Case study: Bimalleolar fracture completed under a popliteal sciatic nerve block
Case presentation
A 70-year-old patient with a history of renal insufficiency presented at our facility with a bimalleolar fracture. The patient was scheduled for the removal of an external fixator, followed by open reduction and internal fixation (ORIF) in the prone position. Importantly, the patient expressed a preference to avoid general anesthesia.
Anesthesia plan
Given the patient’s preference and medical history, the anesthesia team opted for a combination of spinal anesthesia and a peripheral nerve block. Initially, spinal anesthesia was administered using 10 mg (2 mL) of isobaric bupivacaine 0.5%. Subsequently, once the patient was positioned prone in the operating room, a popliteal block was performed using 15 mL of ropivacaine 0.5%. This approach was chosen to provide both intraoperative anesthesia and postoperative pain relief. A tourniquet was placed above the knee to facilitate the surgical procedure.
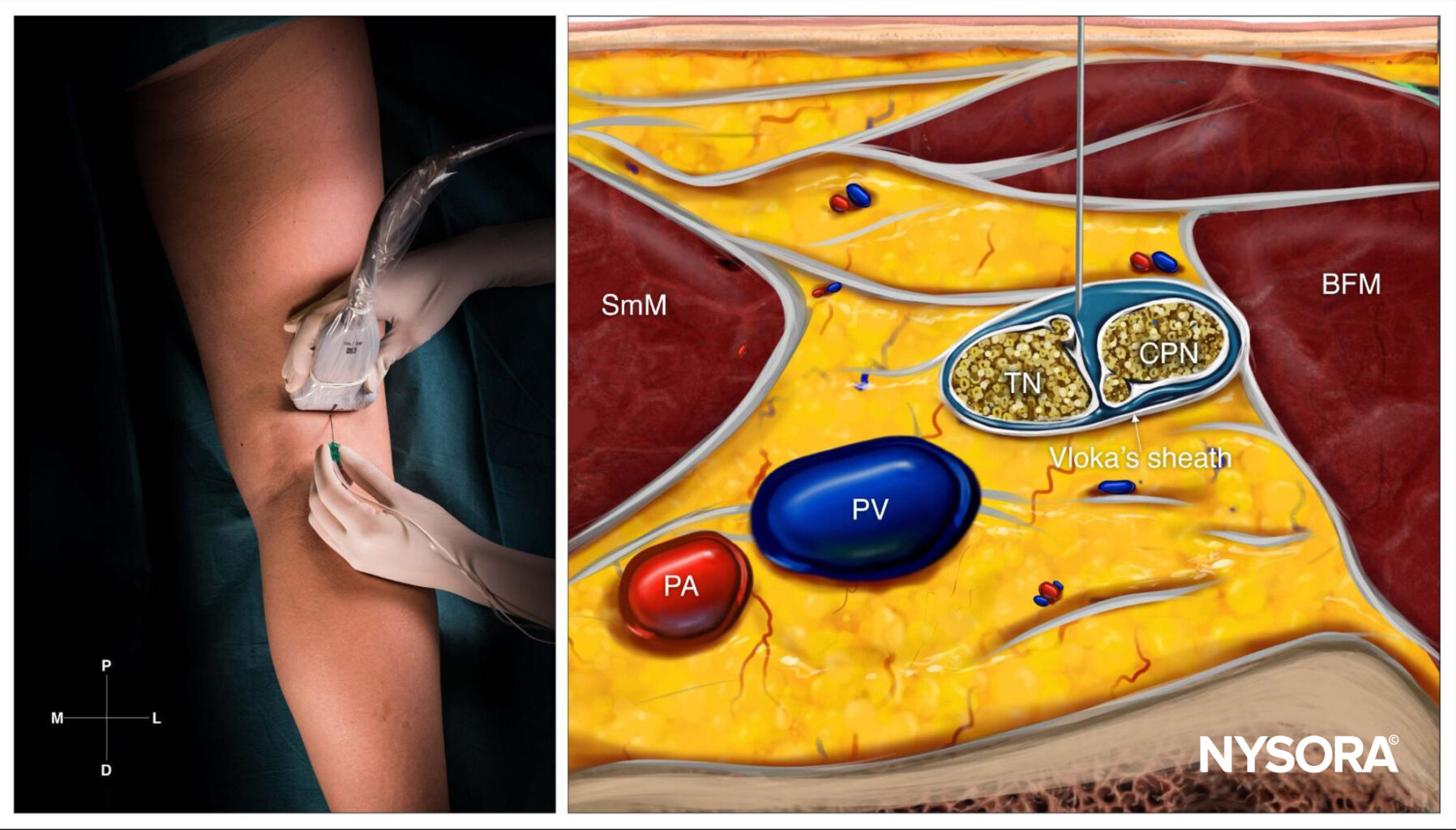
Reverse Ultrasound Anatomy for a popliteal block with needle insertion out-of-plane. The local anesthetic spread is shown in blue. TN, tibial nerve; CPN, common peroneal nerve; PA, popliteal artery; PV; popliteal vein; SmM, semimembranosus muscle; BFM, biceps femoris muscle.
