Tips for an Obturator Nerve Block: Distal Approach
The obturator nerve originates from the ventral rami of the L2 to L4 lumbar nerves. An obturator nerve block serves various purposes: providing supplemental analgesia for hip and knee surgeries, preventing thigh adduction response during transurethral bladder surgery, and relieving painful or permanent hip adductor spasticity.
The obturator nerve, originating from the ventral rami of the L2 to L4 lumbar nerves, plays a pivotal role in the sensory and motor innervation of the lower limbs, particularly the hip and thigh muscles. This nerve is critical in transmitting pain signals from the hip joint and facilitating muscle movements such as thigh adduction. Because of this, it has become an essential target for anesthesia in various surgical procedures and for managing certain types of chronic pain.
In clinical practice, this nerve block has proven valuable for a wide range of conditions:
- Hip and knee surgeries: Provides supplemental analgesia to reduce postoperative pain and opioid consumption.
- Bladder surgeries: Prevents the thigh adduction response (leg movement inward) that can interfere with procedures like transurethral bladder surgery.
- Spasticity management: Relieves spasticity (involuntary muscle stiffness) caused by multiple sclerosis or cerebral palsy.
The obturator nerve block can be combined with other regional anesthesia techniques, such as femoral nerve blocks, to provide comprehensive pain management during lower extremity surgeries.
In the past, obtaining precise and effective obturator nerve blocks was challenging. However, recent advancements in ultrasound-guided techniques have significantly improved the success rate. Using real-time imaging, clinicians can now accurately place the needle and ensure the anesthetic spreads appropriately around the obturator nerve. Nielsen et al. 2017 examined the spread of a local anesthetic around the obturator nerve and its branches after performing an ultrasound-guided subpectineal injection. This research aimed to determine whether the anesthetic would effectively reach the obturator nerve branches responsible for innervating the hip joint.
Key findings
- 100% success rate: In all cadavers, the methylene blue dye successfully spread to the obturator nerve and its branches within the obturator canal, effectively targeting the nerve structures that transmit pain from the hip joint.
- Accessory obturator nerve involvement: The dye also spread to the accessory obturator nerve (AON) in 21% of cases, highlighting its potential relevance in certain individuals.
- Reliable spread: The technique consistently ensured that the dye reached the key branches of the obturator nerve, particularly those supplying the hip joint, making it a reliable method for clinical use.
These findings demonstrate the technique’s potential to deliver localized pain relief in patients undergoing hip surgeries, especially those with fractures, where pain management is critical.
Benefits of an Obturator Nerve Block in Surgery and Pain Management
An obturator nerve block offers several clinical benefits, particularly when used in conjunction with other regional nerve blocks:
- Enhanced Pain Relief: This block can significantly reduce pain in the hip joint by specifically targeting the obturator nerve. It complements other blocks, such as the femoral nerve block, to provide broader pain coverage for lower limb surgeries.
- Reduced Muscle Movement: In procedures such as transurethral bladder surgery, controlling muscle movements like thigh adduction is essential. The obturator nerve block prevents unwanted leg movements, which can interfere with the surgical process.
- Management of Spasticity: For individuals with chronic conditions like multiple sclerosis or cerebral palsy, managing spasticity in the hip adductor muscles can improve mobility and reduce pain. An obturator nerve block helps alleviate this spasticity by interrupting the nerve signals that cause muscle stiffness.
- Preoperative Analgesia for Hip Fractures: The obturator nerve block is particularly useful for patients with hip fractures. By providing preoperative analgesia it helps alleviate severe pain before surgery, improving patient comfort and reducing the need for systemic pain medications like opioids.
Step-by-Step Guide to Performing an Ultrasound-Guided Obturator Nerve Block
- Patient Positioning: The patient is supine, with the leg slightly abducted and externally rotated to expose the groin area.
- Ultrasound Probe Placement: A high-frequency ultrasound probe is used to locate the space between the pectineus and external obturator muscles. This area is critical for ensuring the needle reaches the appropriate nerve branches.
- Needle Insertion: Using an out-of-plane approach, the clinician inserts a 22-gauge needle into the interfascial plane. Ultrasound guidance ensures that the needle is correctly positioned without damaging surrounding tissues.
- Anesthetic Injection: Once the needle is in place, 15 milliliters of local anesthetic are injected slowly into the interfascial space. The ultrasound probe allows the clinician to monitor the spread of the anesthetic in real-time.
