Explore NYSORA knowledge base for free:

Upper respiratory tract infections (URTI) are common in children and pose significant challenges during perioperative management. A recent focused review by Stepanovic et al. 2024 outlines the latest evidence and strategies to ensure safe anesthesia practices for children with URTI, including those recovering from COVID-19. Understanding the risks Increased adverse events: Children with current or recent URTI have a 2-3 times higher risk of respiratory complications like laryngospasm, bronchospasm, and desaturation during surgery. These complications can lead to prolonged oxygen therapy, unintended ICU admissions, or even premature termination of surgeries. Patient-specific risks: Children under 2 years of age or with conditions like asthma, sleep apnea, or respiratory tract infections within the last two weeks are particularly vulnerable. Fever, wheezing, moist cough, and lethargy signal severe URTI and necessitate surgery postponement. Key factors to consider Timing of surgery: Elective surgeries should ideally be deferred for at least two weeks after URTI symptoms resolve. Severe cases, such as high fever or green nasal discharge, may require up to four weeks for airway recovery. Choice of airway device: Supraglottic airway devices are associated with lower risks compared to tracheal tubes. Tracheal tubes are often reserved for situations requiring more secure airways due to their higher complication rate in children with URTI. Anesthesia techniques: Total intravenous anesthesia (TIVA) using propofol is recommended due to its bronchodilatory effects and reduced risk of airway hyperreactivity. Avoid desflurane as it is linked to increased airway reactivity. Risk mitigation strategies: Preoperative administration of salbutamol or alpha-2 agonists like dexmedetomidine can reduce bronchospasm. Deep extubation techniques may reduce airway stimulation and associated complications but require experienced staff for safe implementation. Decision-making framework Risk stratification: Tools like the COLDs score help standardize the risk profile for children with URTI. Scores over 10 suggest higher risks, necessitating careful planning and possibly delaying […]

The medical field evolves rapidly, and regional anesthesia is no exception. Keeping up with the latest techniques and evidence-based practices is crucial for anesthesiologists striving for excellence in patient care. Regional Anesthesia Updates 2025, by NYSORA, offers a streamlined, peer-reviewed resource tailored for busy clinicians. Here’s why this publication is your go-to for advancing your practice. Why choose Regional Anesthesia Updates 2025? Expertly summarized, clinically relevant content Regional Anesthesia Updates 2025 consolidates a year’s worth of groundbreaking research into concise summaries that you can digest in under 10 minutes. Each update is peer-reviewed by leading experts, ensuring the highest level of accuracy and clinical relevance. Stay ahead without the overwhelm Summaries of the most impactful research over the past 12 months. Actionable insights tailored for application in clinical settings. References for further exploration of original articles. Designed for busy professionals