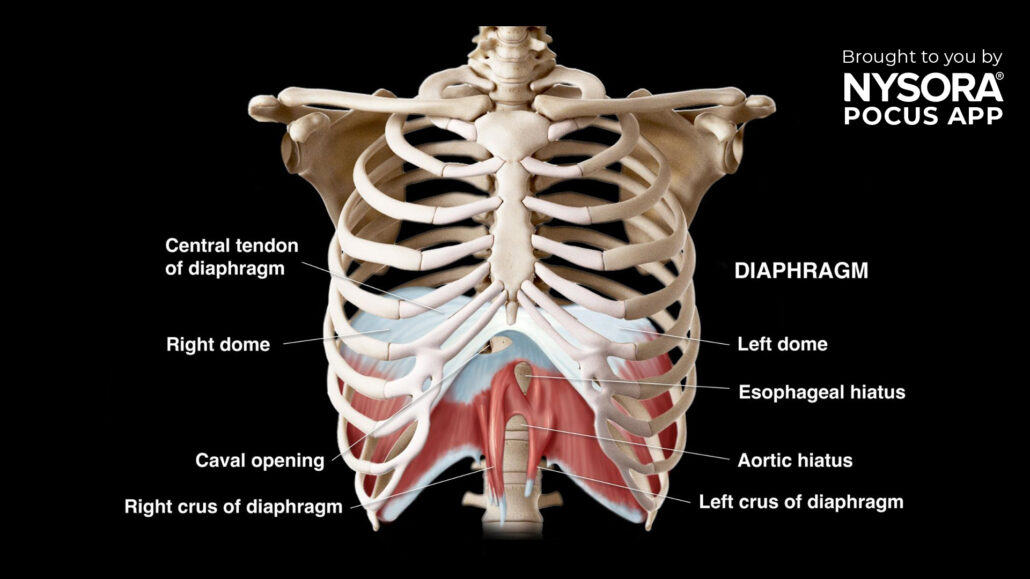
Case study: Assessing diaphragmatic function using ultrasound
Diaphragm ultrasound is a non-invasive, point-of-care ultrasound (POCUS) technique used to assess diaphragmatic function. This case study explores its application in evaluating diaphragmatic dysfunction in a clinical setting.
Case presentation
A 60-year-old woman was transferred to the ICU following an elective cardiac surgery. Her medical history included chronic obstructive pulmonary disease (COPD) and hypertension. Postoperative complications included prolonged ventilator dependency and difficulty weaning from mechanical ventilation.
Physical examination
The patient was alert but exhibited signs of respiratory distress, including shallow breathing and accessory muscle use. Auscultation revealed reduced breath sounds at the lung bases. There was no evidence of overt neuromuscular weakness, but diaphragmatic dysfunction was suspected.
Clinical decision
Given the suspicion of diaphragmatic dysfunction contributing to the patient’s difficulty in weaning from mechanical ventilation, a diaphragm ultrasound was performed at the bedside to assess the diaphragm’s structure and function.
Indications for diaphragm ultrasound
- Difficulty in weaning from mechanical ventilation
- Suspected diaphragmatic paralysis or dysfunction
- Postoperative assessment following high-risk surgeries
- Evaluation of neuromuscular disorders affecting respiratory function
Essential information on diaphragm ultrasound
- Diaphragm ultrasound provides real-time, dynamic assessment of diaphragm movement and thickness.
- It is a bedside, non-invasive technique that offers immediate insights into diaphragmatic function.
- While it complements other imaging modalities, diaphragm ultrasound is particularly useful for trending diaphragm function over time.
Ultrasound machine setup
- Transducer: Curvilinear or phased array SCA; linear for ZOA.
- Preset: Abdominal
- Orientation: Transverse for SCA and toward the head for ZOA.
- Depth: 12-18 cm for SCA; 1.5-3 cm for ZOA
Patient Positioning
- Position the patient supine with both arms at their sides.
