|
Combined Suprascapular and Axillary (Circumflex) Nerve Block: The Shoulder Block
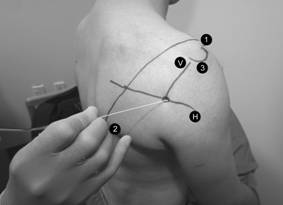
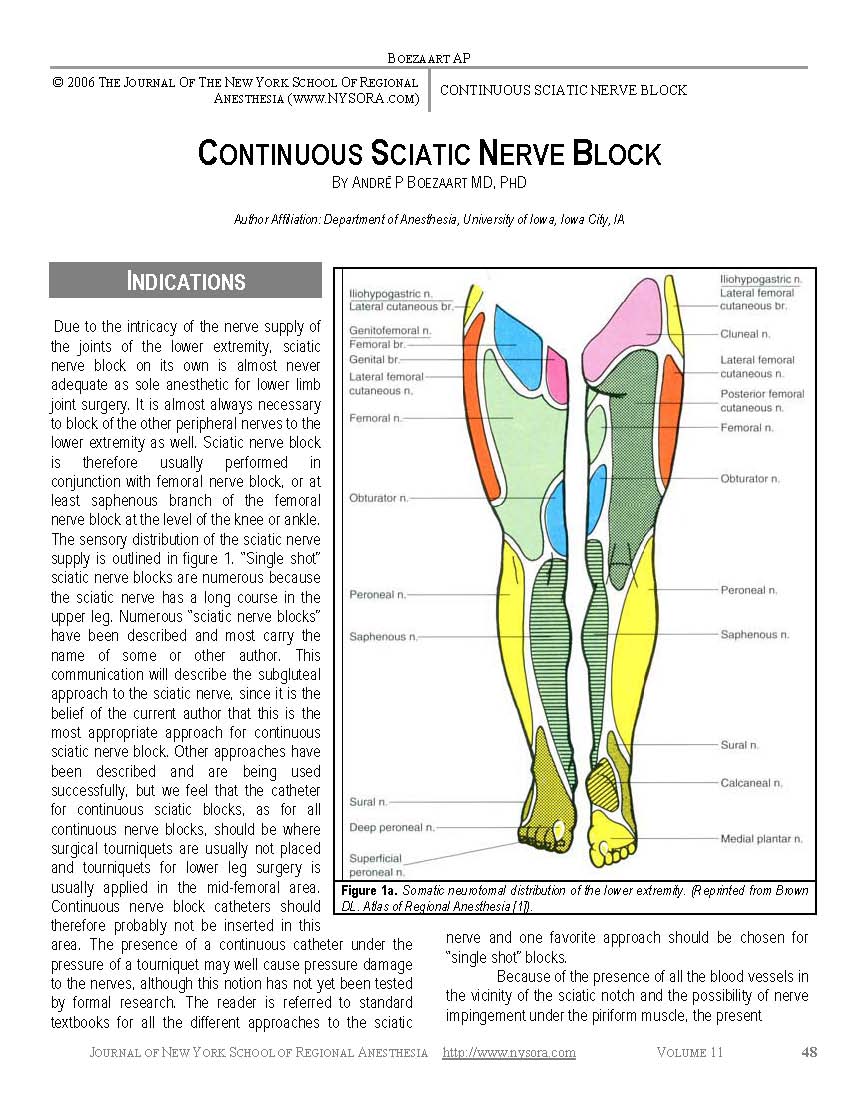
Introduction Traditionally, the interscalene approach to the brachial plexus has been employed to manage postoperative pain following shoulder surgery. Because this technique involves local anaesthetic deposition around the lower cervical nerve roots, it is associated with a number of significant adverse effects. These include temporary side effects associated with spread to adjacent nervous tissue, such as phrenic nerve paralysis, Horner’s syndrome and hoarseness. The associated motor block can be quite extensive, with the entire shoulder girdle paralysed, and on many occasions, also the arm and hand. There are also rare but severe complications caused by inadvertent injection of local anaesthetic into the adjacent CSF, epidural space or vertebral artery. Transient neurological complications are relatively common (14% at 10 days), while permanent damage to the part of brachial plexus can occur in 1 in 500 cases. So avoiding the above adverse effects and still provide adequate analgesia following shoulder surgery would be a good thing. The interscalene technique provides effective shoulder anaesthesia as the C5 and C6 nerve roots are blocked. However, the bulk of nerve supply from C5and 6 is transported to the shoulder joint by just two nerves, the suprascapular and the axillary. There are actually 5 terminal nerves supplying the shoulder joint, with the lateral pectoral, subscapular and musculocutaneous nerves all having a much smaller contribution. The suprascapular nerve will have the largest contribution, and block of this nerve alone has been attempted to control pain following shoulder surgery. Studies have shown it to be more effective that intra-articular local anaesthesia, but somewhat inferior to an interscalene block, and maybe indicated if an interscalene block is contraindicated. So it should follow that blocking both the axillary nerve and the suprascapular nerve may more closely resemble the analgesia achieved with an interscalene technique. That was the question I asked myself in 2005 when some of my patients who had received a surgeon administered suprascapular nerve block (by the lateral approach) following surgery were often still in significant pain. As no description of axillary nerve block was currently available, I developed a technique of my own after reviewing anatomy textbooks, skeletons, MRI scans and a wet dissection of the associated anatomy. My initial description of the technique has been landmark based, and employing a nerve stimulator, and I have found it quick, safe and reliable to perform this way. However, I have endeavoured to add a description using ultrasound, as many anaesthetists are starting to drop nerve landmarks and nerve stimulators from their practice. Before anyone begins using the shoulder block technique, it is important to appreciate that, in contrast to the interscalene block, you must expect and manage a degree of residual pain, and that this is going to vary between patients. This situation is, however, not dissimilar to using a femoral nerve block for major knee surgery, where some patients require additional analgesia due to variable innervation by the sciatic nerve. It also means that the block should always be used in conjunction with a general anaesthetic. Indications: The vast majority of cases I employ this technique block preoperatively are for arthroscopic