Tips for subclavian vein cannulation
Tips for subclavian vein cannulation
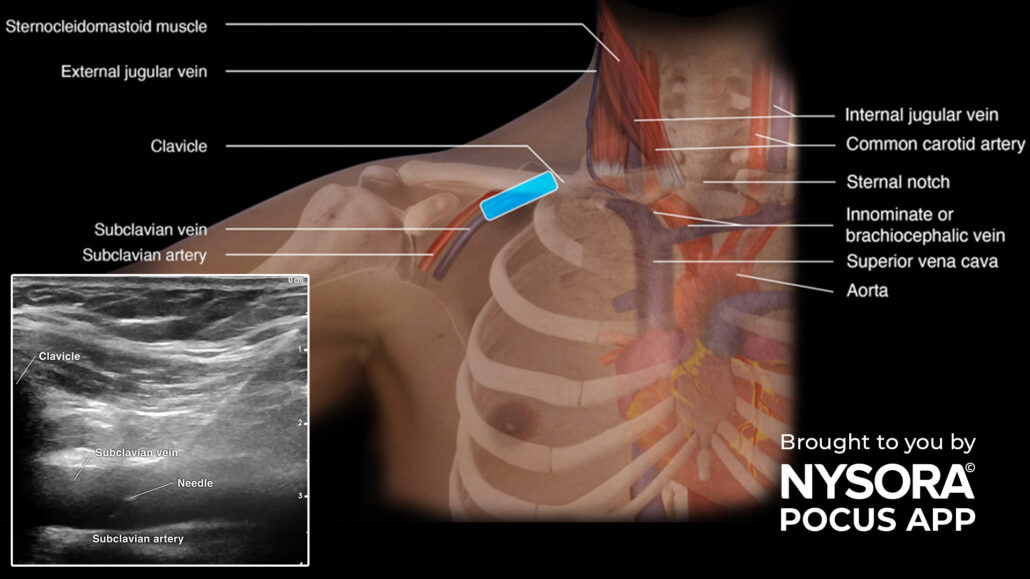
Subclavian vein cannulation is a crucial medical procedure used to access central veins for administering medications, monitoring hemodynamics, and performing advanced therapeutic interventions. By integrating point-of-care ultrasound (POCUS) into this process, healthcare providers can achieve greater precision, enhance patient safety, and significantly reduce procedural complications.
This guide provides expert tips, step-by-step instructions, and important considerations to optimize your subclavian vein cannulation technique.
What is subclavian vein cannulation?
Subclavian vein cannulation involves placing a catheter into the subclavian vein, a central vein near the clavicle. This technique is used in various clinical scenarios requiring reliable vascular access.
Common indications
- Administration of drugs, including long-term therapy or infusions.
- Fluid resuscitation
- Hemodialysis
- Monitoring central venous pressure (CVP)
- Pulmonary artery catheterization
Contraindications
- Coagulopathy or bleeding disorders.
- Infection at the insertion site.
- Thrombosis in the subclavian vein.
Preparation for subclavian vein cannulation
- Patient positioning
- Position the patient in Trendelenburg (head-down tilt) with the arm on the cannulation side abducted to 90°.
- Turn the patient’s head to the contralateral side to expose the puncture site and improve vein accessibility.
Clinical Tip: Abducting the arm creates extra working space by lifting the clavicle, making the vascular structures more superficial.
- Equipment setup
Prepare a central line insertion kit containing:
- Sterile gown, gloves, and drapes.
- Antiseptic solution (e.g., 2% chlorhexidine in 70% isopropyl alcohol).
- Ultrasound machine with a sterile transducer sleeve.
- Lidocaine 2% for local anesthesia.
- Catheters, guidewires, and dilators.
- Patient assessment
- Review the patient’s laboratory results to check for coagulation disorders.
- Examine chest X-rays for pre-existing catheters or anatomical anomalies.
- Assess the puncture site for signs of infection or obstruction.
Technique
Following a systematic approach is vital to the success of this procedure. Here’s a breakdown of the key steps:
Pre-procedural preparation
- Perform hand hygiene and don a surgical mask, hat, sterile gown, and gloves.
- Disinfect the puncture site using an appropriate antiseptic.
- Cover non-sterile areas with sterile drapes.
- Set up and flush the catheter lumens with saline.
