Axillary brachial plexus block vs. other regional anesthesia techniques
The most common indications for an axillary brachial plexus block include surgery of the forearm, wrist, or hand of moderate to long duration, with or without an arm tourniquet. It anesthetizes the brachial plexus at the level of the terminal branches (i.e., median, ulnar, radial, and musculocutaneous nerves), resulting in anesthesia of the upper extremity from the mid-arm down, including the hand.
Surgeries on the distal upper limb, such as wrist and hand operations, are increasingly performed in outpatient settings under regional anesthesia. General anesthesia (GA), while effective, carries risks such as postoperative nausea and prolonged recovery. Regional anesthesia techniques offer advantages, such as reduced recovery time, minimized opioid use, and enhanced patient satisfaction. Among these techniques, the axillary brachial plexus block (ABPB) is frequently used, especially for hands and wrist procedures, due to its relative ease of administration and favorable safety profile. Nijs et al. 2024 compare ABPB with other regional anesthesia (RA) techniques, including supraclavicular and infraclavicular blocks.
What is an axillary brachial plexus block?
ABPB is a method that involves injecting a local anesthetic into the axillary region, targeting the terminal branches of the brachial plexus. These branches provide sensory and motor innervation to the distal upper limb. This technique is especially suitable for forearm, wrist, and hand surgeries.
Other regional anesthesia techniques for upper limb surgery
In addition to ABPB, several other RA techniques are commonly used for distal upper limb surgeries:
- Supraclavicular block (SCB): Targets the trunks of the brachial plexus. This technique is effective for surgeries involving the entire arm, from the shoulder down.
- Infraclavicular block (ICB): Focuses on the cords of the brachial plexus and is commonly used for surgeries from the mid-arm to the hand.
- Intravenous regional anesthesia (IVRA or Bier block): Involves injecting anesthetic into a vein while using a tourniquet to limit the anesthetic’s distribution. This method is often used for minor, short-duration surgeries on the hand or forearm.
- Wide-awake local anesthesia no tourniquet (WALANT): A newer technique that involves directly injecting a local anesthetic into the surgical site without using a tourniquet.
Comparative efficacy of APBP and other techniques
1 Surgical anesthesia success
The primary outcome measure in comparing RA techniques is the ability to achieve adequate surgical anesthesia without the need for additional analgesia or conversion to GA. Studies show that ABPB is comparable to both supraclavicular and infraclavicular blocks. However, infraclavicular blocks demonstrate a slightly faster performance time and a marginally higher success rate in achieving complete anesthesia within 30 minutes.
- ABPB vs. supraclavicular block: There is no significant difference in the success rate of surgical anesthesia between these two techniques. Both approaches provide adequate anesthesia within 30 minutes of block placement.
- ABPB vs. infraclavicular block: Infraclavicular block has a statistically higher success rate and a faster performance time, making it preferable in busy surgical settings where time is critical.
2 Performance time and the onset of anesthesia
Performance time refers to the time required to administer the block. Studies indicate that infraclavicular blocks are performed significantly faster than ABPB, with a difference of about 5 minutes. This may be insignificant in settings where multiple procedures are performed sequentially, but it can be important to optimize operating room efficiency.
- ABPB vs. infraclavicular block: The infraclavicular block is quicker to perform. However, the onset time for achieving complete anesthesia is similar between the two techniques.
- ABPB vs. supraclavicular Block: There is no significant difference in performance time between ABPB and SCB. Both techniques have a similar onset time and provide surgical anesthesia within approximately the same timeframe.
3 Safety and complications
Safety is a crucial consideration when selecting an RA technique. While all regional anesthesia techniques carry inherent risks, ABPB has a lower risk of certain complications compared to supraclavicular and infraclavicular blocks.
- Pneumothorax risk: ABPB eliminates the risk of pneumothorax, a complication more commonly associated with supraclavicular and infraclavicular blocks. This makes ABPB a safer option for patients with compromised pulmonary function.
- Vascular puncture: The incidence of vascular puncture is slightly lower with ABPB compared to other blocks, though the difference is not statistically significant.
- Horner’s syndrome: ABPB has a significantly lower risk of causing Horner’s syndrome (ptosis, miosis, and anhidrosis), a condition more frequently seen with supraclavicular blocks.