shoulder surgery where the patients are able be managed effectively with oral analgesic on the first day postoperatively. Thus it is used for minor subacromial procedures such as subacromial decompression, or intraarticular procedures such as stabilisation procedures requiring labral repair, and acromioclavicular joint reconstruction. I will also use the block in arthroscopic or open rotator cuff surgery, or major open shoulder surgery, where an interscalene block is relatively or absolutely contraindicated, such as with sever respiratory disease or morbid obesity. The one shoulder procedure that I would not consider using the technique is rotator cuff surgery involving the subscapularis, as this muscle is not covered by the shoulder block. The block also has several postoperative indications, such as interscalene block failure, either in PACU or on the ward (eg interscalene catheter displacement or significant pain following resolution of a single shot technique). Anatomy: Effective control of post-surgical shoulder pain generally requires local anaesthetic block of the nerve supply to the synovium, capsule, articular surfaces, periosteum, ligaments and muscles of the shoulder joint 1. These structures receive sensory innervation from the nerves that supply the muscles working across the glenohumeral articulation. As mentioned above, five nerves are responsible. 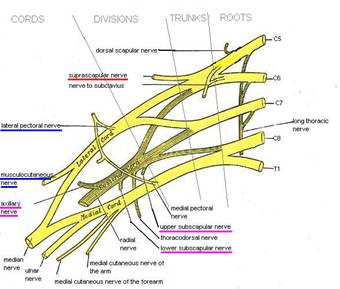 Figure 1
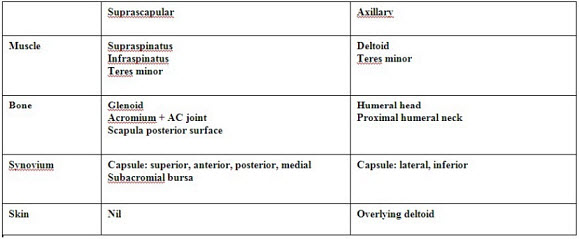
The suprascapular nerve is a branch of the superior trunk. Its courses postero-laterally towards the suprascapular notch on the upper border of the scapular to the supraspinous groove, where it lies beneath the tendon of supraspinatus. It then winds around the greater scapular notch to terminate within infraspinatus. Motor supply is to supraspinatus and infraspinatus muscle of the rotator cuff, with some branches to teres minor. It provides sensation to bulk of the posterior, medial and superior joint capsule, and innervates the following bone structures: glenoid, acromium, posterior surface of scapula. The axillary nerve is formed as a terminal branch of the posterior cord at the lateral border of subscapularis, as it winds towards the posterior aspect of the surgical neck of the humerus (Figures 1 and 2). It runs beneath the shoulder joint only 2 to 3mm below the inferior capsule. In association with the posterior humeral circumflex artery the nerve passes back through the quadrilateral space, a small opening formed by teres minor above, teres major below, long head of biceps medially and the proximal humerus laterally. Motor innervation is primarily to the deltoid, with branches to teres minor. It provides sensation to the inferior, lateral and anterior joint capsule, and innervates the humeral head, upper humeral neck. It also has a cutaneous branch, supplying the skin over the deltoid. The subscapular nerve(s) are a terminal branch of posterior cord, supplying the fourth rotator cuff muscle, the subscapularis, upon which the posterior cord lies. The nerve also provides sensation to the anterior joint capsule, and the anterior glenoid and the anterior surface of the scapula. The lateral pectoral and the musculocutaneous nerves are both branches of the lateral cord. They both assist the suprascapular nerve in supplying sensation the anterior joint capsule. The lateral pectoral nerve also supplies the pectoralis major and minor, while the musculocutaneous nerve’s motor supply within the shoulder joint is to the long head of biceps.
