Explore NYSORA knowledge base for free:
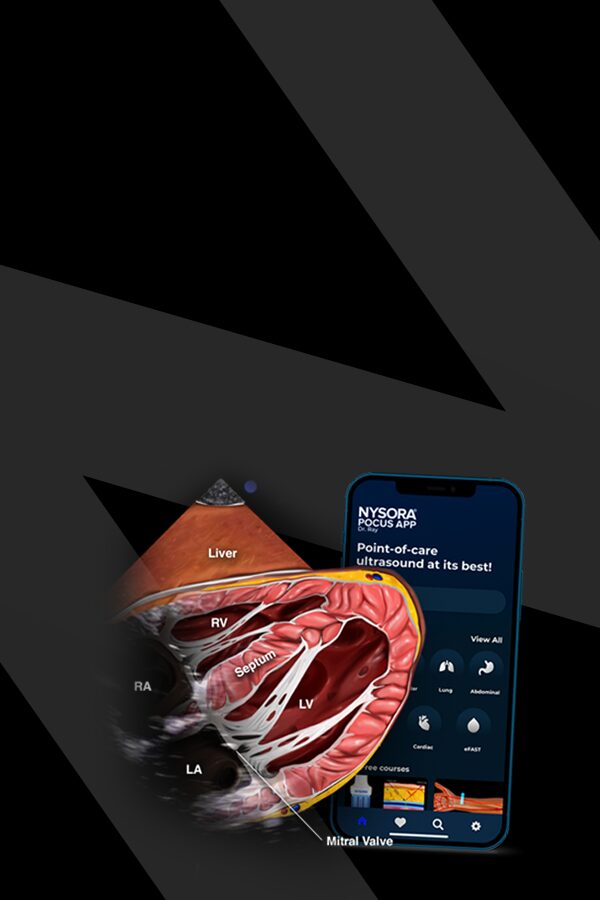
Master your emergency diagnostics skills on the go!

Convenience meets excellence with immersive walkthroughs to the most commonly used POCUS techniques, accompanied by proprietary NYSORA learning aids and clinical pearls.

We recently partnered with Dr. Ray on POCUS. He is an anesthesiologist and critical care physician and he explains that the transition from regional anesthesia into POCUS is a natural step that considerably changes your practice. Therefore, we designed an app together to empower healthcare professionals with advanced guidance on POCUS wherever they go. We sat down with him to discuss POCUS, its history, and NYSORA’s role in the app publication.
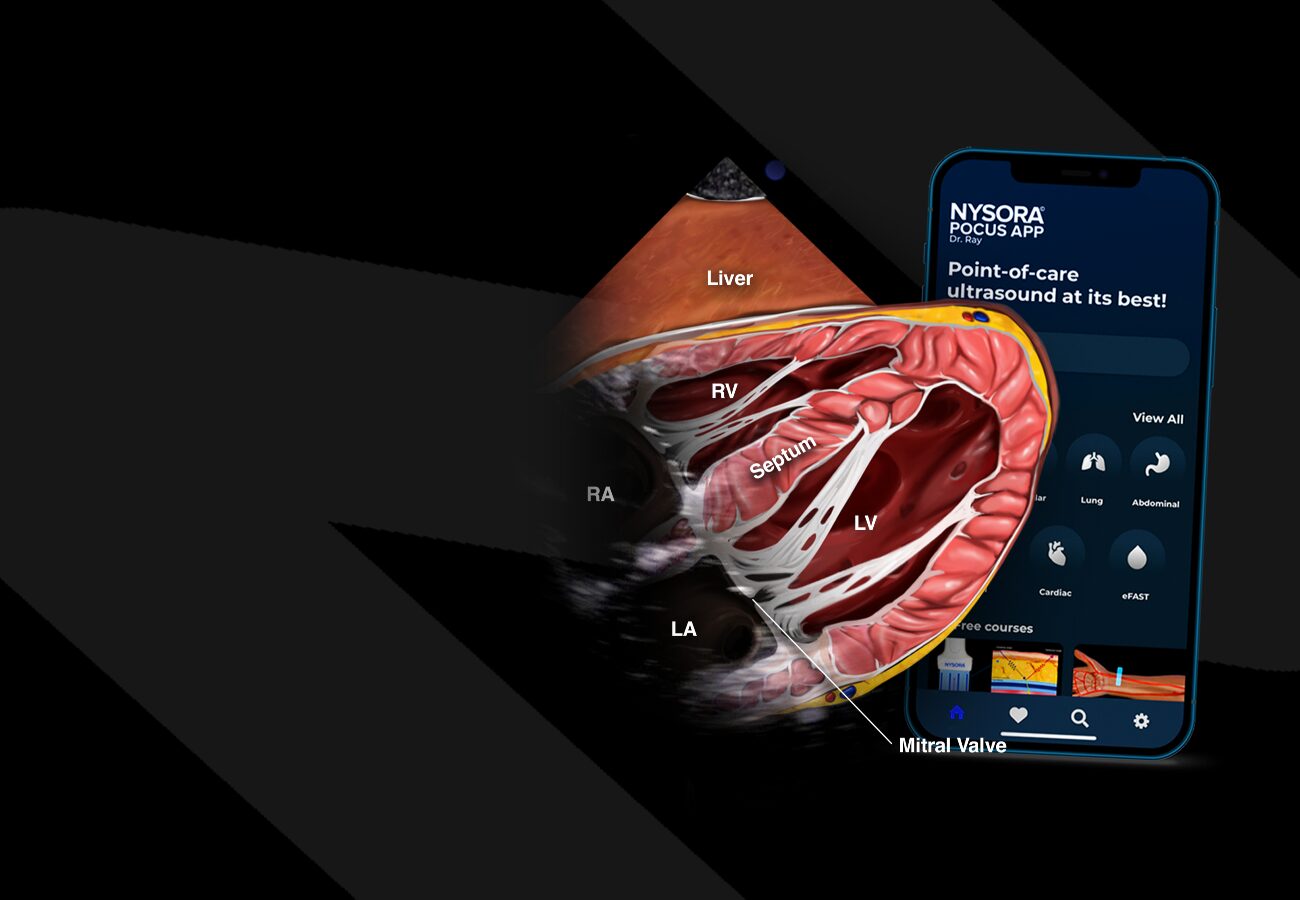
Point-of-care ultrasound (POCUS) refers to the use of (portable) ultrasound devices at the bedside or point of care to provide real-time diagnostic imaging. Unlike traditional ultrasound, which is performed in dedicated imaging departments, POCUS allows healthcare providers to quickly assess patients and guide clinical decision-making directly at the patient’s bedside.
While both ultrasound and point-of-care ultrasound (POCUS) utilize the same imaging technology, they differ in their application and setting. Traditional ultrasound typically involves scheduled appointments in specialized imaging departments, whereas POCUS is performed by healthcare providers directly at the patient’s bedside or point of care to provide immediate diagnostic information and guide treatment decisions in real time.
The objective of point-of-care ultrasound (POCUS) is to facilitate rapid clinical decision-making by providing real-time diagnostic information directly at the patient’s bedside. It allows healthcare providers to quickly assess patients, guide interventions, monitor treatment responses, and expedite patient care, particularly in critical or emergency situations.