- For better access to the diaphragm, slight lateral decubitus or slight upright positioning may be utilized, though reproducibility may be lower.
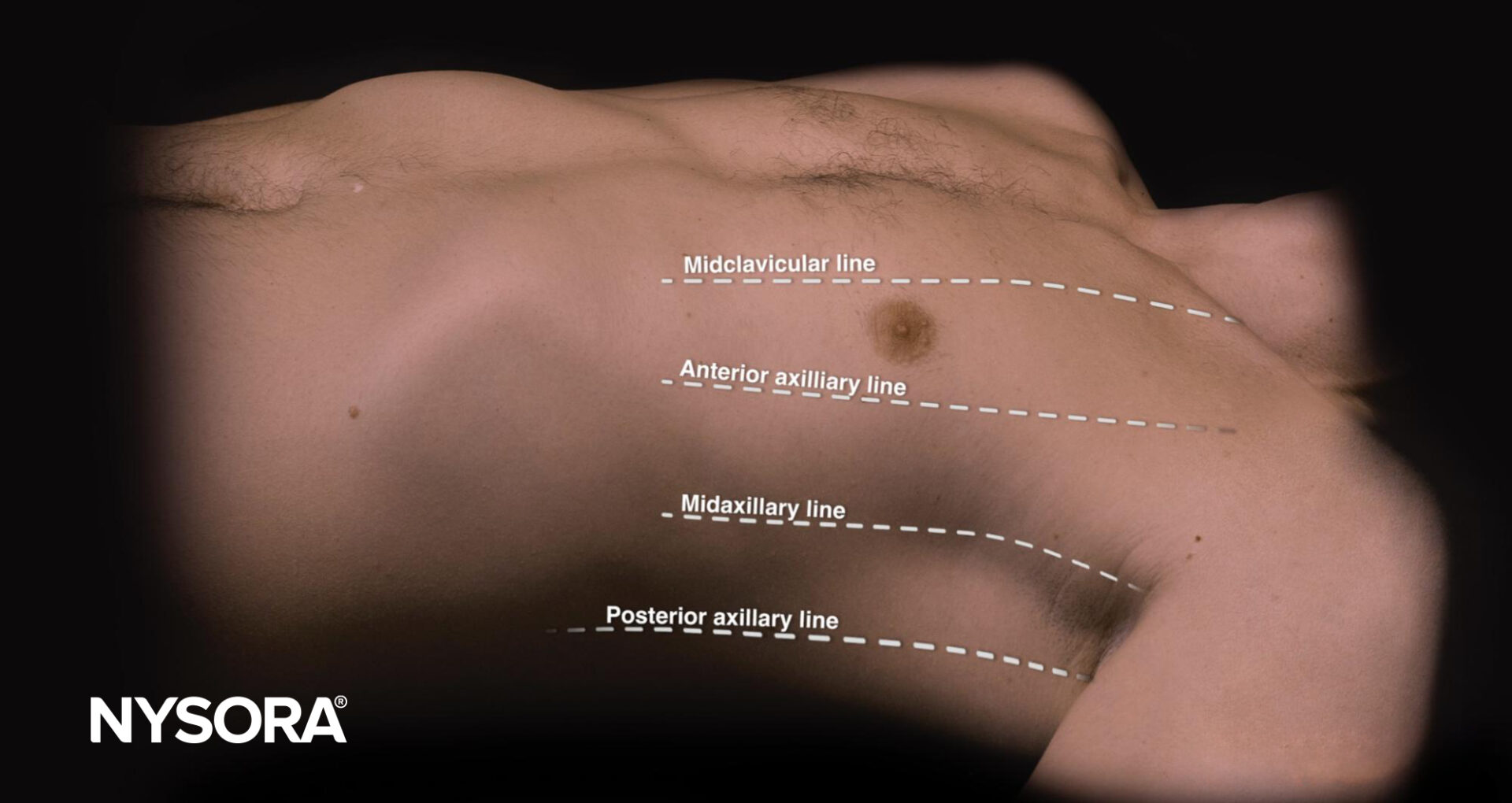
Landmarks
- Clavicle: Midclavicular line
- Axilla: Anterior axillary line