- Assessment: After the injection, the clinician monitors the patient for any adverse reactions and assesses the effectiveness of the block. Surgical procedures may involve checking for numbness or reduced motor function in the thigh adductors.
Future Directions in Obturator Nerve Block Use
While the cadaveric study has shown promising results, further clinical studies are needed to explore the full potential of obturator nerve blocks in various surgical and pain management settings. Clinical trials will provide more comprehensive data on the block’s effectiveness in living patients, especially in combination with other blocks, such as femoral or lumbar plexus blocks. Moreover, understanding the variability in anatomical structures, such as the presence of the accessory obturator nerve, will allow clinicians to tailor their approach to each patient’s unique anatomy, further improving outcomes.
Conclusion
The obturator nerve block, particularly when administered using ultrasound-guided techniques, is a powerful tool in managing pain and reducing muscle movement during surgeries involving the lower limbs. The cadaveric study confirms that the anesthetic reliably reaches the obturator nerve and its branches, supporting its use in clinical practice for hip and knee surgeries, as well as for managing chronic spasticity.
For more information, refer to the full article in Regional Anesthesia & Pain Medicine.
Nielsen TD, Moriggl B, Søballe K, Kolsen-Petersen JA, Børglum J, Bendtsen TF. A Cadaveric Study of Ultrasound-Guided Subpectineal Injectate Spread Around the Obturator Nerve and Its Hip Articular Branches. Reg Anesth Pain Med. 2017;42(3):357-361.
Follow these 3 steps for an obturator nerve block using the distal approach
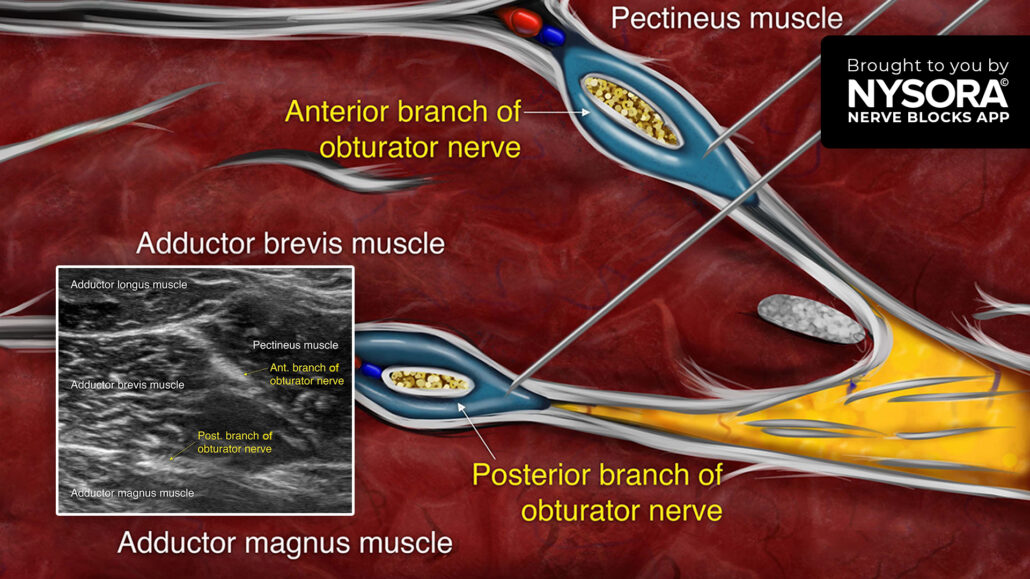
- Place the transducer in a transverse orientation perpendicular to the inguinal crease to identify the femoral vessels. Move the transducer medially along the crease to identify the pectineus, and further medially, the adductor longus, brevis, and magnus muscles.
- The anterior and posterior branches of the obturator nerve can be seen running along the fascial planes superficial and deep to the adductor brevis muscle.
- Insert the needle in-plane or out-of-plane. Inject two aliquots of local anesthetic into the fascial planes between the adductor longus and adductor brevis muscles (anterior branch) and between the adductor brevis and adductor magnus muscles (posterior branch).
Watch the video below to get a better picture of the process and see how the NYSORA Nerve Blocks App brings these instructions to life:
For more tips like these and the complete guide to the 60 most frequently used nerve blocks, download the Nerve Blocks App HERE. Don’t miss the chance to get the bestselling NYSORA Nerve Blocks App also in book format – the perfect study companion with the Nerve Blocks app!




