Hiroaki Murata, Tatsuo Nakamoto, Takayuki Yoshida, and Manoj K. Karmakar
INTRODUCTION
Traditionally, lumbar plexus block (LPB) is performed using surface anatomical landmarks to identify the site for needle insertion and eliciting quadriceps muscle contraction in response to nerve electro-localization, as described in the nerve stimulator-guided chapter. The main challenges in accomplishing LPB relate to the depth at which the lumbar plexus is located and the size of the plexus, which requires a large volume of local anesthetic for success. Due to the deep anatomical location of the lumbar plexus, small errors in landmark estimation or angle miscalculations during needle advancement can result in needle placement away from the plexus or at unwanted locations. Therefore, monitoring the needle path and final needle tip placement should increase the precision of the needle placement and the delivery of local anesthetic. Although computed tomography and fluoroscopy can be used to increase precision during LPB, these technologies are impractical in the busy operating room environment, costly, and associated with radiation exposure. It is only logical, then, that ultrasound (US)-guided LPB be of interest because of the ever-increasing availability of portable machines and the improvement in the quality of the images obtained.
ANATOMY AND GENERAL CONSIDERATIONS
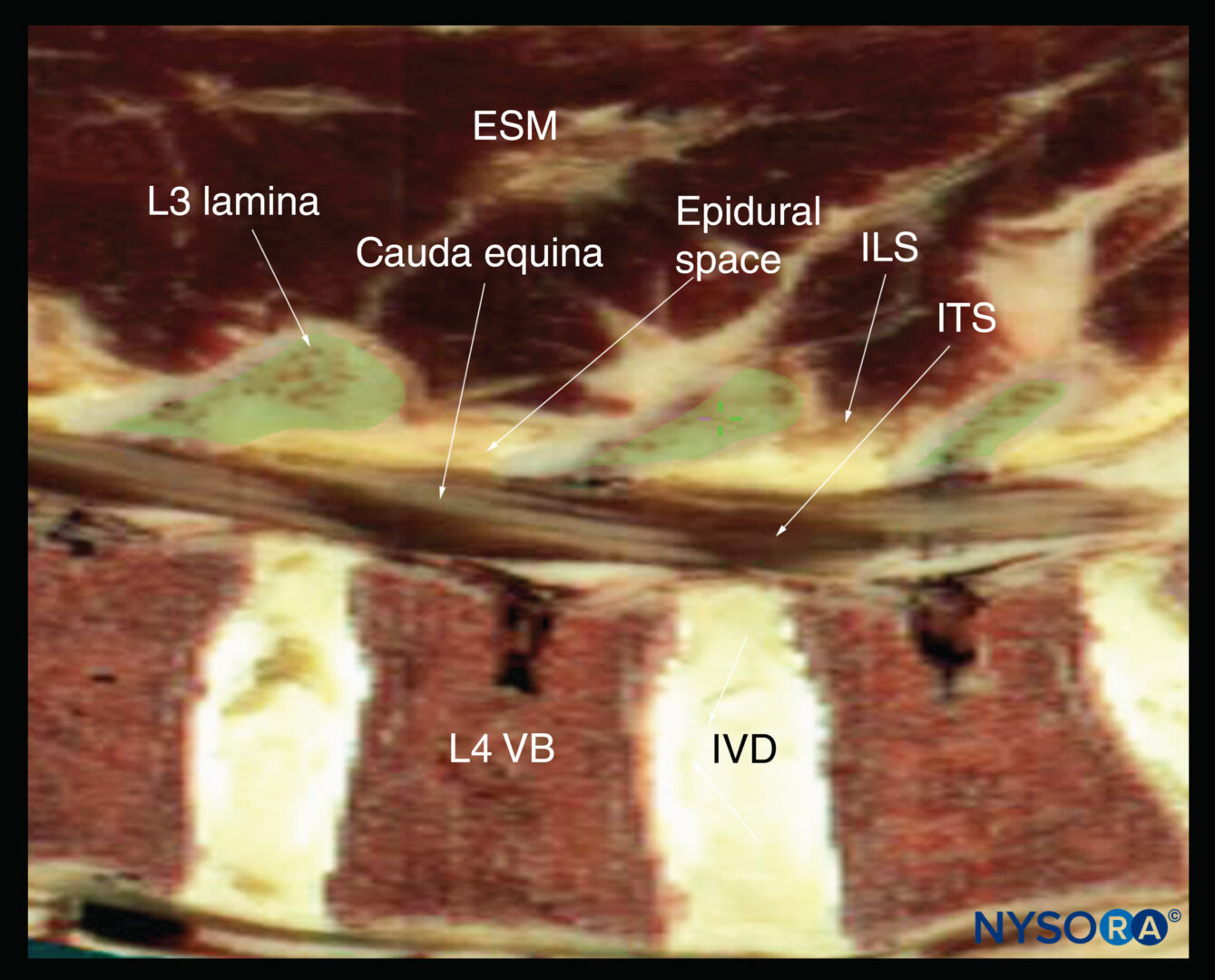
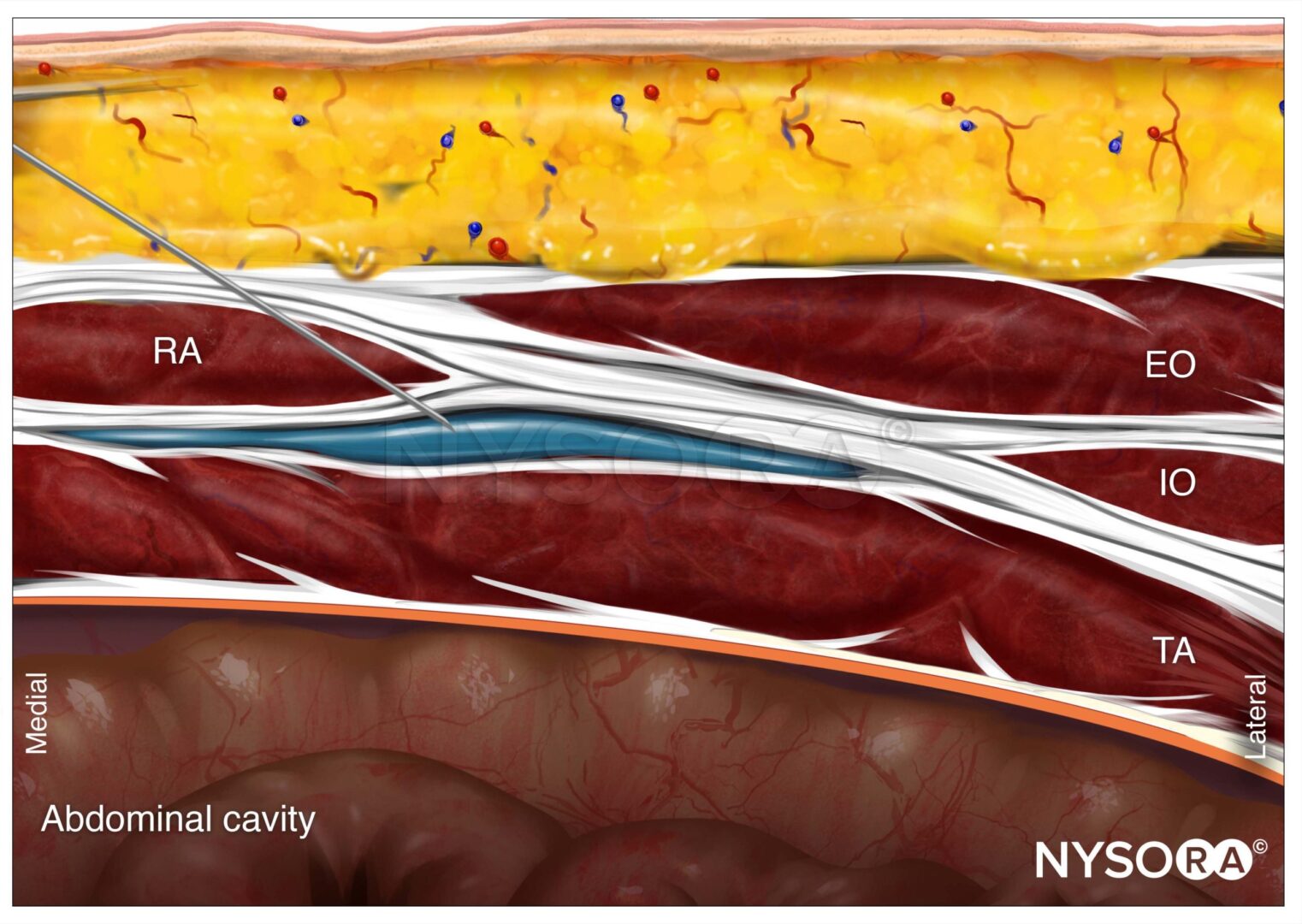
LPB, also known as psoas compartment block, comprises injection of local anesthetic in the fascial plane within the posterior aspect of the psoas major muscle, usually at the L3–4 level (occasionally at the L2–3 or L4–5 levels). Because the roots of the lumbar plexus are located in this plane, an injection of a sufficient volume of local anesthetic in the posteromedial compartment of the psoas muscle results in a block of the majority of the plexus (the femoral nerve, lateral femoral cutaneous nerve, and obturator nerve). The anterior boundary of the fascial plane that contains the lumbar plexus is formed by the fascia between the anterior two-thirds of the compartment of the psoas muscle that originates from the anterolateral aspect of the vertebral body and the posterior one-third of the muscle that originates from the anterior aspect of the transverse processes. The lateral and dorsal borders of the psoas major muscle consist of the quadratus lumborum muscle and the erector spinae muscle, respectively. Considering the rich vascularity of the lumbar paravertebral area, such as the dorsal branch of the lumbar artery, the use of smaller-gauge needles and the avoidance of this block in patients on anticoagulants are prudent. LPB in patients with obesity can be challenging.