- Costal Margin: Identify for transducer placement
- Xiphoid Process: As a reference point for subcostal imaging
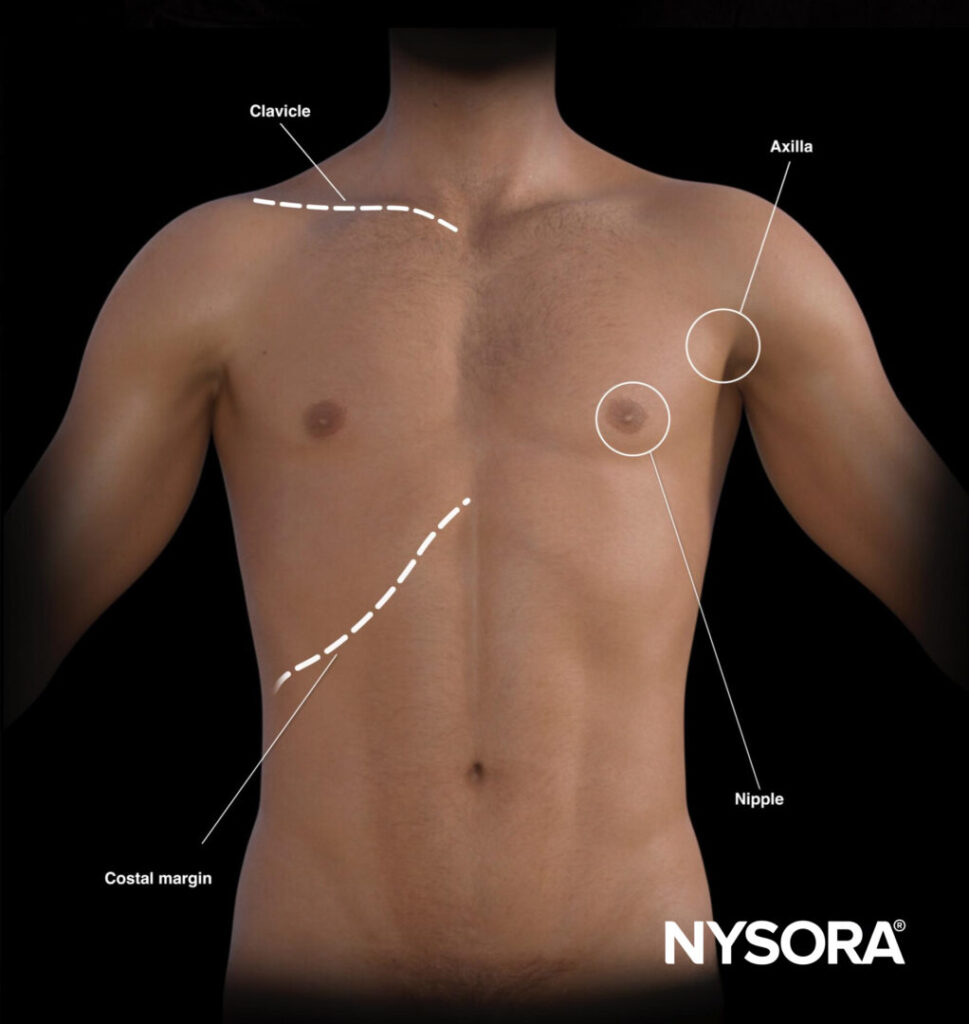
The landmarks on the thorax can also help with virtual lines for transducer placement.
