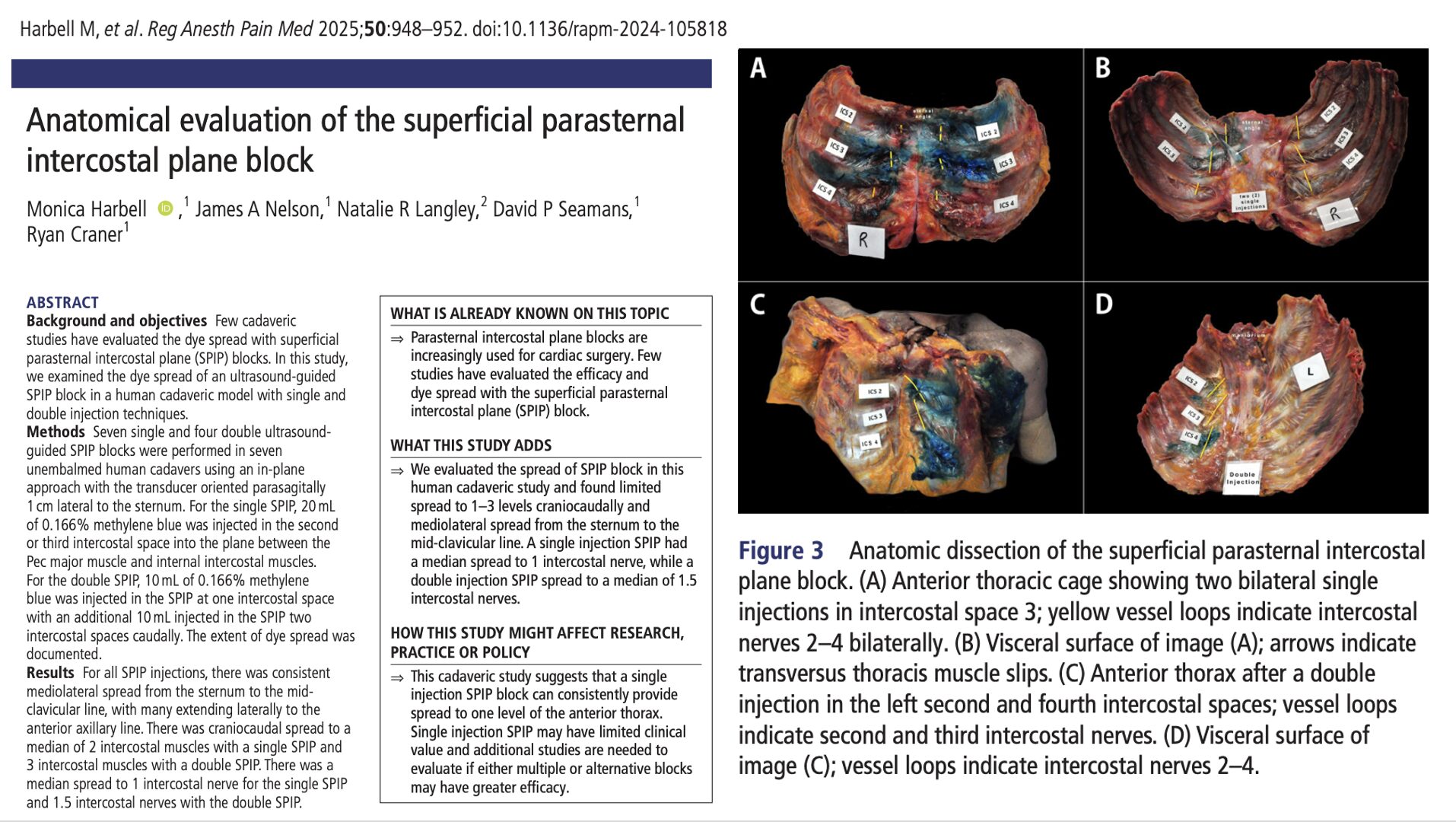
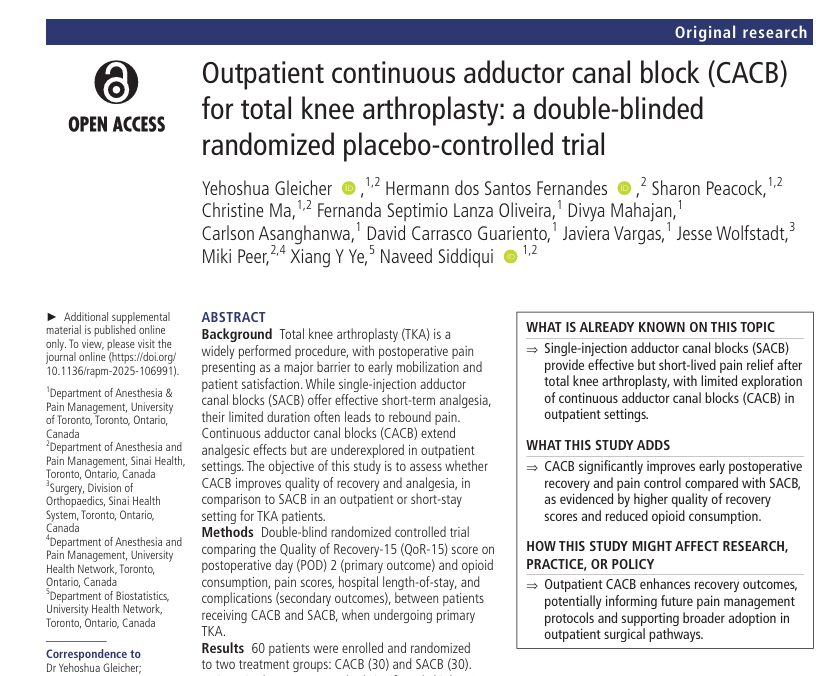
Total knee arthroplasty (TKA) is a common procedure for treating end-stage osteoarthritis, with significant postoperative pain as a notable complication. The adductor canal block (ACB) has become a standard analgesic technique for managing postoperative pain, offering effective pain relief without the quadriceps weakness typically associated with femoral nerve blocks. Recent advancements include continuous ACBs, which extend