Learning objectives
- Describe hypoparathyroidism
- Recognize the symptoms and signs of hypocalcemia, related to hypoparathyroidism
- Anesthetic management of a patient with hypoparathyroidism
Definition and mechanisms
- Hypoparathyroidism is a condition in which the parathyroid glands do not produce enough parathyroid hormone (PTH)
- PTH plays an important role in maintaining normal calcium homeostasis
- The main effector sites responding directly or indirectly to PTH are the intestines, kidneys, and bone
- Hypoparathyroidism ultimately results in hypocalcemia and hyperphosphatemia
Classification
- Acquired hypoparathyroidism: Develops after the removal of, or trauma to, the parathyroid glands due to thyroid surgery (thyroidectomy), parathyroid surgery (parathyroidectomy), or other surgical interventions in the central part of the neck (i.e., chemotherapy or radiation); hypomagnesemia
- Autoimmune hypoparathyroidism: The immune system mistakenly attacks the parathyroid glands or PTH
- Congenital hypoparathyroidism: Occurs at birth resulting from gene mutations or if someone is born without parathyroid glands (i.e., DiGeorge syndrome)
- Familial (inherited) hypoparathyroidism: Genetically passed down from family
Signs and symptoms
The symptoms of hypoparathyroidism are caused by hypocalcemia:
- Acute: Perioral paresthesia, restlessness, neuromuscular irritability, and stridor
- Chronic: Fatigue, muscle cramps, severe spasms (tetany), lethargy, personality changes, and cerebral defects
Neuromuscular signs:
- Positive Chvostek sign: Facial contracture elicited by tapping the facial nerve
- Positive Trousseau sign: Fingers and wrist contracture elicited by inflation of a blood pressure cuff above the patient’s systolic blood pressure for ≥3 minutes
Complications
- Seizures
- Hypotension
- QT prolongation and arrhythmias
- Congestive heart failure
- Bronchospasm, laryngospasm, and resulting respiratory failure
- Problems with kidney function (e.g., kidney stones and chronic kidney failure) due to treatment with calcium and vitamin D supplements
- Hardening and changes in the shape of the bones, and poor growth
- Delayed mental development in children
- Clouded vision due to cataracts
Risk factors
- Recent neck surgery, particularly if the thyroid was involved
- Family history
- Certain autoimmune or endocrine conditions (e.g., Addison’s disease)
Pathophysiology
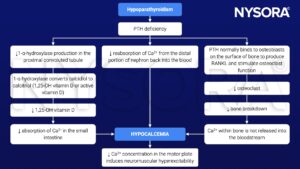
Treatment
- Acute hypocalcemia: IV infusion of calcium (e.g., calcium chloride or calcium gluconate) until the neuromuscular irritability resolves
- Chronic hypocalcemia: Oral calcium and vitamin D supplements
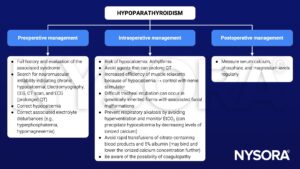
Management
Suggested reading
- Hypoparathyroidism. In: Bissonnette B, Luginbuehl I, Marciniak B, Dalens BJ. eds. Syndromes: Rapid Recognition and Perioperative Implications. McGraw Hill; 2006. Accessed March 06, 2023. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=852§ionid=49517707
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com