For additional information follow the link to Lumbar Paravertebral Sonography
TRANSVERSE IN-PLANE TECHNIQUE
Regardless of technique, the patient is placed in the lateral decubitus position with the side to be blocked uppermost. The operator should identify the transverse processes on a longitudinal sonogram (Figure 1a, b, c). One technique involves identifying the flat surface of the sacrum and then scanning proximally until the intervertebral space between L5 and S1 is recognized as an interruption of the sacral line continuity (Figure 1b). Once the operator identifies the L5 transverse process, the transverse processes of the other lumbar vertebrae are easily identified by a dynamic cephalad scan in ascending order (Figure 1c, d).
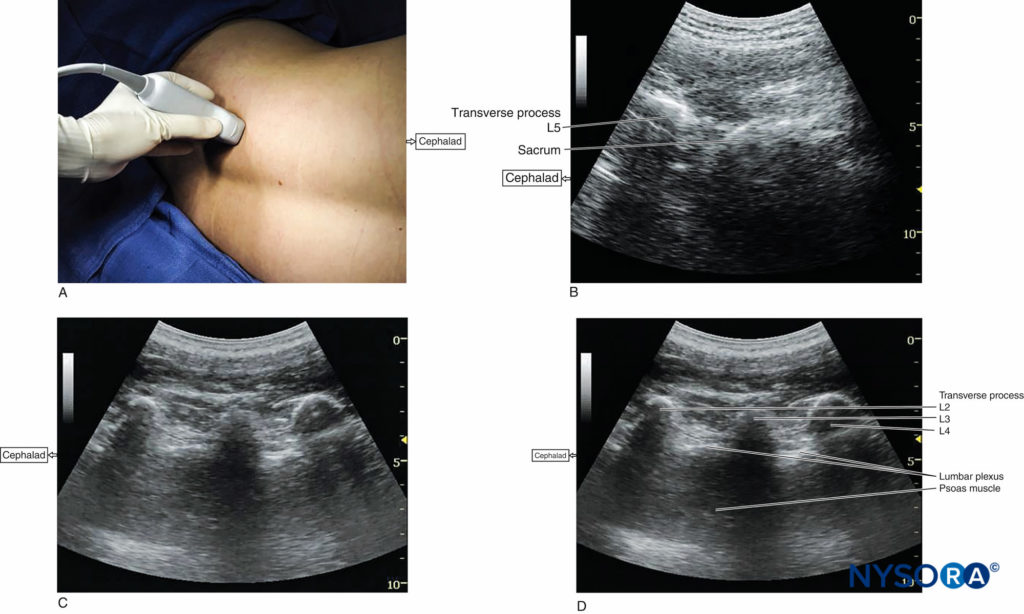
FIGURE 1. (A) Transducer position to image the longitudinal lumbar paravertebral space including the transverse processes. Lumbar plexus block can be performed with this transducer position using both out-of-plane and in-plane approaches (see also Figure 4a). (B) Longitudinal US image of the lumbar paravertebral space demonstrating the sacrum and L5 transverse process. When the surface of the sacrum disappears, the next osseous structure is the L5 transverse process. (C) US anatomy of the lumbar paravertebral space demonstrating transverse processes at a depth of approximately 3 cm. The acoustic shadows of the transverse processes look like a trident. A lower-frequency, curved array transducer is used to optimize imaging at this deep location and obtain a greater angular view. (D) Labeled US image of Figure 1C.