Chart 1
Chart 2
Figure 2: Chart 1 & Chart 2 Techniques: Equipment: A 100mm 22G insulated stimulating needle will be required used for block of both nerves, either by the landmark or by the US guided technique. A. Landmark techniques This is best performed in the sitting position, with the shoulder in full adduction. 1. Suprascapular nerve block: technique of Meier The ideal approach to the nerve would ensure block of the more proximal branches to the acromium and the subacromial region. block of the nerve in the suprascapular notch does achieve this, but is associated with a small risk of pneumothorax 8,19,20. The technique chosen was that described by Meier, which allows block of the suprascapular nerve during its passage from the suprascapular notch to the spinoglenoid notch, as it lies in the lateral supraspinous groove 19,20. It also allows a large volume of local anaesthetic to be injected beneath the supraspinatus muscle, as well as the option of inserting a catheter.
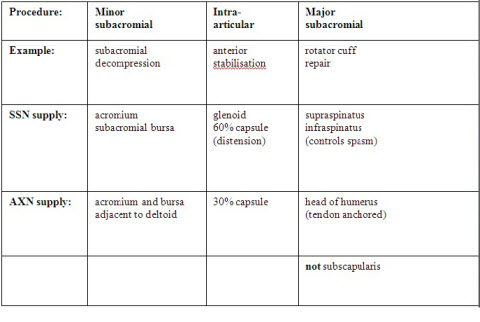
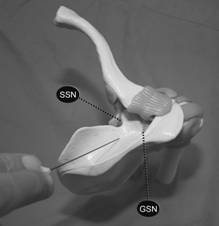
Figures 3 and 4. Cutaneous markings of suprascapular nerve block of Meier, and superior view of the supraspinatous fossa. The suprascapular nerve enters the groove at the suprascapular notch (SSN) and winds laterally around the greater scapular notch (GSN). Figures 3 and 4 illustrate the technique of Meier 19,20; the patient is in the sitting position with the arm in full adduction. A line connecting the lateral part of the acromium and the medial end of the spine of the scapula is identified. The insertion point is located 2cm medial and 2cm cephalad to the midpoint of this line. A 10cm insulated needle is inserted 4 to 6 cm lateralocaudally (45° in the coronal plane), with a ventral inclination of about 30°. If stimulation of the infraspinatus muscle is observed, or the patient reports a pain free ‘knocking’ sensation in the shoulder, 10 to 15ml of long acting local anaesthetic is injected 19,20. If no twitches were elicited, the LA is injected along the bony surface of the lateral supraspinous groove. 2. Axillary nerve block: technique of Price The safest and most consistent point at which to block the axillary nerve is immediately following the nerve’s passage through the quadrilateral space to lie on the posterior surface of the humerus. It avoids injection more proximally where the nerve lies only 2 to 3 mm below the inferior capsule, carrying a risk of entering the joint with the block needle. The technique relies on bony landmarks that are easily palpated in almost all patients, and are consistent between patients. As for the suprascapular nerve block, the patient is seated with the arm in full adduction. a. Horizontal plane Both the anterior aspect of the acromium and the inferior angle of the scapula are palpated. A line directly joining these two landmarks points is drawn across the skin (Figure 5). The midway point along this line is identified and marked with a horizontal line. The quadrilateral space lies at the level of this horizontal plane (Figure 2 and 6). b. Vertical plane The postero-lateral aspect of the acromium is palpated, and from this point a vertical line is traced down, directly behind the humerus (Figure 5). This represents a vertical plane through which the axillary nerve passes laterally, at the level of the horizontal plane. The point on the skin at which the vertical plane and the horizontal plane intersect designates the needle puncture point (Figure 2 and 6).