Views
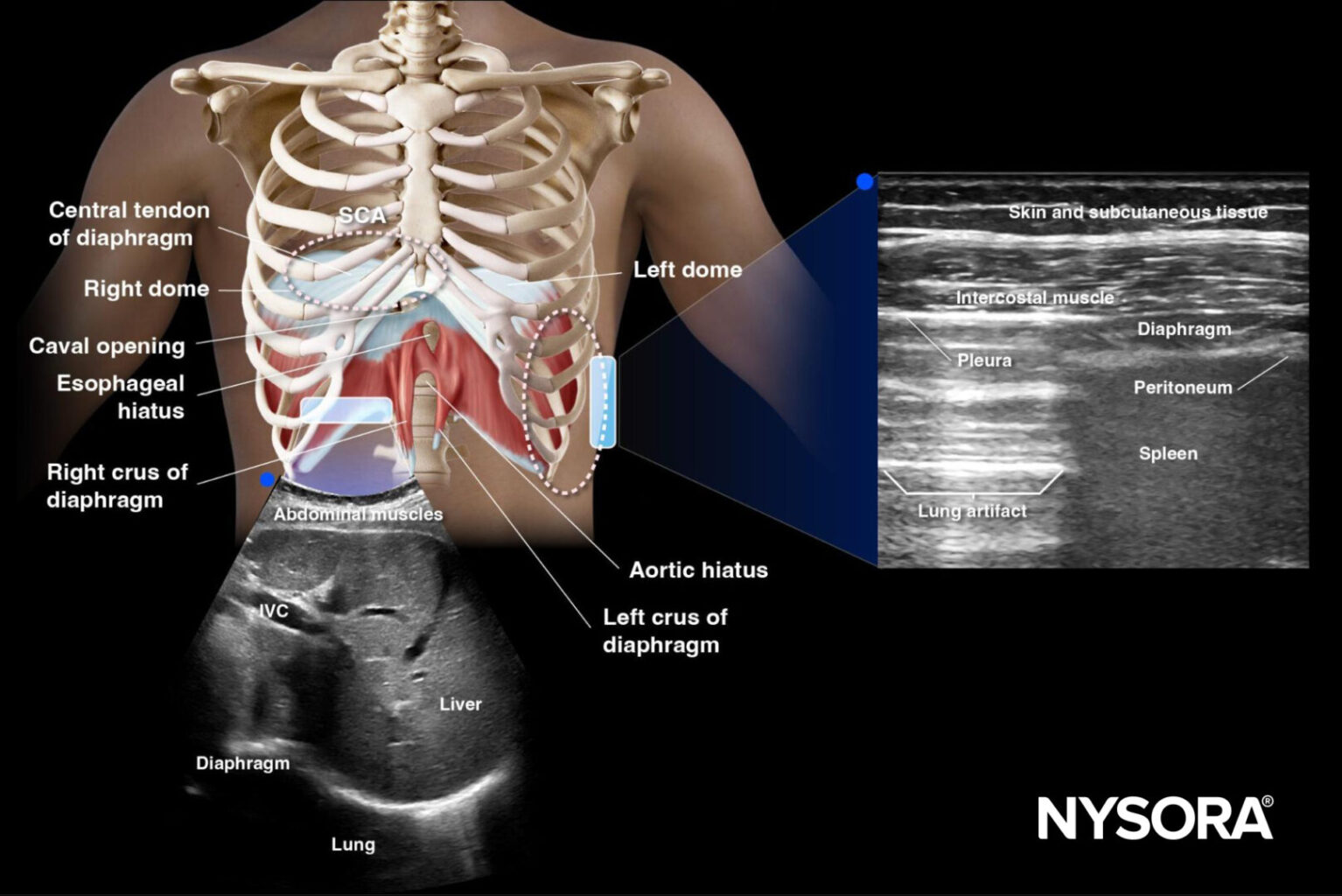
- Subcostal Area (SCA):
- Place the transducer in a transverse position in the subcostal region on the midclavicular line.
- Visualize the diaphragm using the liver or spleen as acoustic windows.