analgesic effects beyond single injections. However, catheter migration remains a challenge, leading to inadequate analgesia.
A novel approach, the interfascial plane between the sartorius muscle and femoral artery (ISAFE) technique, promises to reduce catheter migration. This study compares the ISAFE approach with the traditional adductor canal catheter insertion technique, hypothesizing that ISAFE will result in lower catheter dislodgment rates.
Study objective and methods
The primary objective of this randomized controlled trial was to compare the incidence of adductor canal catheter dislodgment between the ISAFE approach and the conventional catheter insertion technique in patients undergoing unilateral TKA.
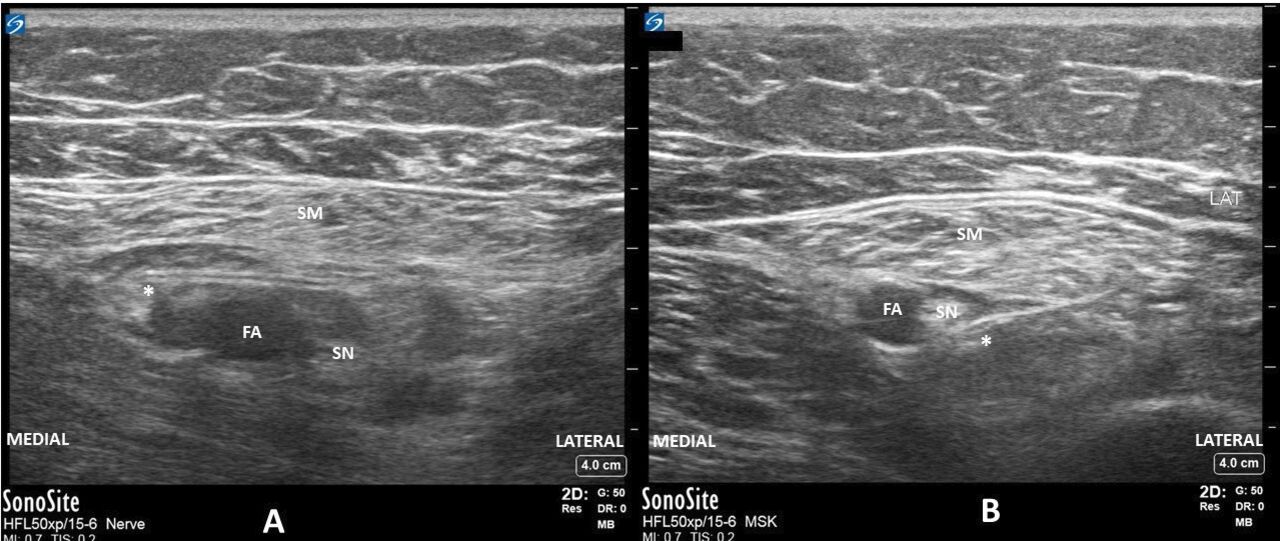
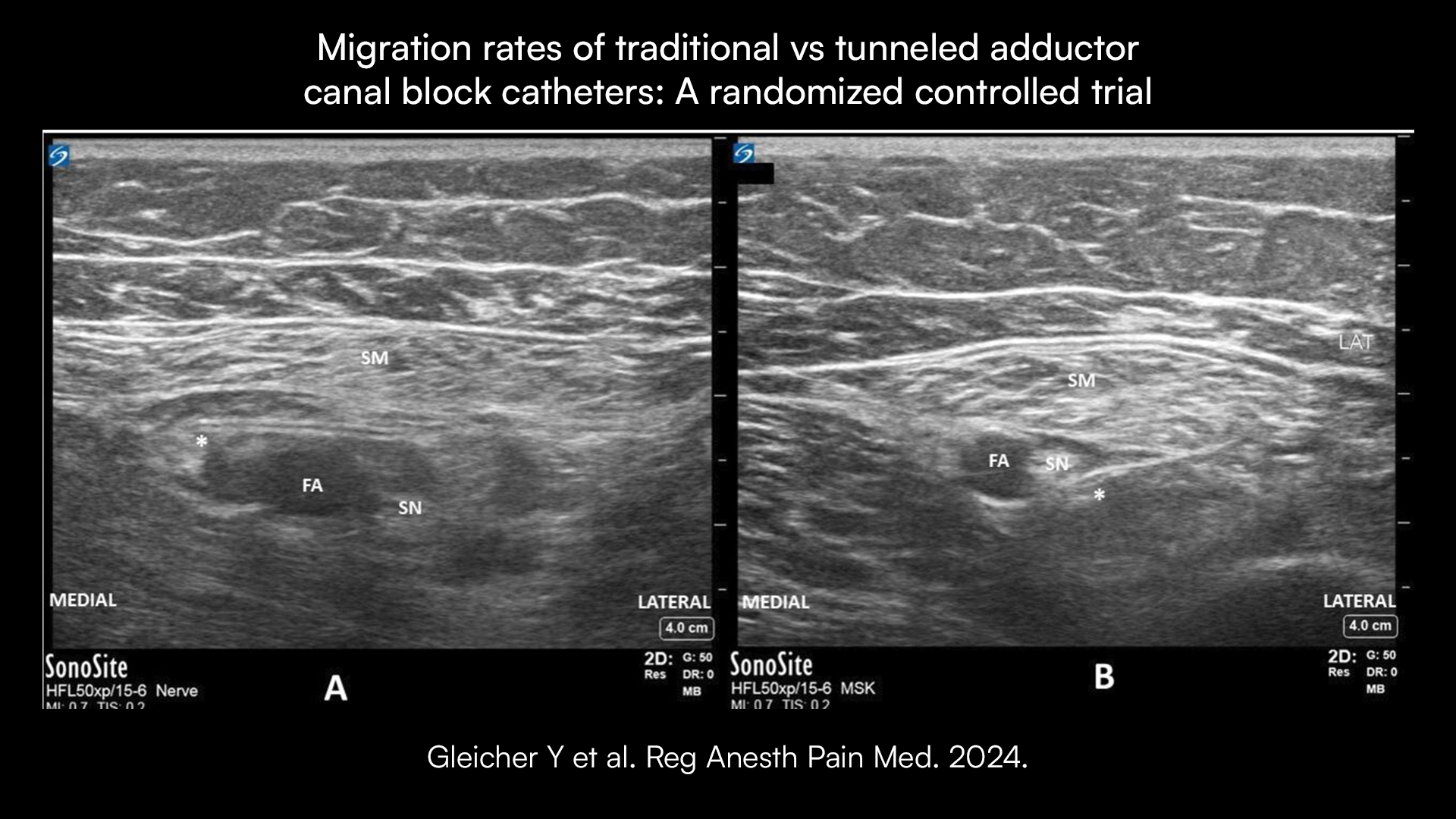
(A) ISAFE approach. (B) Conventional approach. *Catheter tip final position. FA, femoral artery; ISAFE, interfascial plane between the sartorius muscle and femoral artery; SM, sartorius muscle; SN, saphenous nerve.