The following settings are typically used to start the scanning:
- Abdominal preset or nerve preset if available
- Depth: 9–12 cm
- Curved array transducer (4–8 MHz)
- Tissue harmonic imaging and compound imaging functions engaged when available
- Adjustment of the overall gain and time-gain compensation
Learn more about Optimizing an Ultrasound Image.
The transducer is positioned approximately 4 cm lateral from the midline at the level just cephalad to the iliac crest and directed slightly medially to assume a transverse oblique orientation (Figure 2a). This approach allows imaging of the lumbar paravertebral region with the psoas major, erector spinae, and quadratus lumborum muscles; the vertebral lamina; and the anterolateral surface of the vertebral body (Figure 2b, c, d). In this view, the psoas major muscle appears slightly hypoechoic with multiple hyperechoic striations within. The inferior vena cava on the right-sided scan (Figure 2e) or the abdominal aorta on the left-sided scan can be seen deep to the psoas major muscle, providing additional information regarding the location of the psoas major muscle, which is positioned superficial to these vessels. When scanning at the L2–L4 level, the lower pole of the kidney can be seen as an oval structure that ascends and descends with respirations (see Figure 2e).
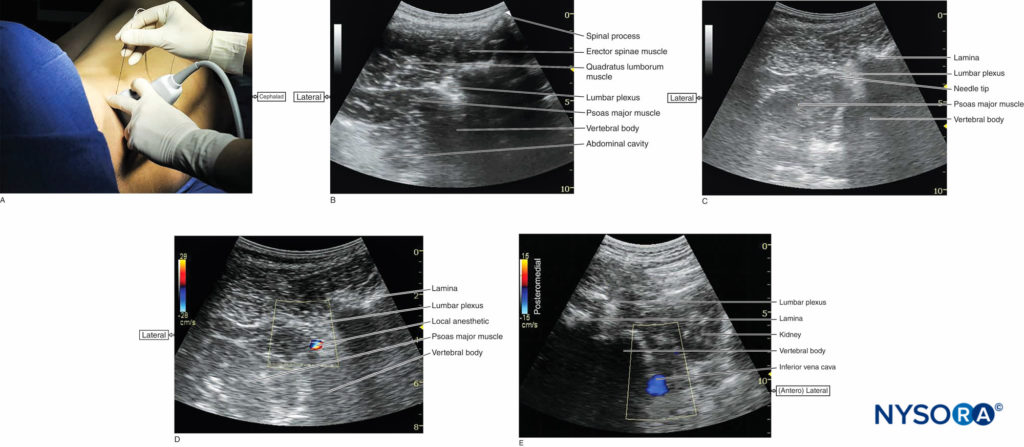
FIGURE 2. (A) Transducer position and needle insertion point to accomplish US-guided lumbar plexus block in the transverse oblique view using an in-plane approach. (B) US anatomy of the lumbar paravertebral space in the transverse oblique view. The lumbar plexus root is seen just below the lamina as it exits the interlaminar space and enters into the posteromedial aspect of the psoas major muscle. (C) Needle path in US-guided lumbar plexus block using a transverse oblique view and in-plane approach from the lateral to medial direction. (D) Spread of local anesthetic solution with lumbar plexus block injection. Due to the deep location of the plexus, local anesthetic spread may not always be well seen. Color Doppler imaging can be used to help determine the location of the njectate. (E) Transverse image of the right-side lumbar paravertebral space. Color Doppler US captures the flow in the inferior vena cava. The right kidney is also seen.
The key to obtaining adequate images of the psoas major muscle and lumbar plexus with the transverse oblique scan is to insonate between two adjacent transverse processes (the lumbar intertransverse space). This scanning method avoids the acoustic shadow of the transverse processes, which obscures the underlying psoas major muscle and the intervertebral foramen (angle between the transverse process and vertebral body), and also allows visualization of the articular process of the facet joint. Because the intervertebral foramen is located at the angle between the articular process of the facet joint and vertebral body, lumbar nerve roots can be depicted. The needle can be inserted laterally or medially to the transducer and advanced toward the posterior aspect of the psoas major muscle until either contact of the needle with the lumbar plexus is seen or an ipsilateral quadriceps muscle contraction is elicited. Local anesthetic injection into the lumbar paravertebral area should be performed without excessive force because high injection pressure can lead to unwanted epidural spread and/or rapid intravascular injection.
