Deep venous thrombosis (DVT) is a serious medical condition in which a blood clot forms in the deep veins, typically in the legs. If left untreated, DVT can lead to life-threatening complications like pulmonary embolism (PE). This article presents a case study of a 52-year-old patient with DVT following recent orthopedic surgery. It outlines the steps for diagnosing and managing this condition using point-of-care ultrasound (POCUS) and clinical guidelines.
A 52-year-old man presented to the emergency department with swelling and pain in his left leg, worsening over the last three days.
Medical History:
- Recent knee replacement surgery (2 weeks ago)
- Obesity (BMI 33)
- Smoking habit (1 pack/day for 20 years)
Clinical examination findings:
- Localized pain and asymmetric edema in the left leg.
- Reddish-blue skin discoloration over the calf.
- Mild dyspnea (shortness of breath) and discomfort in the chest, raising concerns about potential pulmonary embolism.
Common risk factors for DVT:
- Recent surgery, especially orthopedic procedures
- Prolonged immobilization
- Cardiac conditions
- Hypercoagulable states (blood clotting disorders)
- Smoking, obesity, and use of contraceptive medications
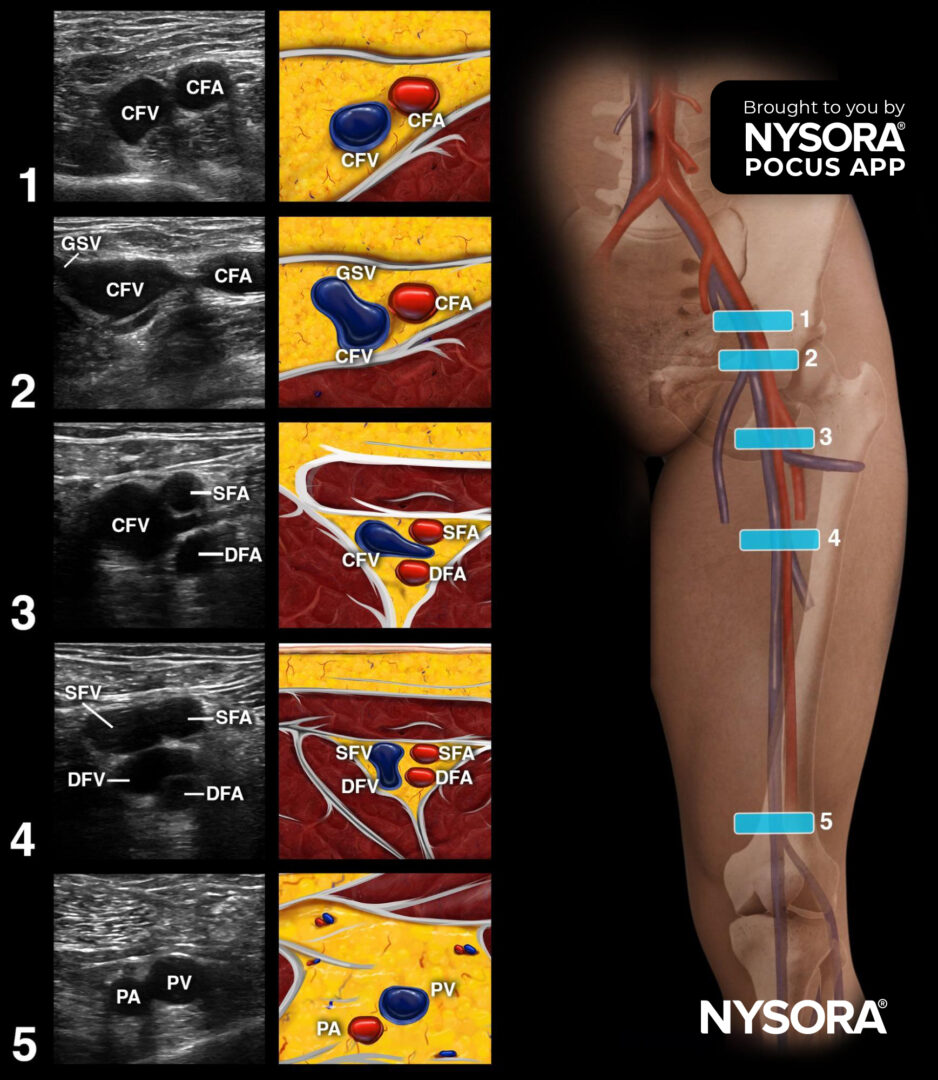
Diagnostic approach: Using POCUS to detect DVT
- Position the patient:
- Start with the patient supine with the leg extended and externally rotated.
-
- For popliteal (behind the knee) assessments, position the leg in flexion.
2. Scanning:
-
- Start at the inguinal crease with a linear transducer.
- Scan slowly and assess the compressibility of the vein every 1-2 cm along the femoral and popliteal areas.
3. Key locations for detecting thrombi:
-
- Common femoral vein (CFV)
- Bifurcation of the CFV and saphenous vein
- Popliteal vein
Pay special attention to these regions as they are common sites for clot formation.
4. Confirm DVT:
-
- The vein’s non-compressibility is a definitive sign of DVT. In normal cases, applying pressure to the vein with the transducer should collapse it completely. If it remains open, a thrombus is likely present.