Patient outcome
The combination of spinal anesthesia and popliteal block was successful in providing adequate anesthesia for the duration of the surgery. The patient reported minimal discomfort and remained hemodynamically stable throughout the procedure. Postoperatively, the patient experienced effective pain relief from the popliteal block.
This case highlights the effectiveness of combining spinal anesthesia with a peripheral nerve block in patients where general anesthesia is either contraindicated or not preferred. It also demonstrates the importance of individualizing anesthesia plans to cater to patient preferences and specific health conditions.
Advancing pain management in ankle fracture surgery: Insights from the AnAnkle trial
Effective pain management is a cornerstone of successful surgical outcomes, especially in orthopedic procedures like ankle fracture surgery. The AnAnkle Trial, a groundbreaking randomized clinical study, offers valuable insights into the efficacy of peripheral nerve blocks (PNBs) compared to spinal anesthesia (SA). Conducted across two centers with 150 participants, this trial provides a detailed comparison of postoperative pain profiles, opioid consumption, and patient satisfaction.
Key findings
- Superior pain control with PNBs:
-
-
- Patients who received PNBs reported significantly lower pain intensity scores and morphine consumption within the first 27 hours post-surgery compared to those who underwent SA.
- PNBs demonstrated an extended analgesic effect, lasting an average of approximately 16.5 hours compared to just 3.5 hours with SA.
-
- Reduced opioid dependency:
-
-
- PNB recipients consumed less intravenous morphine (median of 20 mg) compared to SA patients (median of 32.5 mg) within the initial 27 hours.
- Despite the potential for rebound pain after PNB resolution, overall opioid-related side effects were fewer in the PNB group.
-
- High Patient Satisfaction:
-
- An overwhelming 99% of patients in the PNB group stated they would choose the same anesthesia method again, compared to 90% in the SA group.
Anesthesia techniques evaluated
Peripheral nerve blocks (PNBs)
- Administered as ultrasound-guided popliteal sciatic and saphenous blocks using ropivacaine.
- Advantages:
- Precise targeting of nerve clusters for localized and effective pain relief.
- Extended duration of pain control compared to SA.
- Challenges:
- Rebound pain following the resolution of the block remains a concern but is manageable with appropriate follow-up care.
Spinal anesthesia (SA)
- Utilized hyperbaric bupivacaine for neuraxial nerve blocking.
- Advantages:
- Immediate onset of anesthesia.
- Limitations:
- Shorter duration of analgesia.
- Increased likelihood of requiring supplemental opioids for pain management.
Impact on postoperative recovery
Pain intensity and opioid consumption (PIOC) scores
The primary endpoint of the study combined longitudinal pain scores with opioid usage, providing a comprehensive measure of postoperative recovery:
- PNB patients exhibited significantly better PIOC scores, with a median reduction of 26.5%, compared to an increase of 54.3% in the SA group.
- The probability of a better PIOC score with PNB over SA was estimated at 74.8%.
Quality of recovery
Although the overall quality of recovery scores (QoR-15) did not differ significantly between the groups, the longer-lasting pain relief and lower opioid requirements associated with PNBs indicate an enhanced recovery experience.
Clinical implications
- Optimizing pain management strategies:
-
-
- The trial underscores the potential of PNBs to reduce reliance on opioids, aligning with global efforts to mitigate the opioid crisis.
- Effective multimodal pain management protocols, including PNBs, should be standard in acute orthopedic surgeries.
-
- Addressing rebound pain:
-
-
- Strategies to mitigate rebound pain, such as transitioning to oral analgesics or multimodal approaches as the block resolves, are essential.
-
- Patient-centered care:
-
- The high patient satisfaction rate with PNBs highlights their role in enhancing surgical experience and recovery.
Conclusion
The AnAnkle Trial confirms that PNBs offer superior pain relief and reduced opioid consumption compared to SA in ankle fracture surgery. By providing prolonged analgesia and minimizing opioid-related complications, PNBs represent a significant advancement in regional anesthesia for orthopedic procedures.
For more information, refer to the full article in the British Journal of Anaesthesia.
Sort R, Brorson S, Gögenur I, Hald LL, Nielsen JK, Salling N, Hougaard S, Foss NB, Tengberg PT, Klausen TW, Møller AM. Peripheral nerve block anaesthesia and postoperative pain in acute ankle fracture surgery: the AnAnkle randomised trial. Br J Anaesth. 2021 Apr;126(4):881-888. doi: 10.1016/j.bja.2020.12.037.
For more case studies like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!