Understanding the cervical plexus: Anatomy, blocks, and clinical relevance
A cervical plexus block is indicated for carotid endarterectomy, superficial neck procedures, and clavicle fracture analgesia. This block targets the cervical plexus, which is formed by the anterior rami of the C1-C4 cervical spinal nerves. The technique aims to distribute local anesthetic around the plexus’s superficial branches, achieving sensory anesthesia in the anterolateral neck, retro-auricular areas, and the skin above and below the clavicle.
The cervical plexus is a significant network of nerves that plays an essential role in the sensory and motor functions of the neck and parts of the upper torso. Its importance in clinical applications, particularly in regional anesthesia, cannot be overstated. This article by Jarvis et al. 2023 explores the anatomy of the cervical plexus, various nerve block techniques, potential complications, and clinical indications.
Key points of the cervical plexus
- Structure: The cervical plexus consists of sensory and motor branches derived from the anterior rami of cervical nerves C1 to C4.
- Divisions: It has superficial (sensory) and deep (motor) branches.
- Innervation: Provides sensory innervation to the neck and upper anterior torso and motor innervation to neck muscles.
- Applications: Used in various medical procedures, including regional anesthesia for surgeries involving the neck, clavicle, or shoulder.
Anatomy of the cervical plexus
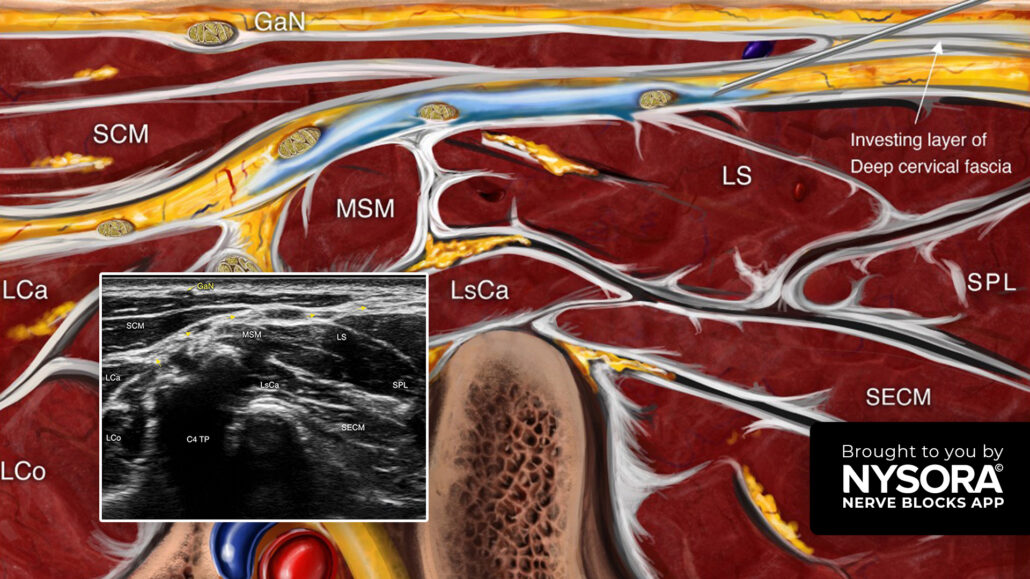
Cervical fascia
The cervical plexus lies within the neck, surrounded by layers of cervical fascia that protect and compartmentalize vital structures:
- Superficial cervical fascia: Contains the platysma muscle, superficial veins, and lymph nodes.
- Deep cervical fascia: Includes the investing, pretracheal, prevertebral layers, and the carotid sheath.
Branches of the cervical plexus
- Superficial branches: Primarily sensory, supplying skin over the neck and parts of the head and shoulder.
- Lesser Occipital Nerve (C2)
- Great Auricular Nerve (C2-C3)
- Transverse Cervical Nerve (C2-C3)
- Supraclavicular Nerves (C3-C4)
- Deep branches: Mostly motor, innervating neck muscles.
- Includes connections with the phrenic nerve (C3-C5), which innervates the diaphragm.
Regional anesthesia techniques
Superficial cervical plexus block
- Targets the sensory branches of the cervical plexus.
- Performed using either anatomical landmarks or ultrasound guidance.
- Injection along the posterior border of the sternocleidomastoid muscle creates a “sausage-like” local anesthetic distribution.
Deep cervical plexus block
- Used for motor block or combined sensory-motor block.
- Traditional techniques include:
- Posterior approach: Needle insertion through extensor muscles of the neck (less commonly used due to patient discomfort).
- Lateral approach: Needle insertion at the transverse processes of C2-C4 vertebrae.
- Ultrasound guidance enhances safety and precision.
Intermediate cervical plexus block
- This block was introduced more recently, and targets the fascial plane between the sternocleidomastoid and prevertebral muscles.
- Reduces risks associated with deeper structures.
Complications of cervical plexus blocks
While effective, cervical plexus blocks carry some risks, including:
- Infection: Minimized by strict aseptic technique.
- Hematoma Formation: Particularly in patients with coagulopathies.
- Nerve Injury: Avoided through careful needle handling and low-pressure injections.
- Specific risks of deep blocks:
- Phrenic nerve palsy, causing diaphragmatic paralysis.
- Accidental intravascular injection or subarachnoid placement.
- Horner’s syndrome due to sympathetic chain involvement.
Clinical indications
Cervical plexus blocks are versatile and widely used in medical practice:
- Surgical procedures:
- Carotid endarterectomy
- Thyroidectomy
- Cervical discectomy and fusion
- Pain management:
- Postoperative analgesia for surgeries involving the neck or clavicle.
- Emergency management of painful clavicle fractures.
- Catheter insertion:
- Enhances patient comfort during internal jugular vein catheterization.
Conclusion
The cervical plexus is a critical anatomical structure with significant applications in anesthesia and pain management. Ultrasound guidance has improved the safety and efficacy of cervical plexus blocks, making them indispensable in modern clinical practice. Understanding the anatomy and techniques associated with the cervical plexus is vital for healthcare professionals who perform surgical anesthesia, pain relief, or other interventions.
For more information, refer to the full article in BJA Education.
Jarvis MS, Sundara Rajan R, Roberts AM. The cervical plexus. BJA Educ. 2023 Feb;23(2):46-51. doi: 10.1016/j.bjae.2022.11.008.
Step-by-step: Three key steps for performing a cervical plexus block
- Place the transducer transversely over the lateral aspect of the neck to identify the sternocleidomastoid muscle (SCM).
- The superficial branches of the cervical branches are located under the SCM.
- Insert the needle in-plane, behind the posterior border of the SCM, and inject 5-8 mL of local anesthetic between the fascial layers containing the branches of the cervical plexus.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!