- Zone of Apposition (ZOA):
-
- Place the transducer parallel to the ribs between the 8th and 10th intercostal spaces along the anterior axillary line.
- Evaluate the diaphragm as a three-layered structure beneath the pleural line.
Assessment
Diaphragmatic Excursion
Normal excursion: Diaphragm movement should appear as a sinusoidal pattern on M-mode during respiration.
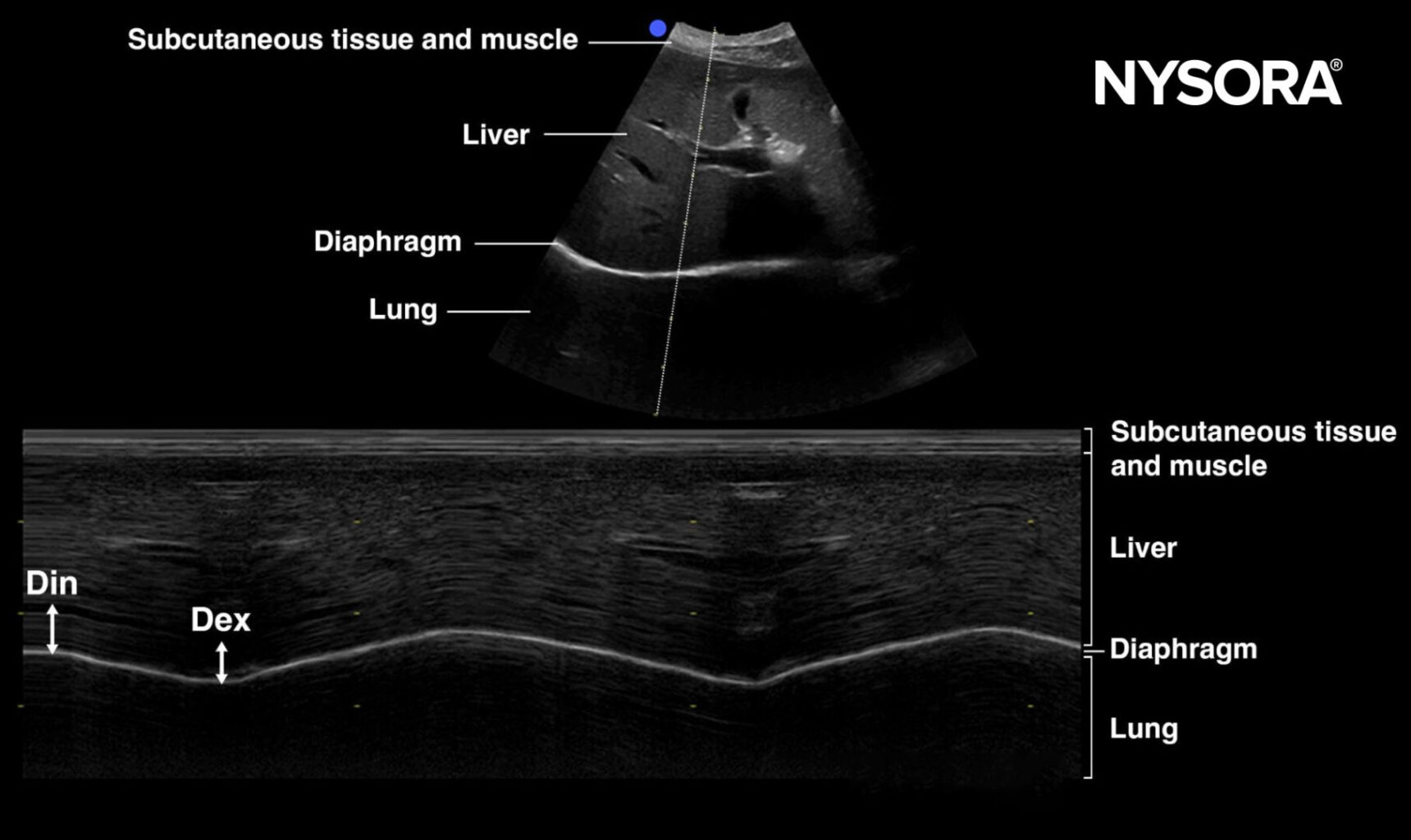
- Measurement: Excursion is measured in centimeters. Normal values for diaphragm excursion during shallow breathing, deep breathing, and sniffing maneuvers are:
