Exploring the role of liposomal bupivacaine in supraclavicular brachial plexus blocks
The supraclavicular approach blocks the brachial plexus from the distal trunks to the proximal cords or at the level of the brachial plexus divisions. This block is used for analgesia in upper extremity surgeries. The block was first introduced in 1911 by Kulenkampff as a landmark-based approach and popularized by Dr. Alon Winnie in the 1970s. Kapral and colleagues re-invented the block using ultrasound to decrease the risk of pneumothorax and intravascular injection. The technique is very reliable, and also known as the “spinal anesthesia of the upper extremities.”
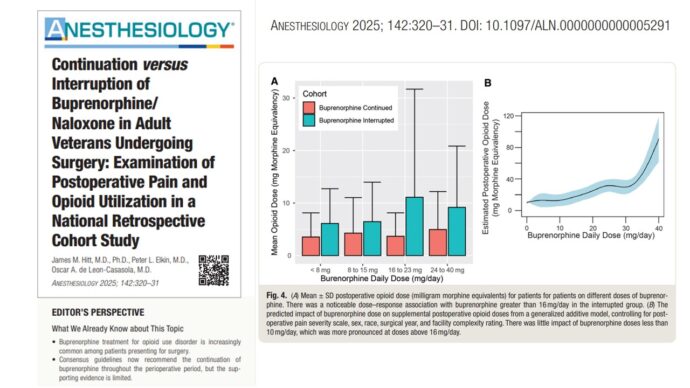
A recent randomized controlled trial published in Anesthesiology investigated the efficacy of adding liposomal bupivacaine to standard bupivacaine in supraclavicular brachial plexus blocks. This study could redefine pain management strategies for patients undergoing distal radial fracture surgery.
Background
Brachial plexus blocks are widely used to deliver regional anesthesia for upper limb surgeries. However, their utility is limited by the short duration of single-injection nerve blocks, leading to rebound pain after 24 hours. Liposomal bupivacaine, an extended-release formulation, has shown promise in prolonging analgesia in other applications. This trial sought to explore its effects when combined with standard bupivacaine for distal radial fracture surgery.
Study design and methodology
- Participants: 80 adult patients scheduled for distal radial fracture fixation.
- Groups:
- Liposomal Bupivacaine Group: Received 10 mL 0.5% plain bupivacaine plus 10 mL 1.33% liposomal bupivacaine.
- Standard Bupivacaine Group: Received 20 mL 0.5% plain bupivacaine.
- Blinding: Both patients and outcome assessors were blinded.
- Primary Outcome: Weighted area under the curve (AUC) of numerical pain scores at rest over the first 48 hours post-surgery.
- Secondary Outcomes: Pain with movement, oxycodone consumption, and quality of recovery scores were included.
Key findings
Primary outcome
- Pain scores at rest over 48 hours were significantly lower in the liposomal bupivacaine group (mean AUC: 0.6) compared to the standard bupivacaine group (mean AUC: 1.4; p < 0.001).
Secondary outcomes
- Pain with movement: Patients in the liposomal group reported reduced pain during movement in the first 48 hours (AUC: 2.3 vs. 3.7; p < 0.001).
- Overall benefit with analgesia score: Liposomal bupivacaine showed statistically significant improvement (AUC: 1.1 vs. 1.7; p = 0.02).
- No significant differences in oxycodone consumption, recovery quality, and sleep disturbance.
Short-Term insights
- The most substantial benefit was observed on postoperative day 1.
- Pain reduction was not statistically significant from postoperative days 2 to 7.
Clinical implications
- Enhanced acute pain relief: Liposomal bupivacaine provides superior pain control during the critical early postoperative phase.
- Comparable safety profile: No significant differences in adverse effects, such as respiratory impairment or motor dysfunction.
- Targeted use xases: Particularly beneficial for patients at high risk for rebound pain or prolonged postoperative discomfort.
Challenges and limitations
- Limited long-term efficacy: Benefits did not extend beyond the first postoperative day.
- Off-label use: The application of liposomal bupivacaine in supraclavicular blocks is not FDA-approved.
- Potential cost considerations: Its use may be more justifiable in patients at higher risk of severe postoperative pain.
Future directions
The findings highlight the potential for liposomal bupivacaine to reshape postoperative pain management strategies, especially in surgeries requiring regional anesthesia. Further studies should focus on:
- Identifying high-risk groups: Exploring its effectiveness in patients predisposed to severe rebound or chronic pain.
- Functional outcomes: Assessing its impact on recovery metrics such as mobility and quality of life.
Conclusion
This “spinal anesthesia of the upper extremities” continues to set new standards for patient care, as evidenced by the recent integration of liposomal bupivacaine. The findings of the study not only underscore the block’s effectiveness in reducing acute postoperative pain but also highlight its safety and reliability.
For more information, refer to the article in Anesthesiology.
Chan TCW, Wong JSH, Wang F, Fang CX, Yung CS, Chan MTH, Chan WSH, Wong SSC. Addition of Liposomal Bupivacaine to Standard Bupivacaine versus Standard Bupivacaine Alone in the Supraclavicular Brachial Plexus Block: A Randomized Controlled Trial. Anesthesiology. 2024 Oct 1;141(4):732-744.
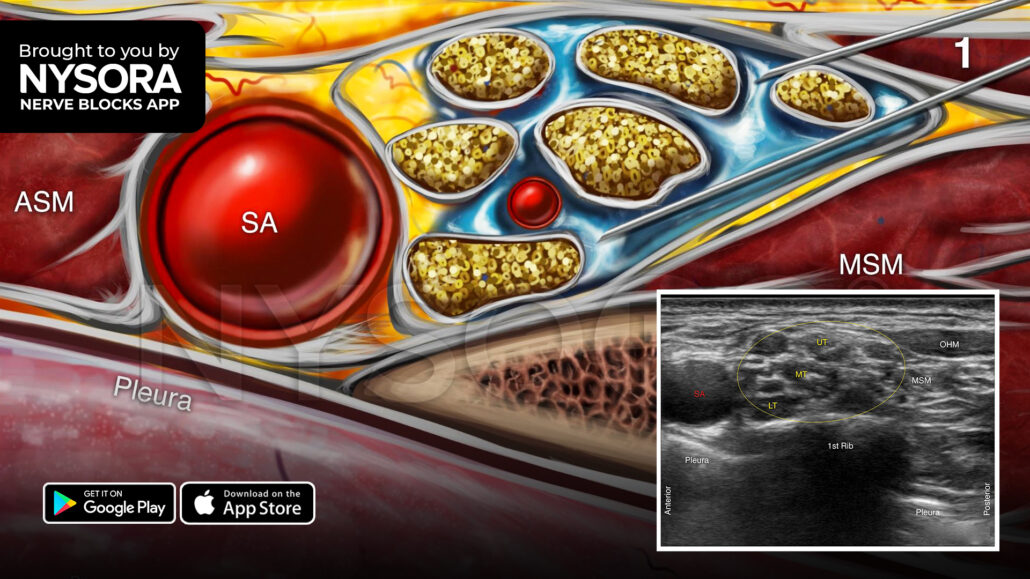
Here are 3 tips to successfully perform a supraclavicular brachial plexus block
- The initial insertion of the needle should not be deeper than 1 cm since the brachial plexus is shallow at this location.
- Visualize the needle path at all times to reduce the risk of pneumothorax.
- The neck is highly vascular, so use the color Doppler to detect any large vessels (i.e., dorsal scapular artery, transverse cervical artery, suprascapular artery) in the needle path.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!