Tips for an Intercostal Nerve Block
Pain management in thoracic surgery is a critical aspect of postoperative care. Thoracic surgeries, including thoracotomy and video-assisted thoracoscopic surgery (VATS), are known for causing severe postoperative pain, which can lead to complications if not adequately managed. Intercostal nerve block has emerged as a viable analgesic method to address pain following these procedures. A 2021 systematic review and meta-analysis of Guerra-Londono et al. examined the efficacy and safety of intercostal nerve block in thoracic surgery, comparing it to other common pain management techniques such as thoracic epidural analgesia, paravertebral block, and systemic analgesia.
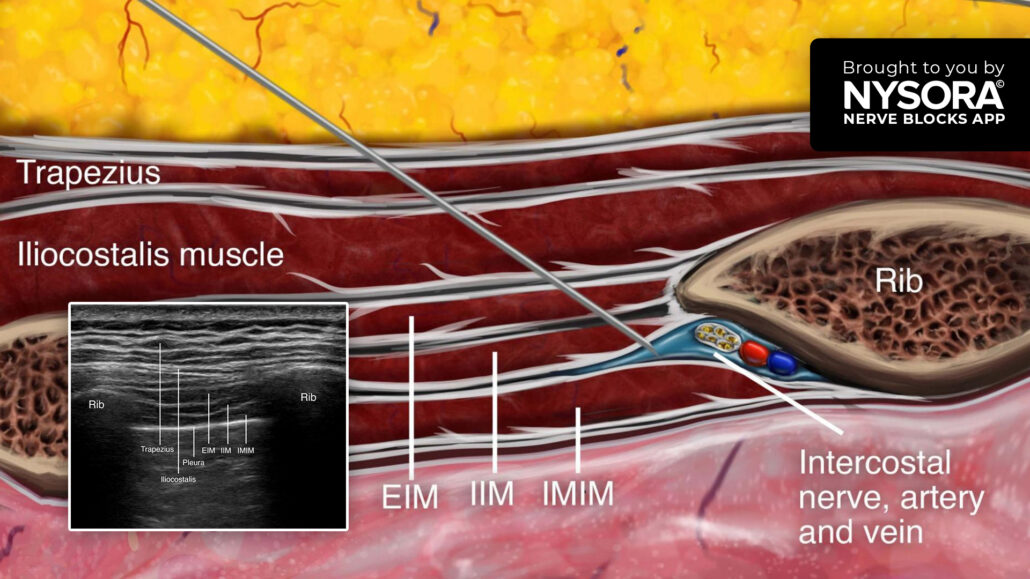
What is an intercostal nerve block?
An intercostal nerve block is a regional anesthesia technique that injects a local anesthetic near the intercostal nerves, transmitting pain signals from the thorax. It can be administered as a single injection or through continuous infusion.
An intercostal nerve block provides analgesia for rib fractures, postsurgical analgesia for chest and upper abdominal surgery (e.g., thoracotomy, thoracostomy, mastectomy, gastrostomy, and cholecystectomy), herpes zoster, or post-herpetic neuralgia.
Key findings
This comprehensive meta-analysis incorporated data from 66 studies involving over 5,000 patients who underwent various forms of thoracic surgery. Here are the main outcomes regarding intercostal nerve block’s effectiveness and safety:
- Pain reduction: Compared to systemic analgesia, intercostal nerve block significantly reduced static and dynamic pain, particularly in the first 24 hours post-surgery. Patients who received an intercostal nerve block experienced lower pain scores, which were clinically relevant, defined as a decrease of at least one point on a 10-point pain scale.
- Opioid consumption: Intercostal nerve block also showed opioid-sparing effects. At 48 hours post-surgery, patients who received an intercostal nerve block required significantly fewer opioids than those relying solely on systemic analgesia.
- Comparison with other techniques: While intercostal nerve block effectively reduced pain, its analgesic effects were slightly inferior to Thoracic epidural analgesia and paravertebral block, considered the gold standard for thoracic surgery pain management. However, due to patient-specific factors, intercostal nerve block may still be preferred when thoracic epidural analgesia or paravertebral block are contraindicated.
Intercostal nerve block vs. systemic analgesia
Systemic analgesia, which typically involves the use of intravenous opioids, is a common approach to managing postoperative pain. However, opioids are associated with a range of adverse effects, including nausea, vomiting, sedation, and respiratory depression. Intercostal nerve block offers a regional approach that minimizes these systemic effects by targeting the nerves responsible for pain at the surgical site.
- Lower pain scores: The meta-analysis revealed that patients receiving an intercostal nerve block had significantly lower pain scores than those receiving only systemic analgesia during the first 24 hours after surgery.
- Reduced opioid use: Intercostal nerve block also reduced the need for opioids by an average of 10.97 MMEs within the first 48 hours, offering a safer alternative for pain control in patients who may be at risk of opioid-related complications.
Intercostal nerve block vs. thoracic epidural analgesia and paravertebral block
Thoracic epidural anesthesia and paravertebral block are commonly used regional anesthesia techniques for managing postoperative pain in thoracic surgery. Both techniques provide effective pain relief but require more complex catheter-based administration than intercostal nerve block.
- Comparable pain relief: The meta-analysis found that intercostal nerve block was noninferior to thoracic epidural analgesia regarding dynamic pain reduction at 7-24 hours post-surgery. However, paravertebral block showed marginally superior pain control compared to intercostal nerve block during this period.
- Opioid consumption: intercostal nerve block was associated with greater opioid consumption compared to thoracic epidural anesthesia, which is known for its powerful opioid-sparing effects. However, the difference was not clinically prohibitive, making intercostal nerve block a valuable alternative for patients who may not be candidates for thoracic epidural analgesia or paravertebral block.
Safety and complications
The meta-analysis also reviewed the safety of intercostal nerve block in thoracic surgery:
- Low risk of complications: intercostal nerve block was associated with a low rate of complications and side effects, especially when compared to systemic analgesia. Common complications related to epidural and paravertebral blocks, such as hypotension and urinary retention, were less prevalent with intercostal nerve block .
- Faster recovery: Patients receiving intercostal nerve block were able to mobilize sooner postoperatively due to the effective pain control and lower incidence of opioid-related side effects such as drowsiness and respiratory depression.
Clinical implications and considerations
An intercostal nerve block provides a significant pain management strategy, particularly in cases where thoracic epidural analgesia or paravertebral block are not indicated. Here are the main considerations for clinical practice:
- Patient selection: intercostal nerve block is beneficial for patients at risk of complications from more invasive procedures like thoracic epidural analgesia or those with contraindications for systemic opioids.
- Simplicity of administration: Compared to thoracic epidural analgesia and paravertebral block, intercostal nerve block can be administered more easily. This makes it an attractive option where resources or expertise for catheter-based techniques may be limited.
- Multimodal analgesia: The intercostal nerve block should be considered part of a multimodal approach to pain management, which may include systemic analgesics and other non-opioid medications to reduce pain further and enhance recovery.
Conclusion
The intercostal nerve block offers a safe, effective, and opioid-sparing alternative for postoperative pain management in thoracic surgery. While its pain control is slightly inferior to that of thoracic epidural analgesia and paravertebral block, intercostal nerve block remains a valuable option, particularly for patients for whom these more invasive techniques are not feasible.
For more information, refer to the full article in JAMA.
Guerra-Londono CE, Privorotskiy A, Cozowicz C, et al. Assessment of Intercostal Nerve Block Analgesia for Thoracic Surgery: A Systematic Review and Meta-analysis. JAMA Netw Open. 2021;4(11):e2133394. doi:10.1001/jamanetworkopen.2021.33394
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!