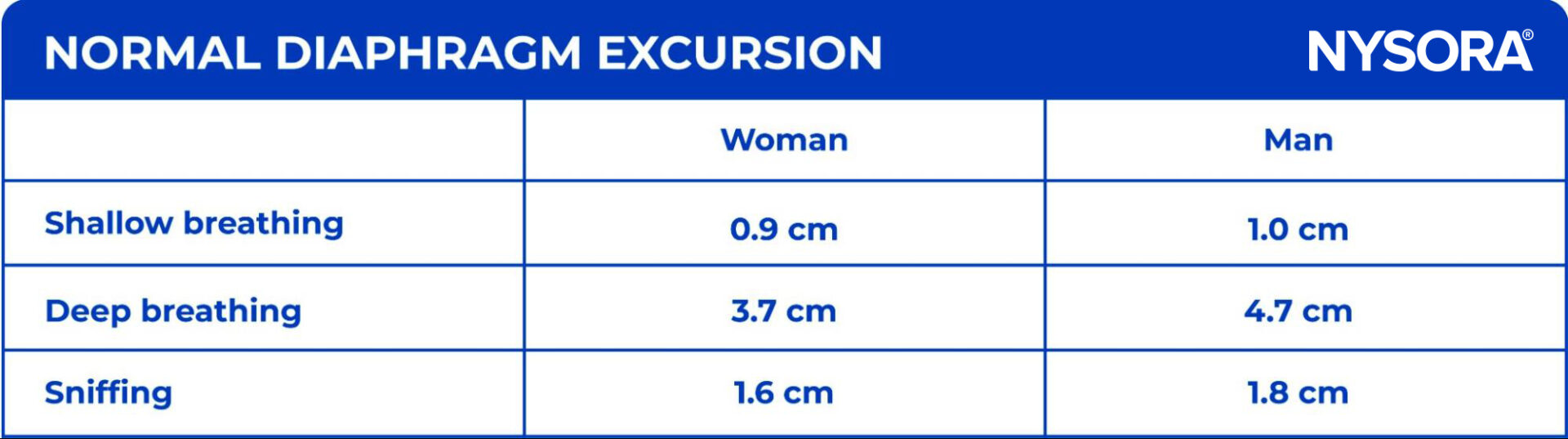
- Findings: In this patient, diaphragm excursion during shallow breathing was 0.5 cm, indicating diaphragmatic dysfunction. A paradoxical cranial movement of the diaphragm during inspiration was observed, suggestive of diaphragm paralysis.
Diaphragm Thickening
Normal Thickening: The diaphragm should thicken during inspiration, with the thickness increasing from around 1.7 mm during shallow breathing to 4.5 mm at total lung capacity (TLC).