Tailored for anesthesiologists, this resource delivers concise, actionable updates to fit your demanding schedule. Whether you’re in the OR or taking a quick coffee break, it provides quick, reliable guidance to enhance your practice. Key features of Regional Anesthesia Updates 2025 Peer-reviewed for accuracy Every guideline and recommendation in this update undergoes rigorous evaluation by specialists. This ensures the content is not only current but also adheres to the highest standards of quality. Trustworthy, curated insights empower you to deliver more effective care. Eliminate the Fear of Missing Out (FOMO) The sheer volume of new research can feel overwhelming. This book offers a focused review of the most critical literature, so you stay informed without losing valuable time. Enhanced learning experience Original illustrations: Simplify complex concepts with NYSORA’s renowned visuals. Space for notes: Personalize your learning with dedicated sections for annotations and drawings. Crafted by RA experts Created specifically for anesthesiologists with a keen interest in regional anesthesia, the book […]
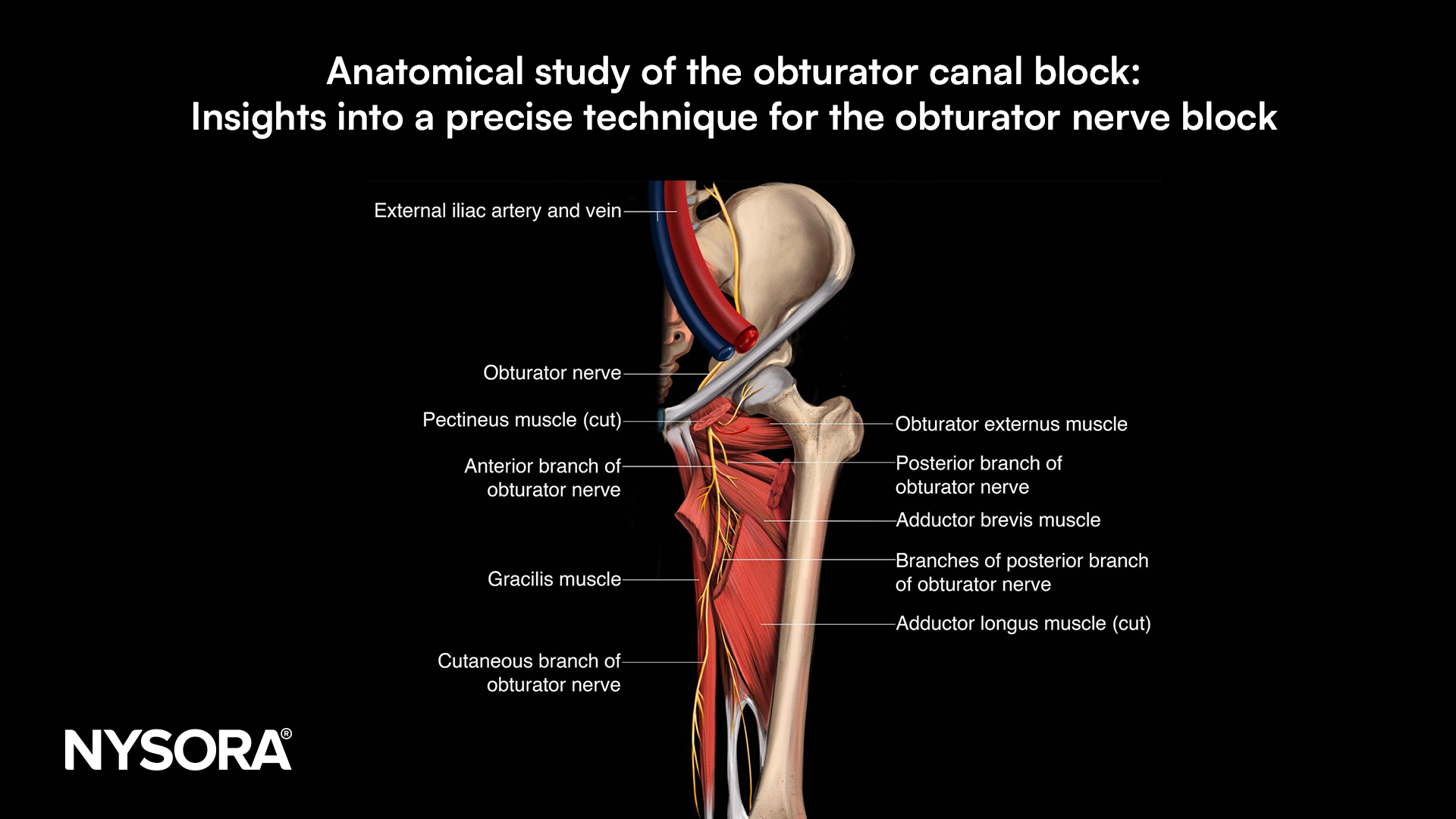
The obturator nerve (ON) plays a vital role in innervating the adductor muscles and contributing to the hip and knee joint innervation. Given its role in procedures requiring hip and knee anesthesia, the ON has become a target for nerve blocks. However, the obturator nerve’s anatomy and variations in its branching can complicate this block. Traditional methods for blocking the obturator nerve have shown varying levels of success due to these anatomical complexities. A recent anatomical study examined an ultrasound-guided approach targeting the obturator canal’s exit, aiming to clarify anatomical landmarks and solution distribution to enhance the accuracy and effectiveness of the obturator canal block (OCB). Study objective and methods This anatomical study sought to evaluate the distribution and effectiveness of an ultrasound-guided OCB at the exit of the obturator canal. The study used 10 cadavers to generate 20 hemipelvis samples. Ultrasound references helped identify key landmarks like the obturator canal, iliopubic ramus, pectineus, and external obturator muscles, as well as the obturator membrane. Injection technique: A low-frequency convex transducer initially identified the area, and a high-frequency linear transducer was then used to guide the injection of methylene blue dye at the exit of the obturator canal. Dissection and assessment: Dissections followed the injections to evaluate dye distribution within the obturator nerve’s branches, particularly the common trunk, anterior branch, and posterior branch. Key findings The study revealed consistent dye distribution across key branches of the obturator nerve, suggesting that the ultrasound-guided OCB technique provides precise coverage of the nerve and its branches. Dye distribution: The methylene blue dye stained the common trunk and anterior branch of the obturator nerve in all samples (100%) and the posterior branch in 80% of cases. This indicates that the ultrasound-guided technique achieved comprehensive coverage of the obturator nerve at the canal exit. Intrapelvic staining: […]