The study aimed to determine whether the ISAFE approach would result in a lower dislodgment rate, thereby improving postoperative analgesia. Ninety-seven patients were randomized into two groups: the ISAFE group and the conventional group. Blinding was maintained for both patients and evaluators. Catheters were inserted postoperatively under ultrasound guidance, with their positions confirmed and secured. The primary outcome was assessed via ultrasound 24 hours after surgery, while secondary outcomes, including pain scores, opioid consumption, and catheter-related complications, were monitored for 48 hours post-surgery.
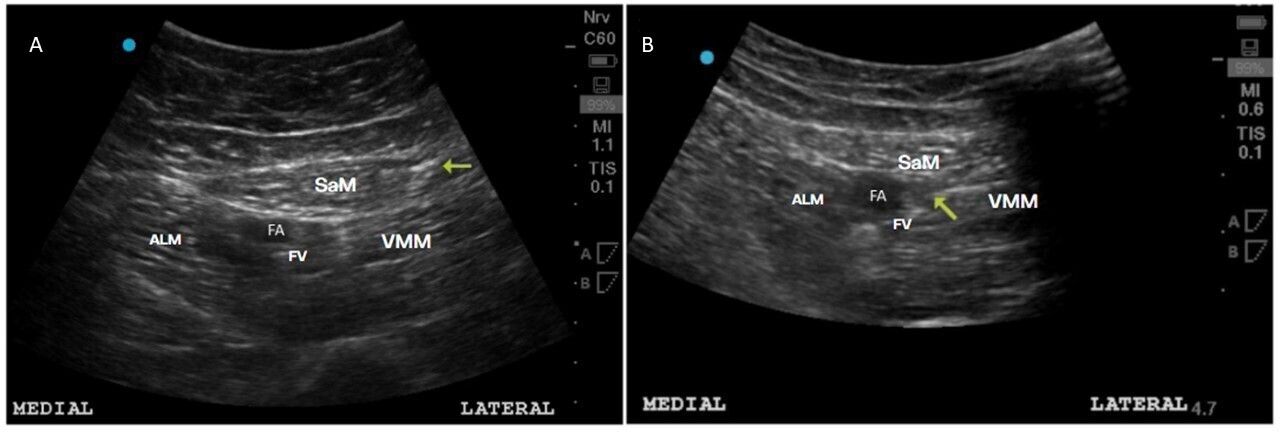
(A) Tip of a migrated peripheral nerve catheter inside sartorius muscle (yellow arrow). (B) Tip of a peripheral nerve catheter remaining inside adductor canal (yellow arrow). In both cases, a saline injection was used to locate the catheter tip. ALM, adductor longus muscle; FA, femoral artery; FV, femoral vein; SaM, sartorius muscle; VMM, vastus medialis muscle.
Results
Primary outcome
The ISAFE group had significantly lower catheter dislodgment compared to the control group (18.6% vs 44.9%, p=0.01).
Secondary outcomes
- Pain scores at rest were lower in the ISAFE group on POD 1 and POD 2.
- No significant differences in pain scores during movement or opioid consumption between the groups.
- The distance from the initial catheter position was similar in both groups, but ISAFE catheters were closer to the saphenous nerve.
Catheter-related complications
- No significant differences in insertion-related complications between groups.
- No catheter displacement at the skin insertion site was noted in either group.
Discussion
The ISAFE technique significantly reduces catheter migration compared to the traditional approach. Although both techniques showed similar migration distances, ISAFE catheters remained closer to the saphenous nerve, enhancing analgesic efficacy. The findings suggest that tunneling the catheter across the adductor canal or parallel to the saphenous nerve prevents dislodgment. Despite lower pain scores at rest in the ISAFE group, the clinical relevance remains uncertain due to similar opioid usage between groups.
Conclusion
The ISAFE approach for continuous ACB catheter placement reduces migration rates compared to the conventional technique. Further research is needed to determine if these differences translate into improved clinical outcomes.
For more detailed information, refer to the full article in RAPM.
Gleicher Y, Dos Santos Fernandes H, Peacock S, et al. Comparison of migration rates between traditional and tunneled adductor canal block catheters: a randomized controlled trial. Reg Anesth Pain Med. 2024;49(6):423-428.
Gleicher Y et al. Reg Anesth Pain Med. 2024.
Unlock comprehensive insights into the adductor canal block by downloading the Nerve Blocks App HERE, and you can find it in the book format on Amazon.