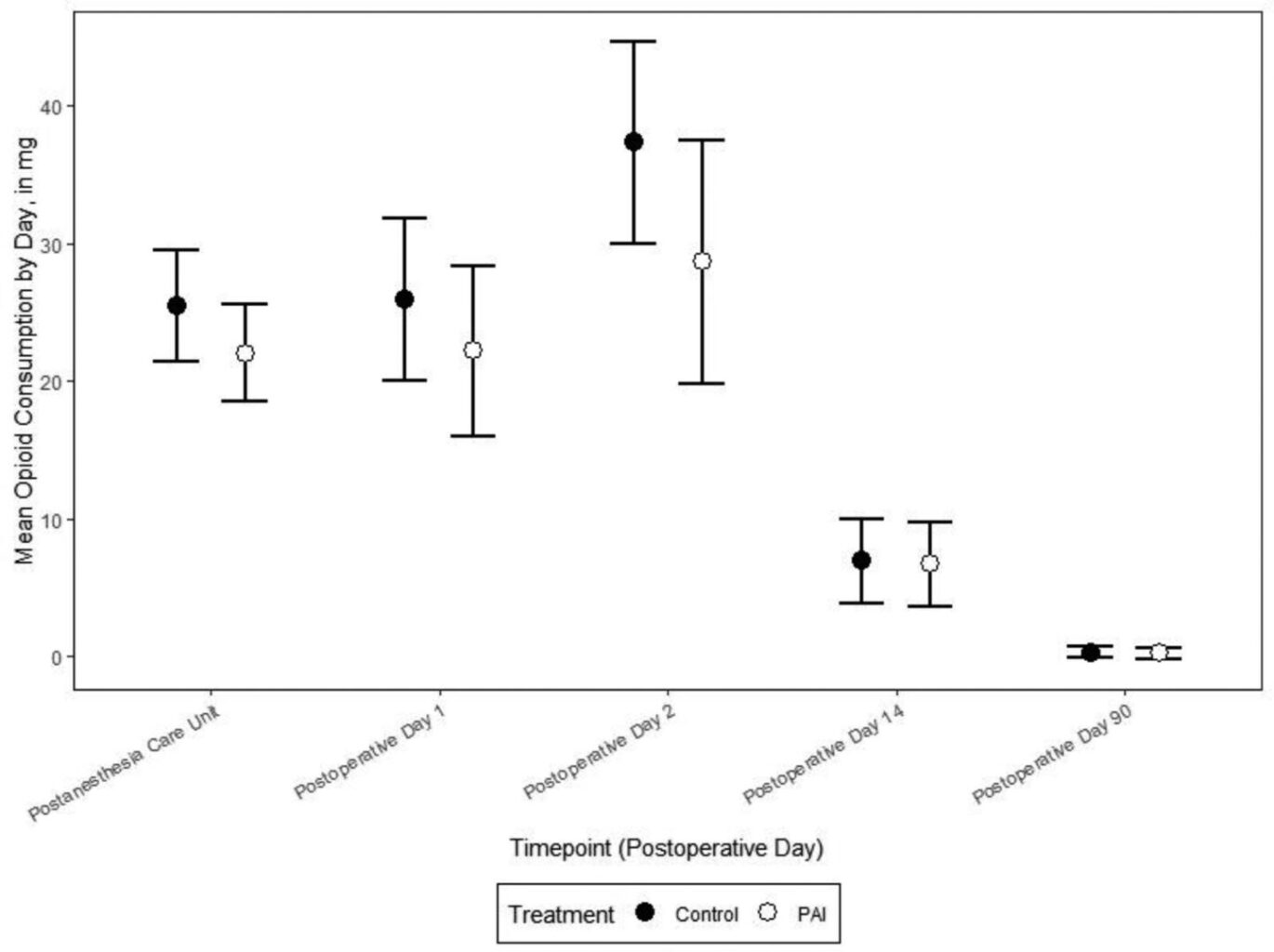
Total mean opioid morphine equivalents in milligrams by randomization group over time. Data are plotted as mean and 95% CI. Results represented show opioids taken after T = 0 which was defined as the end of anesthesia. Patients in PAI group received 8 mg Morphine intraoperatively (before T = 0) which was is not reflected in this figure. When considered, additional 8mg of morphine for the PAI group did not change the outcome measures. CI indicates confidence interval; OME, morphine equivalents; PAI, periarticular injection.
Clinical implications
The study suggests that for TKA patients receiving comprehensive analgesic protocols, the addition of PAI does not provide significant benefits over saline PAI. This indicates flexibility in choosing whether to include PAI in pain management regimens.
Considerations
- Local anesthetic dose: PAI involves a higher dose of local anesthetics, potentially increasing the risk of systemic toxicity.
- Needle precision: PAI is less precise compared to ultrasound-guided IPACK blocks.
- Surgeon preference: Not all surgeons prefer to perform PAI.
Limitations
The study was conducted at a single center, and results might differ in other settings. The specific mixture used for PAI might not be entirely evidence-based but reflected the standard practice at the study hospital.
Conclusion
This study provides valuable insights into pain management for TKA patients. While PAI does not show superiority over saline injections in the context of comprehensive analgesia regimens, the choice to use PAI can be based on individual patient needs and resource availability.
For more detailed information, refer to the full article in Anesthesia & Analgesia.
YaDeau JT, Cushner FD, Westrich G, et al. What Is the Role of a Periarticular Injection for Knee Arthroplasty Patients Receiving a Multimodal Analgesia Regimen Incorporating Adductor Canal and Infiltration Between the Popliteal Artery and Capsule of the Knee Blocks? A Randomized Blinded Placebo-Controlled Noninferiority Trial. Anesth Analg. 2024;138(6):1163-1172.
Further research
Larger multicenter studies could provide more definitive answers and help tailor analgesia protocols to optimize patient outcomes in TKA.
Discover more about adductor canal and IPACK blocks by downloading the Nerve Blocks App HERE. Or you can choose the bestselling NYSORA Nerve Blocks App in book format – an essential resource for mastering nerve blocks!