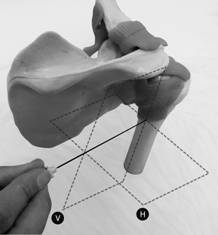 Figure 6
Figures 5 and 6. The axillary nerve block of Price. A line connects the anterior acromium (1) with the inferior angle of the scapula (2). The midpoint represents the level of he horizontal axis (H) at which the quadrilateral space lies. The line representing vertical axis (V) is drawn down from the postero-lateral aspect of the acromium (3). A 10cm insulated needle is passed directly anterior from this intersect towards the posterior aspect of the humerus, in line with both the horizontal and the vertical planes. Twitches in the posterior deltoid may occur after 2 to 3cm due to direct stimulation as the needle passes through that muscle. Muscular twitches involving the anterior deltoid at a depth of 6 to 8cm indicate the axillary nerve has been located. 10 to 15 ml long acting local anaesthetic is then injected. Confirming that the deltoid twitch are anterior and result from a needle pass deep enough to contact the posterior humerus are critical to block success with a nerve stimulator. If no twitches are elicited, the needle can be walked up and down in the vertical plane along the posterior surface the humerus, avoiding perforating the shoulder capsule superiorly. If twitches are still not elicited 10 to 15ml of LA can be deposited beneath the deltoid on the posterior surface of the humerus at the initial entry point. Contact with soft tissue when advancing onto the humerus, indicates the needle tip is lying within the origin of the lateral head of triceps. The needle should be withdrawn 1 cm and walked superiorly in the vertical plane until free bone is contacted, or until deltoid twitch indicates the axillary nerve has been located. 10 to 15 ml of local anaesthetic is then injected slowly. The direction of local anaesthetic spread during axillary nerve block is illustrated with the use of radio-opaque dye (Figures 7a and 7b).
Figures 7a and 7b. Following injection of 15ml of local anaesthetic plus radio-opaque dye the injectate can be seen to fill a potential space beneath the posterior deltoid. Medially the injectate fills the conical structure of the quadrilateral space. Thirty seconds later the injectate has passed medially through the quadrilateral space and inferior to the glenohumeral joint capsule. The dye can be seen filling a potential space that would correspond to the medial aspect of the subscapularis muscle upon which the axillary nerve crosses after branching off the posterior cord. B. Ultrasound guided technique. Because both nerves lie on bone, the landmark technique allows efficient performance of the block. Thus any US guided technique would have to retain those advantages. However, as both nerves, and their accompanying arteries and veins, are both small and relatively deep, the US guided approach is simplified by using the same landmarks as for the landmark techniques, namely the adjacent bone. Either a high frequency or curvilinear can be used. The ultrasound technique is probably more easily performed in the lateral position, again with the shoulder in full adduction. 1. Suprascapular nerve. The best approach is to image the floor of the supraspinous fossa along its long axis, including the point at it becomes the greater suprascapular notch. Overlying will be the supraspinatus and the trapezius muscles. The needle approach is in plane, and its final position will be very similar to the landmark technique, with LA injected upon contacted the lateral aspect of the supraspinous fossa, beneath supraspinatus. The suprascapular nerve and artery may be visible either before or after injection of LA. 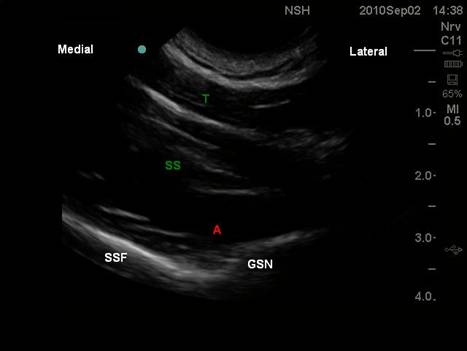 Suprascapular nerve
2. Axillary nerve. The most reliable approach is to image the posterior surface of the humerus in its long axis. This will allow a short axis view of the circumflex artery and the axillary nerve. The artery is the most reliable landmark, and LA injected adjacent to this on the posterior surface of the humerus will fill a potential space beneath the deltoid muscle. If the artery is not visible, follow the periosteum cephalad until it merges with joint capsule. Injection of LA 1 cm caudal to this should be in the vicinity of the axillary nerve. If the US images are poor, a nerve stimulator will assist location of the axillary nerve. 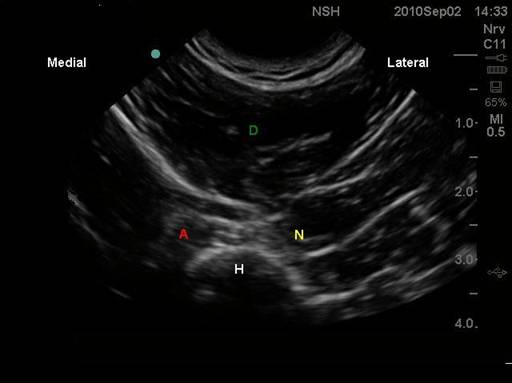 Axillary nerve