Recently, the “shamrock method” has become considered one of the standard approaches for US-guided LPB. In this method, the transducer is placed transversely in the abdominal flank adjacent to the iliac crest (Figure 3a). A shape like a shamrock with three leaves can be seen with the psoas major muscle anteriorly, the erector spinae muscle posteriorly, and the quadratus lumborum muscle at the apex of the transverse process (Figure 3b). The lumber plexus can be identified as a hyperechoic oval structure in the posteromedial compartment of the psoas major muscle near the transverse process. By tilting the transducer caudally, the L3 transverse process disappears from the US image, which permits an in-plane posteroanterior needle approach (Figure 3c). The needle insertion point is based on the landmark-guided method; that is, approximately 4 cm lateral to the midline or at the junction of the lateral third and medial two-thirds of a line between the spinous process of L4 and a line parallel to the spinal column passing through the posterior superior iliac spine. The needle insertion point can be decided by an ultrasonographical estimation of the distance from the bottom of the transducer to the posteromedial quadrant of the psoas major muscle, where the lumbar plexus is expected to locate. Then, the needle is advanced anteriorly under US guidance until the needle tip reaches to the lumbar plexus or an appropriate muscle twitch is observed. In this view, the inferior vena cava and abdominal aorta can be seen simultaneously anterior to the vertebral body (Figure 3d).
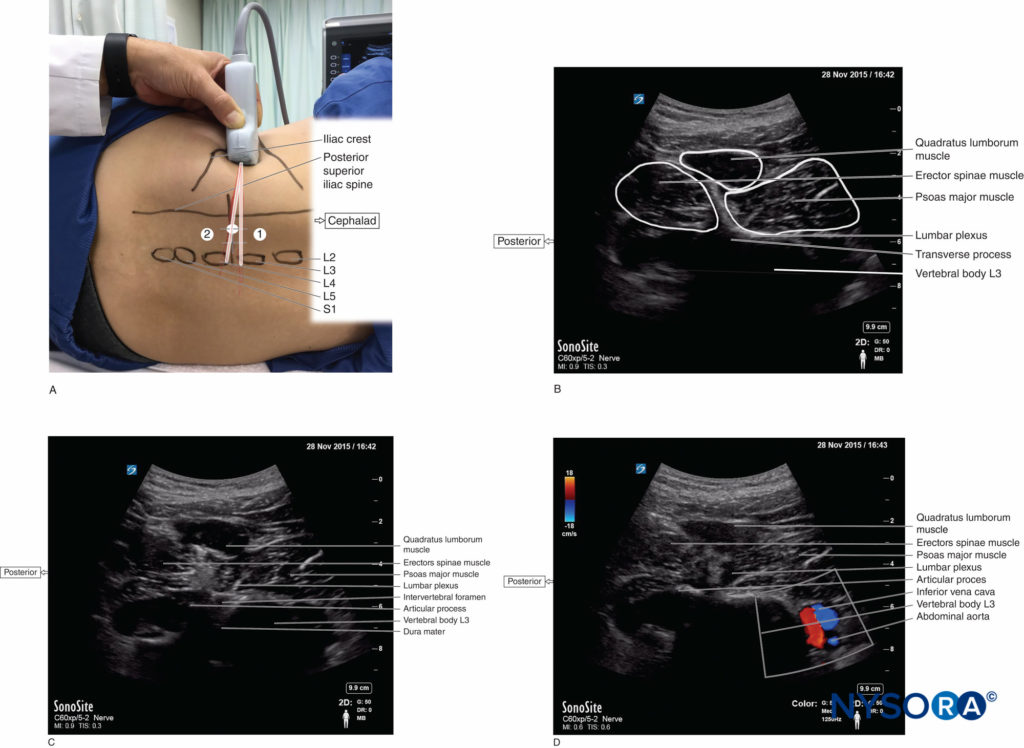
FIGURE 3. (A) Transducer position and needle insertion point to accomplish US-guided lumbar plexus block with the shamrock method using an in-plane approach. The transducer is placed transversely in the left side of the abdominal flank adjacent to the iliac crest to image the “shamrock” with the transverse process (1). By tilting the transducer (2), the transverse process disappears from the US image, which permits an in-plane posteroanterior needle approach. (B) US anatomy of the right lumbar paravertebral region at the level of the L3 transverse process in the shamrock view. A shape that looks like a shamrock with three leaves consists of the erector spinae, quadratus lumborum, and psoas major muscles and the transverse process. (Continued) (C) US anatomy of the right lumbar paravertebral region just caudal to the L3 transvers process (lumbar intertransverse space in the shamrock view). The lumbar plexus root is seen just lateral to the intervertebral foramen. The dura mater is confirmed as a hyperechoic line in the spinal canal through the intervertebral foramen. (D) The abdominal aorta and inferior vena cava are confirmed by color Doppler anterior to the vertebral body at the lumbar intertransverse space in the right-side shamrock view.