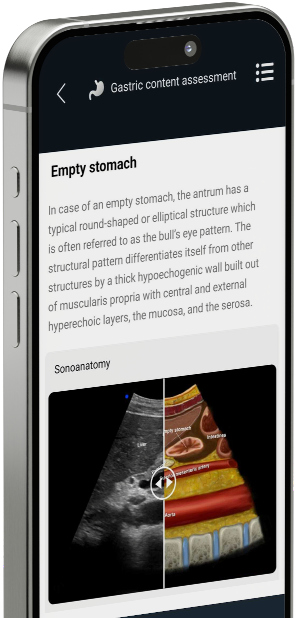
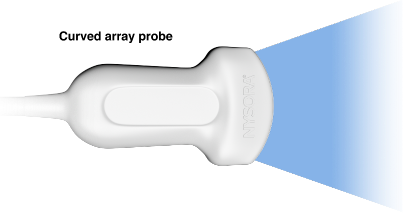
The four main types of ultrasound scanning techniques are:
- B-mode ultrasound: Produces two-dimensional grayscale images to visualize anatomical structures.
- Doppler ultrasound: Assesses blood flow by detecting changes in the frequency of sound waves reflected by moving blood cells.
- Color Doppler ultrasound: Combines B-mode imaging with Doppler technology to visualize blood flow direction and velocity, typically represented in color.
- Power Doppler ultrasound: Is more sensitive in detecting blood flow than color Doppler, but does not provide information on direction and speed of blood flow.
- Spectral Doppler ultrasound: A way to visualize the Doppler principle by means of graphical peaks.
- M-mode ultrasound: Displays motion over time, often used to assess cardiac function and fetal heart rate.
Point-of-care ultrasound (POCUS) can be performed by various healthcare providers, including physicians, nurse practitioners, physician assistants, paramedics, and other trained personnel with appropriate certification or training in ultrasound imaging. Proper education and training are essential to ensure proficiency and safety when performing POCUS.
Point-of-care ultrasound (POCUS) is utilized across various medical specialties to aid in diagnosis, treatment, and patient management. Some specialties that commonly use POCUS include emergency medicine, critical care, internal medicine, anesthesia, obstetrics and gynecology, surgery, cardiology, and primary care. POCUS is also increasingly integrated into pre-hospital and point-of-injury care by paramedics and emergency medical technicians.