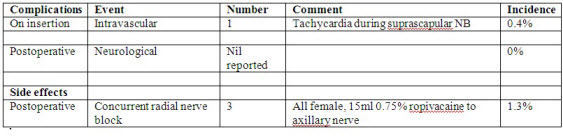
Supplemental analgesia requirement As discussed above, the shoulder block does not anaesthetise all 5 nerves supplying the shoulder joint, so I routinely give supplemental opiate intraoperatively to all my patients receiving this technique. The immediate postoperative analgesia requirements do vary between patients, most likely reflecting variations in the pattern of innervation of the shoulder joint, much like what we observe in the knee joint when using a femoral nerve block. Thirty seconds later the injectate has passed medially through the quadrilateral space and inferior to the glenohumeral joint capsule. The dye can be seen filling a potential space that would correspond to the medial aspect of the subscapularis muscle upon which the axillary nerve crosses after branching off the posterior cord. Some patients (maybe 50%) will have minimal if any pain, while others will need between 5 and 10mg of morphine between theatre and recovery. A small number may need a bit more. What has become apparent, however, is that virtually all patients will find their pain recedes significantly over the first two hours postoperatively. The only explanation I can propose is that much of the residual pain is due to the stretching of the shoulder capsule with arthroscopic fluid, which must recede over the initial postoperative period. Meanwhile, the pain arising from surgery to the shoulder joint structures is well covered by combined suprascapular and axillary nerve block. Side effects and complications: The adverse effects from the authors first 230 cases were reviewed and divided into three categories: insertion complications, side effects and long term complications. Both insertion complications and side effects were assessed and recorded by the author during block insertion, and 1 to 2 hours following surgery respectively. Long term complications of interest were neurological in nature, related to either a deficit or neuropathic-type pain. While follow-up was not standardized, 198 of the 230 cases involved the same surgeon who was aware that the technique had been used. The complications and side effects are listed in Table 2. Thus I have found this technique very useful for day case surgery, where my patients are discharged home 2 hours following surgery with little pain and virtually no side effects. In comparison, the interscalene block would result in patient with nil pain, but the side effects due to the block are still very apparent two hours postoperatively
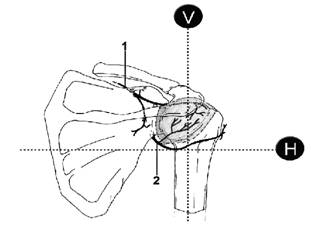
Chart 3
Only one insertion complication was noted, a presumed intravascular injection. There were no neurological complications bought to the attention of the author by any of the surgical teams following up the patients. Side effects following the technique were limited to three cases of concurrent radial nerve block associated with the axillary nerve block. The cause of this was local anaesthetic tracking proximally to the posterior cord. Helpful comments: 1. Rotator cuff surgery involving the subscapularis muscle will not be covered by this technique. 2. Be prepared to manage residual pain in PACU. Fortunately it only most cases it recedes significantly over the 3. Anterior deltoid twitch is critical when using a nerve stimulator to locate the axillary nerve. Future directions: 1. I have underway a randomised trial comparing single shot shoulder block versus single shot interscalene in minor subacromial and intra-articular arthroscopic surgery. Primary end point is quality of pain, secondary endpoints include side effects. 2. I am currently developing a technique (ie a 3rd injection) that may separately block the anterior articular that supply the anterior shoulder joint capsule with a single injection of ropivacaine along the anterior neck of the glenoid. This may have the potential to further reduce postoperative pain without causing any major complications or side effects such a shooter block in the upper limb. 3. My next RCT will compare the shoulder block versus the interscalene technique for rotator cuff surgery. I will be using a catheter technique for the interscalene block, but will only be placing a catheter in the suprascapular nerve component of the shoulder block, with just a single shot technique for the axillary nerve component. |