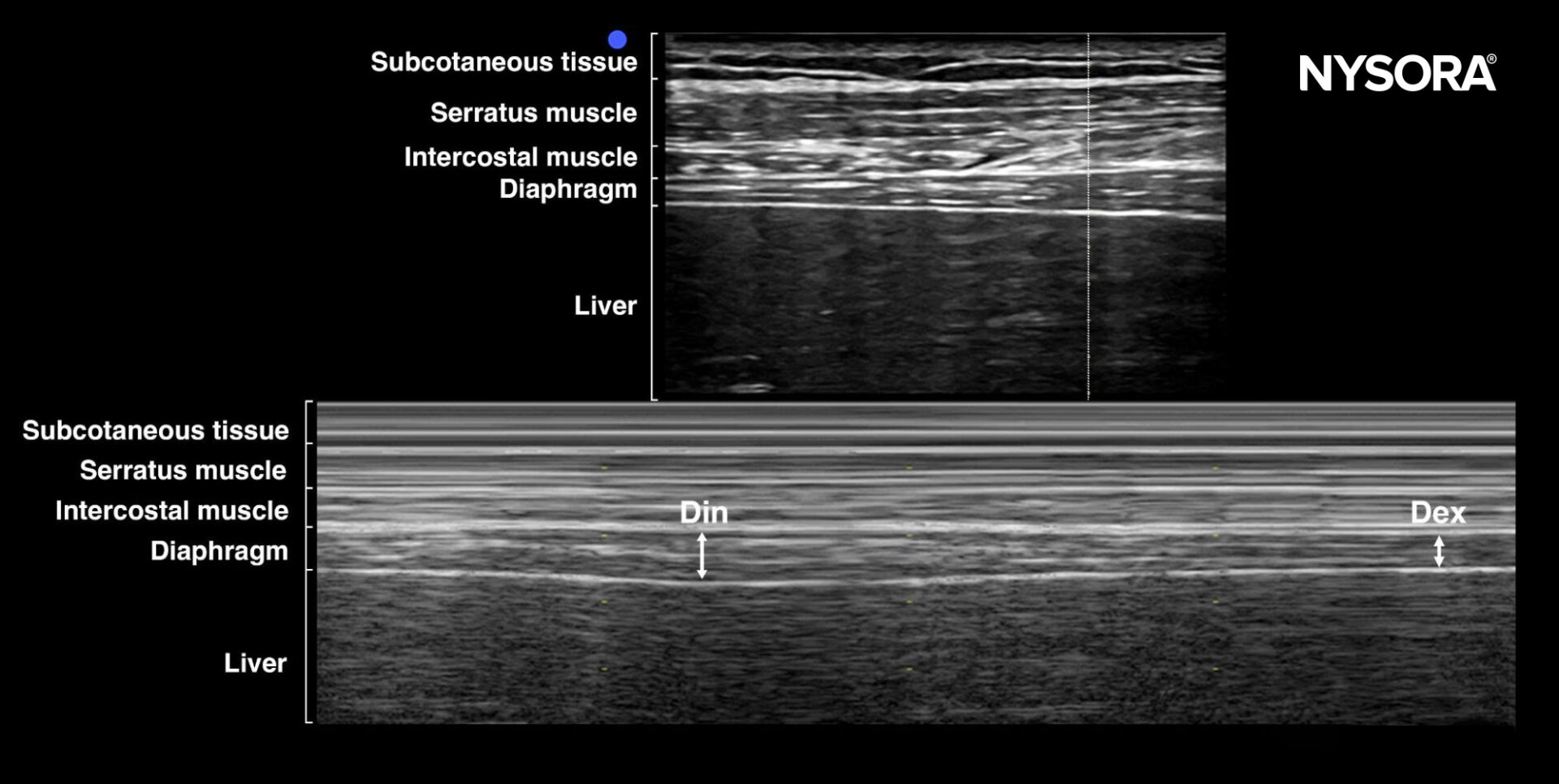
- Thickening Fraction (TF): Calculated using the formula:
TF = (Din-Dex)/Dex
A TF of less than 20% indicates diaphragmatic dysfunction. In this patient, TF was calculated to be 15%, confirming the diagnosis of diaphragmatic dysfunction.
Diagnosis
The findings strongly suggest that the patient is suffering from diaphragmatic dysfunction, likely related to diaphragm paralysis. This condition is contributing to the difficulty in weaning the patient from mechanical ventilation. Immediate interventions to address this dysfunction should be considered, including possible supportive therapies or further investigation to determine the underlying cause of the paralysis.
For more in-depth information on diaphragm ultrasound and advanced applications, consider downloading NYSORA’s POCUS App for detailed resources, illustrations, animations, and more.