4 Pain during block placement
Several studies have examined patient discomfort during block placement. Both ABPB and infraclavicular blocks show similar pain scores during administration. However, ABPB is generally better tolerated than a supraclavicular block when using nerve stimulation rather than ultrasound guidance.
5 Patient satisfaction
Patient satisfaction rates are high across all RA techniques. ABPB, infraclavicular block, and intravenous regional anesthesia all score similarly regarding overall patient comfort and willingness to undergo the same anesthesia in future procedures.
Conclusion
ABPB offers a safe and effective option for upper limb surgeries, particularly in patients who may be at higher risk for complications associated with supraclavicular or infraclavicular blocks. While infraclavicular blocks may offer slightly faster performance and a marginally higher success rate, ABPB remains a preferred choice for its safety profile and ease of administration.
Key takeaways
- ABPB is a widely used RA technique for distal upper limb surgeries, offering a high success rate and favorable safety profile.
- Infraclavicular block performs faster than ABPB, though both provide comparable onset times for surgical anesthesia.
- Compared to supraclavicular blocks, ABPB carries lower risks of serious complications, such as pneumothorax and Horner’s syndrome.
For more information, refer to the full article in the Journal of Clinical Medicine.
Nijs K, Hertogen P, Buelens S, Coppens M, Teunkens A, Jalil H, Van de Velde M, Al Tmimi L, Stessel B. Axillary Brachial Plexus Block Compared with Other Regional Anesthesia Techniques in Distal Upper Limb Surgery: A Systematic Review and Meta-Analysis. J Clin Med. 2024 May 29;13(11):3185. doi: 10.3390/jcm13113185.
Step-by-step: 3 key steps for performing an axillary brachial plexus block
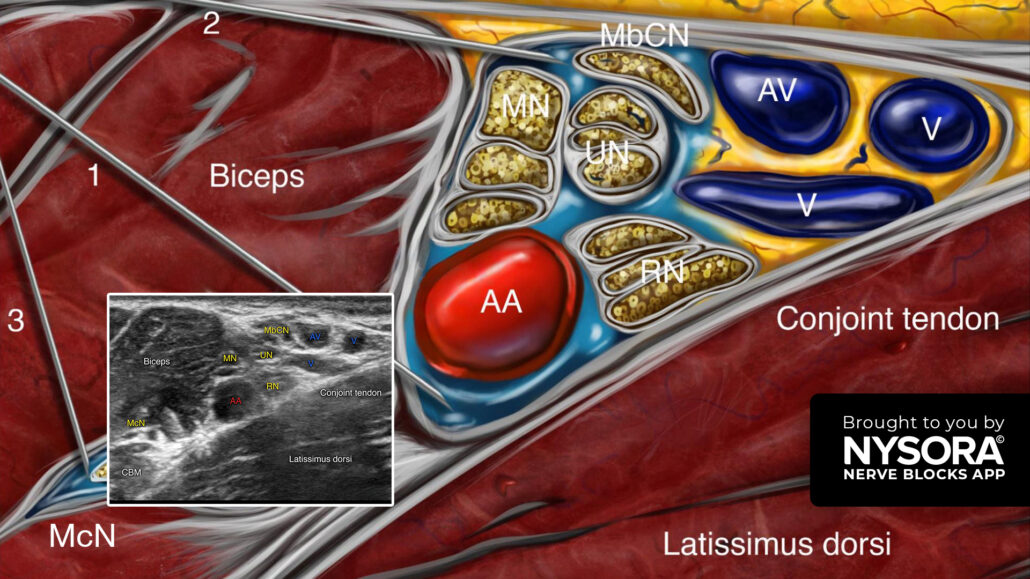
- Place the transducer in a transverse orientation over the intersection of the pectoral major and biceps muscle insertion. Do not place the transducer too high in the axillary fossa.
- Identify the axillary artery, the conjoint tendon, the neurovascular sheath containing the median, ulnar, and radial nerves, the muscles (i.e., biceps, coracobrachialis, and latissimus dorsi muscles), and the musculocutaneous nerve.
- Insert the needle in-plane, from lateral to medial, toward the axillary artery and inject 20 mL of local anesthetic (8 mL above the axillary artery, 8 mL below the axillary artery, and 4 mL for the musculocutaneous nerve).
Tip: When the musculocutaneous nerve travels together with the median nerve, it is not necessary to block this nerve with a separate injection.
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!