Ultrasound findings
n this case, the ultrasound revealed a non-compressible femoral vein at the bifurcation of the lateral perforator vein, confirming a deep venous thrombosis. The thrombus only partially obstructed the vein, which is also common in DVT cases.
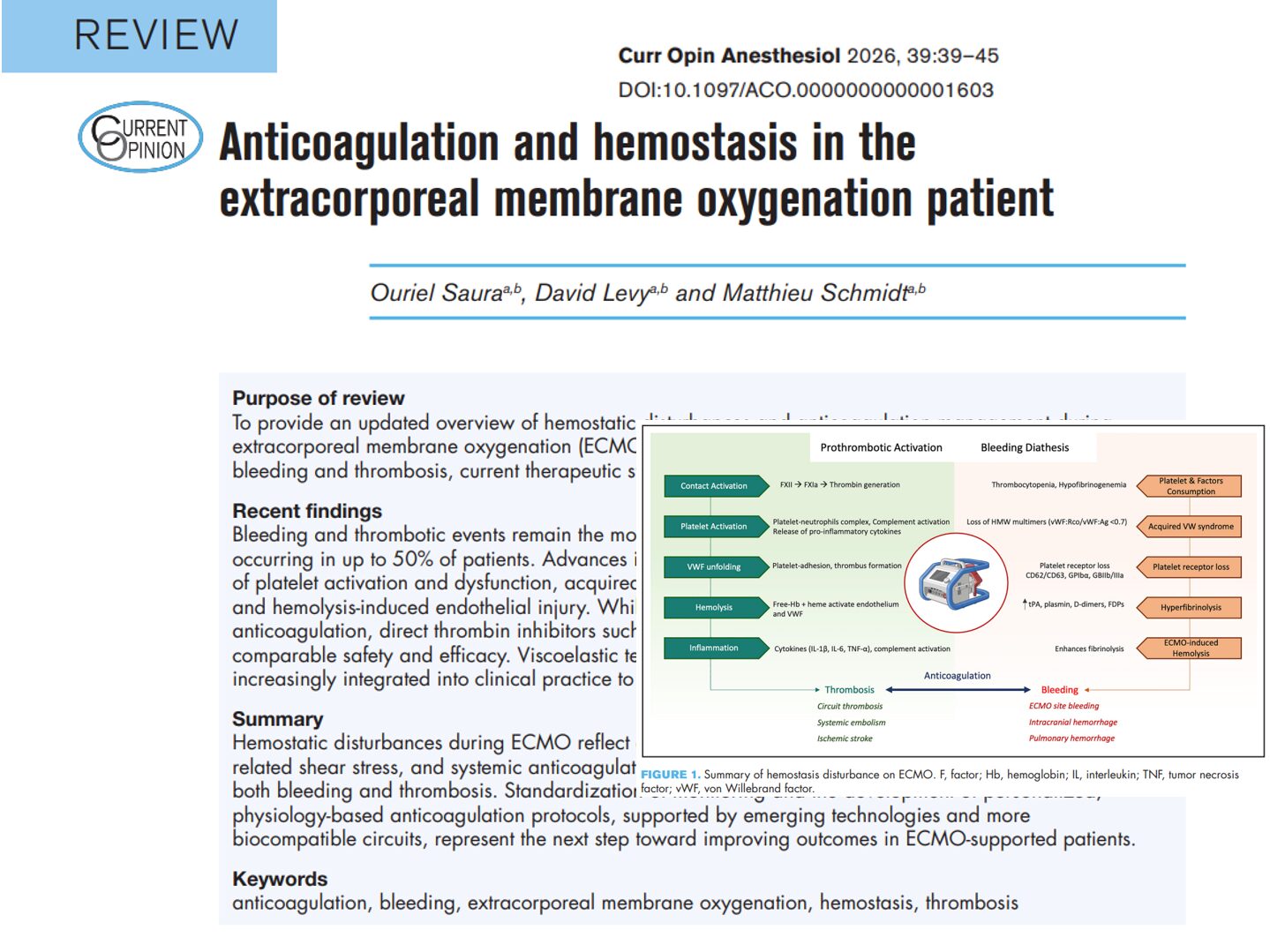
Management
Upon diagnosing DVT, immediate anticoagulation was initiated with intravenous heparin, followed by a transition to long-term oral anticoagulation such as warfarin or a DOAC. The patient was monitored for pulmonary embolism through testing like CT pulmonary angiography due to shortness of breath and chest discomfort. Graduated compression stockings were prescribed to improve venous flow and prevent complications. At the same time, lifestyle modifications, including quitting smoking, maintaining a healthy weight, and regular physical activity, were recommended to reduce future DVT risk.
Conclusion
Deep venous thrombosis is a serious condition that can have life-threatening consequences if not diagnosed and treated early. In this case, early detection through ultrasound and timely intervention with anticoagulant therapy helped prevent the progression of the clot and potential pulmonary embolism. Recognizing the symptoms, understanding the risk factors, and following best practices for DVT management can significantly improve patient outcomes and reduce the likelihood of future complications.
For more information on detecting DVT using point-of-care ultrasound, download NYSORA’s POCUS App!