The shamrock method has been reported to have several advantages over US-guided LPB using paramedian transverse scan. First, the needle trajectory is almost the same as in the traditional landmark-guided LPB, which means that this method simply adds ultrasonographical information to the landmark-guided LPB approach. Second, needle can be advanced perpendicularly to the US beam, which allows for a clearer visualization of the needle.
LONGITUDINAL OUT-OF-PLANE AND IN-PLANE TECHNIQUES
In the parasagittal longitudinal US image, the acoustic shadow of the transverse process has a characteristic appearance, referred to as the “trident sign” (see Figure 1c,d).
Once the transverse processes are recognized at approximately 4 cm lateral and parallel to the lumbar spine, to produce a longitudinal scan of the lumbar paravertebral region (Figure 4a), the psoas major muscle is imaged through the acoustic window of the transverse processes.
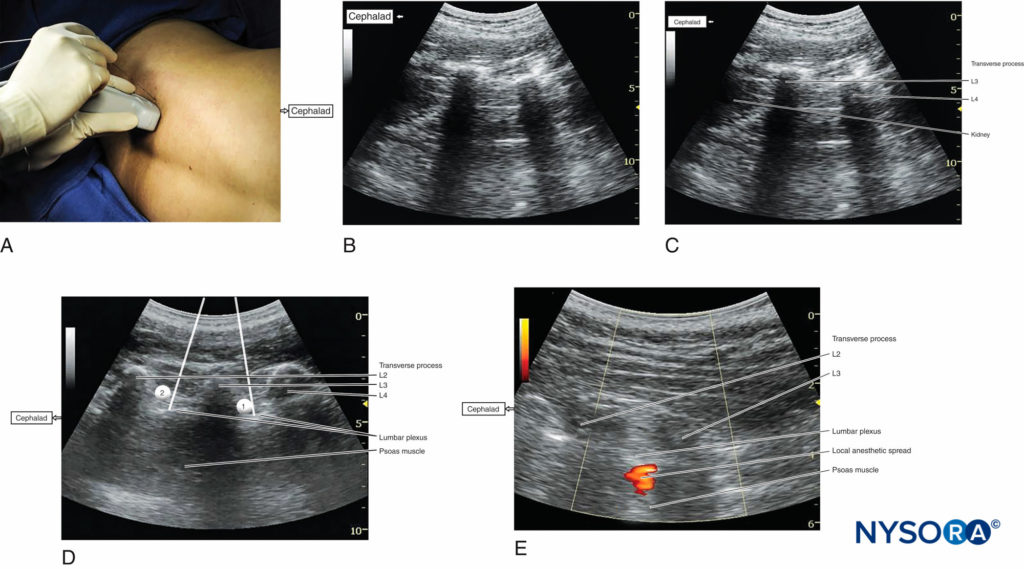
FIGURE 4. (A) Transducer position and needle insertion point to accomplish US-guided lumbar plexus block in the longitudinal parasagittal view using an out-of-plane approach. (B) US anatomy of the longitudinal lumbar paravertebral space at the L2–L3 and L3–L4 levels demonstrating the lower pole of the kidney on the left side of the image at a depth of approximately 5 cm. (C) Labeled US image of Figure 4b. (Continued) (D) Simulated needle insertion paths (1, 2) to inject local anesthetic at two different levels to accomplish a lumbar plexus block using an out-of-plane technique. (E) Local anesthetic disposition during injection into the psoas muscle and the L2–L3 level. The spread of local anesthetic is often not well visualized using two-dimensional imaging.