Cannulation steps
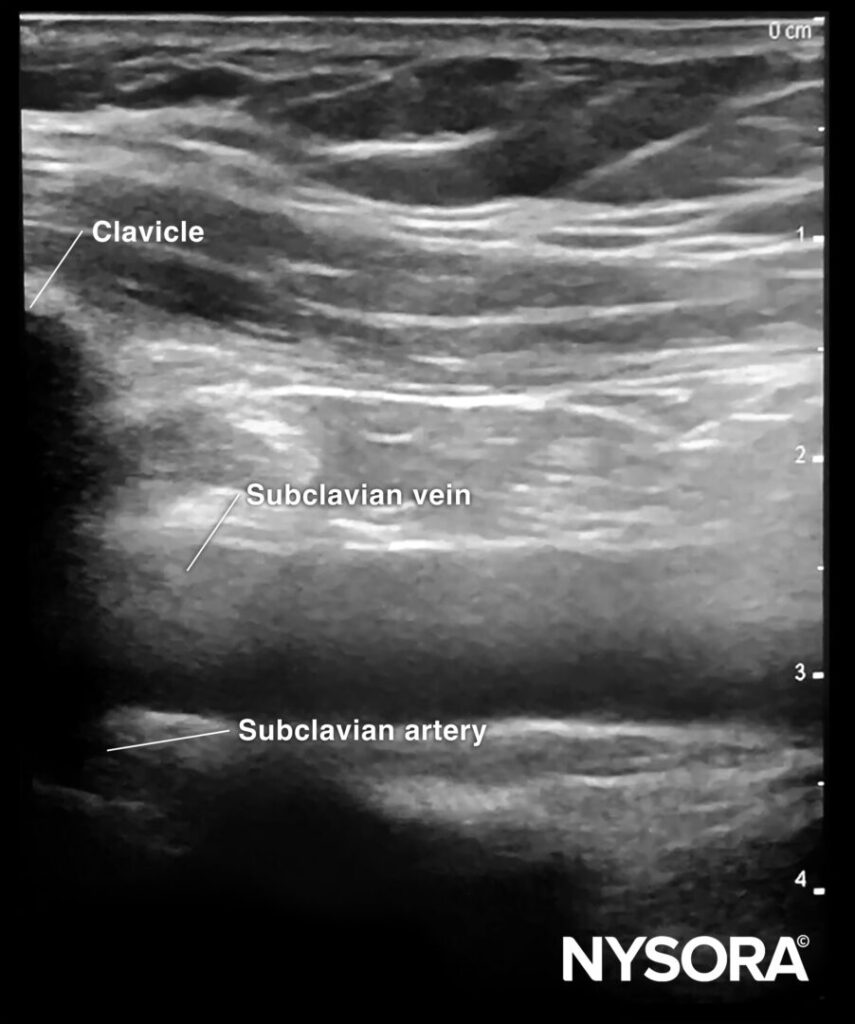
- Ultrasound preparation
- Cover the ultrasound transducer with a sterile sleeve.
- Apply sterile gel to the patient’s skin.
- Position the transducer longitudinally along the clavicle.
- Local anesthesia
- Use 5 mL of 2% lidocaine to anesthetize the puncture site if the patient is awake.
- Puncture and guidewire insertion
- Insert the needle under ultrasound guidance using an in-plane technique to visualize the full needle path.
- Confirm needle placement within the vein by aspiration of blood.
- Thread the guidewire through the needle and retract the needle while holding the guidewire in place.
- Dilation and catheter placement
- Make a small incision at the puncture site to facilitate catheter insertion.
- Use a dilator to enlarge the puncture site and thread the catheter over the guidewire.
- Advance the catheter into the vein and remove the guidewire.
- Verification
- Confirm catheter placement using ultrasound to check the position of the guidewire.
- Perform a lung ultrasound to assess lung sliding and rule out pneumothorax.
- Check for the rapid atrial swirl sign (RASS) via cardiac ultrasound to confirm proper catheter placement.
- Finalization
- Aspirate blood from all lumens to confirm patency and flush with saline.
- Suture the catheter securely to the skin.
- Apply a sterile dressing to the site.
Expert tips for subclavian vein cannulation
- Before starting, identify key anatomical landmarks (vein, artery, pleura, ribs).
- Use ultrasound guidance to reduce complications compared to blind techniques.
- For small or flattened veins in intubated patients, apply the Valsalva maneuver or increase positive end-expiratory pressure (PEEP) to distend the vein.
- Always combine subclavian vein cannulation with lung and cardiac ultrasound to confirm catheter placement and rule out complications.