The psoas muscle appears as a combination of longitudinal hyperechoic striations within a typical hypoechoic muscle appearance just deep to the transverse processes (see Figure 1c,d). Some hyperechoic striations may appear particularly intense and may mislead the operator to interpret them as roots of the lumbar plexus; therefore, the identification of the roots in a longitudinal scan is not reliable without nerve stimulation. This unreliability is partly because intramuscular connective tissues (eg, septa, tendons) within the psoas muscle are thick and may be indistinguishable from the nerve roots at such a deep location.
As the transducer is moved progressively cephalad, the lower pole of the kidney often comes into view as low as the level of L2–L4 (Figure 4b, c). The goal of the technique is to guide the needle through the acoustic window between the transverse processes (between the “teeth” of the “trident”) of L3–L4 or L2–L3 into the posterior part of the psoas major muscle containing the roots of the lumbar plexus.
Both out-of-plane (see Figure 4a) and in-plane approaches can be employed with the parasagittal longitudinal technique. After obtaining ipsilateral quadriceps muscle contractions, local anesthetic is injected (Figures 4d) with real-time visualization of the injection into the posterior part of the psoas major muscle (Figure 4e).
Continue reading: Lumbar Paravertebral Sonography and Considerations for Ultrasound-Guided Lumbar Plexus Block.
REFERENCES
- Sauter AR, Ullensvang K, Niemi G, et al: The Shamrock lumbar plexus block: a dose-finding study. Eur J Anaesthesiol 2015;32:764–770.
- Doi K, Sakura S, Hara K: A modified posterior approach to lumbar plexus block using a transverse ultrasound image and an approach from the lateral border of the transducer. Anaesth Intensive Care 2010;38:213–214.
- Ilfeld BM, Loland VJ, Mariano ER: Prepuncture ultrasound imaging to predict transverse process and lumbar plexus depth for psoas compartment block and perineural catheter insertion: a prospective, observational study. Anesth Analg 2010;110:1725–1728.
- Weller RS, Gerancher JC, Crews JC, Wade KL: Extensive retroperitoneal hematoma without neurologic deficit in two patients who underwent lumbar plexus block and were later anticoagulated. Anesthesiology 2003;98:581–585.
- Narouze S, Benzon HT, Provenzano DA, et al: Interventional spine and pain procedures in patients on antiplatelet and anticoagulant medications: guidelines from the American Society of Regional Anesthesia and Pain
- Medicine, the European Society of Regional Anaesthesia and Pain Therapy, the American Academy of Pain Medicine, the International Neuromodulation Society, the North American Neuromodulation Society, and the World Institute of Pain. Reg Anesth Pain Med 2015;40:182–212.
- Karmakar MK, Li JW, Kwok WH, Hadzic A: Ultrasound-guided lumbar plexus block using a transverse scan through the lumbar intertransverse space: a prospective case series. Reg Anesth Pain Med 2015;40:75–81.
- Karmakar MK, Li JW, Kwok WH, Soh E, Hadzic A: Sonoanatomy relevant for lumbar plexus block in volunteers correlated with crosssectional anatomic and magnetic resonance images. Reg Anesth Pain Med 2013;38:391–397.
- Gadsden JC, Lindenmuth DM, Hadzic A, Xu D, Somasundarum L, Flisinski KA: Lumbar plexus block using high-pressure injection leads to contralateral and epidural spread. Anesthesiology 2008;109:683–688.
- Lin JA, Lu HT, Chen TL: Ultrasound standard for lumbar plexus block. Br J Anaesth 2014;113:188–189.Lin JA, Lu HT: Solution to the challenging part of the Shamrock method during lumbar plexus block. Br J Anaesth 2014;113:516–517.
- Lin JA, Lee YJ, Lu HT: Finding the bulging edge: a modified shamrock lumbar plexus block in average-weight patients. Br J Anaesth 2014;113: 718–720.
- Parkinson SK, Mueller JB, Little WL, Bailey SL: Extent of block with various approaches to the lumbar plexus. Anesth Analg 1989;68: 243–248.
- Capdevila X, Macaire P, Dadure C, et al: Continuous psoas compartment block for postoperative analgesia after total hip arthroplasty: new landmarks, technical guidelines, and clinical evaluation. Anesth Analg 2002;94:1606–1613, table of contents.
- Karmakar MK, Ho AM, Li X, Kwok WH, Tsang K, Ngan Kee WD: Ultrasound-guided lumbar plexus block through the acoustic window of the lumbar ultrasound trident. Br J Anaesth 2008;100:533–537.