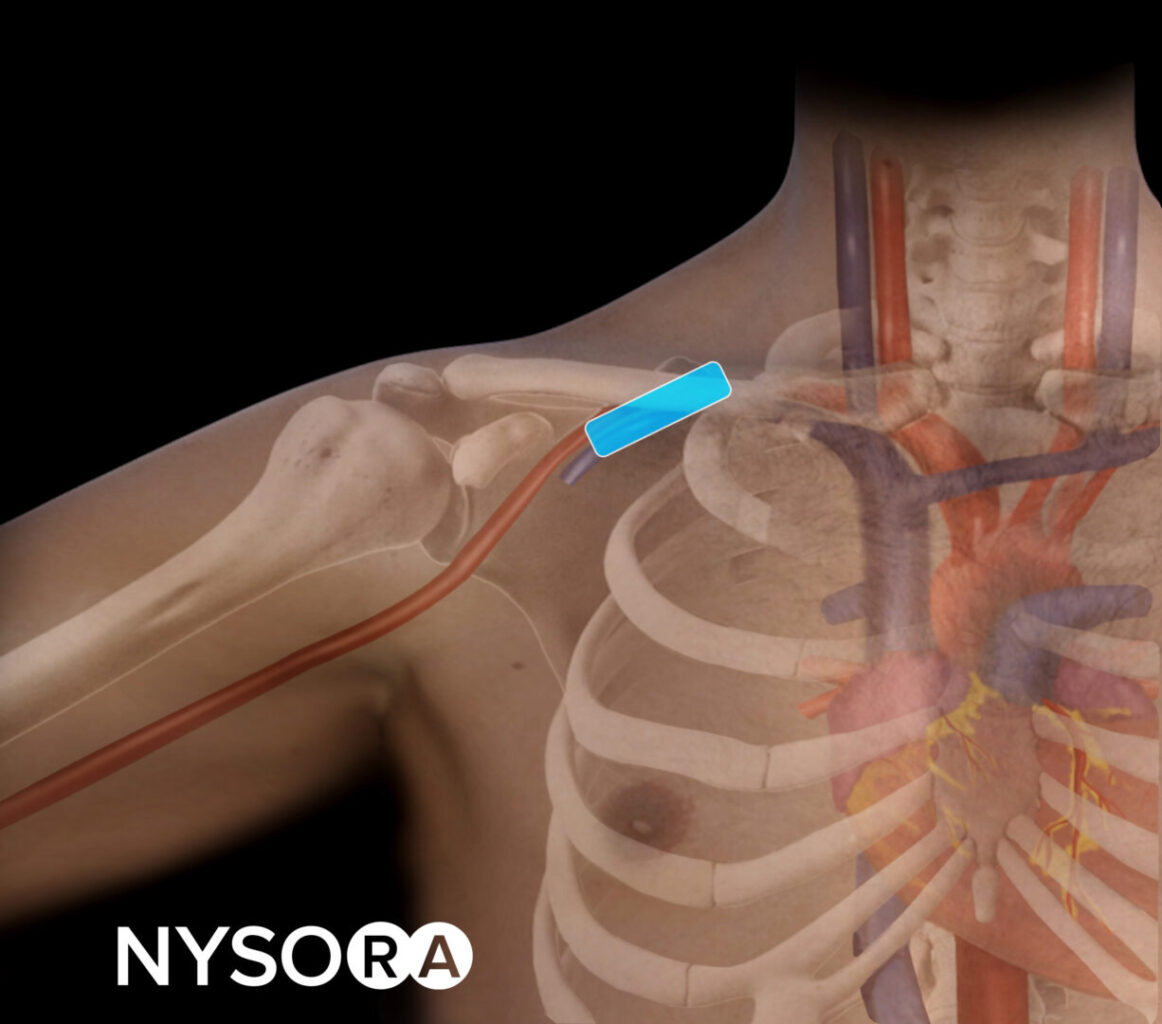
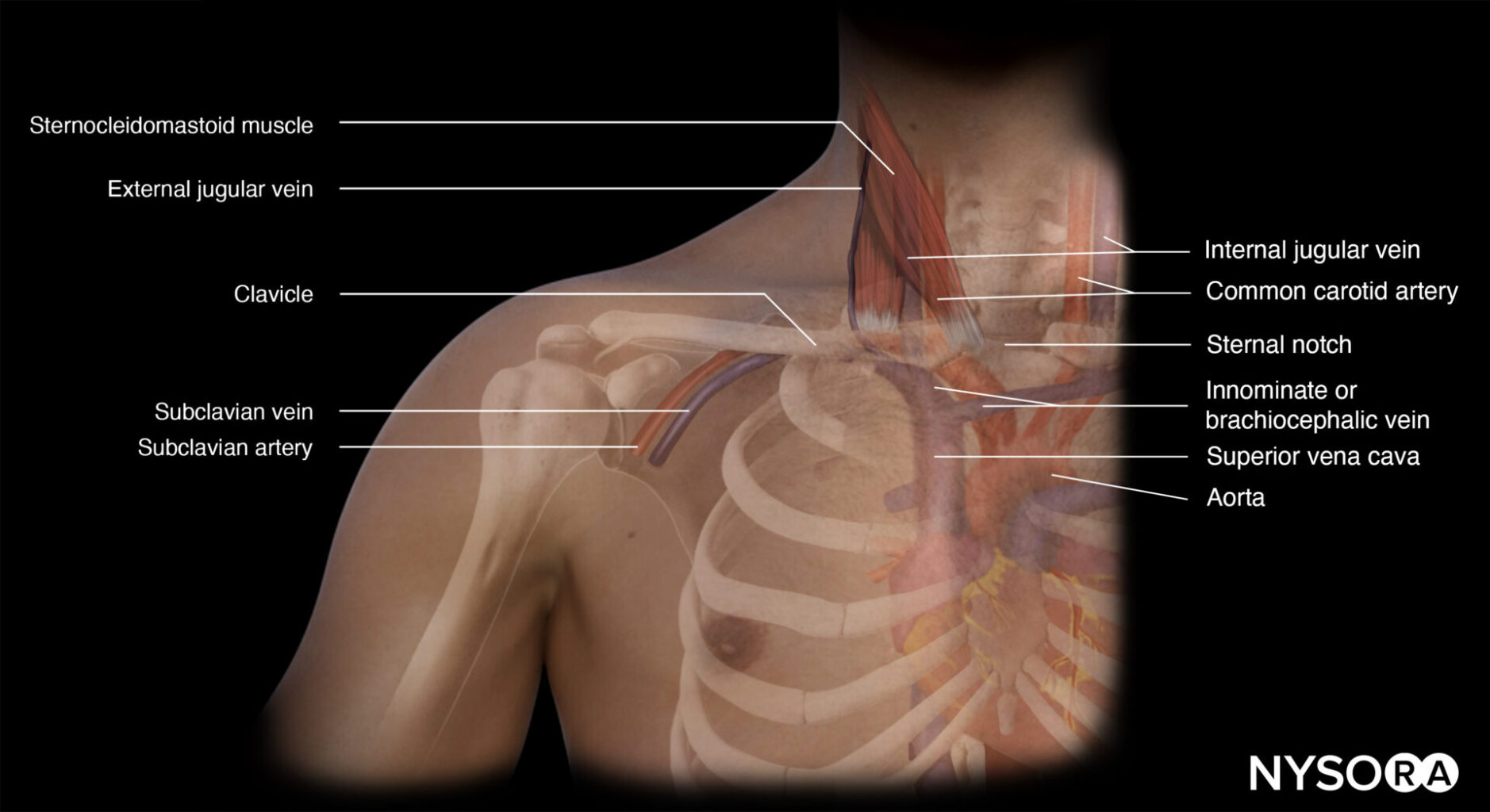
Anatomy overview
Relevant structures
- Subclavian vein: Located beneath the clavicle, parallel to the subclavian artery.
- Pleura: The thin membrane surrounding the lungs should be avoided during cannulation.
- Clavicle: Acts as an external landmark for transducer placement.
Ultrasound orientation
- Place the ultrasound transducer longitudinally along the clavicle near the deltopectoral groove.
- Rotate the transducer to align the vein with the ultrasound beam.
Safety considerations
- Monitor the patient’s oxygenation, blood pressure, and heart rate throughout the procedure.
- Apply full ASA monitoring to detect complications like desaturation or arrhythmias.
- If the attempt fails, reassess the anatomy using ultrasound and consider alternative sites (e.g., internal jugular vein).
By following these tips and techniques, you can perform subclavian vein cannulation with confidence, precision, and safety. Incorporating ultrasound guidance is key to reducing complications and achieving optimal patient outcomes.
Enhance your skills with POCUS
Transform your practice with NYSORA’s POCUS App. This advanced tool provides comprehensive guidance for ultrasound procedures, enhancing diagnostic capabilities and patient care.
Download the app Here.