Comparing proximal and distal approaches for intercostobrachial nerve block in upper arm surgery
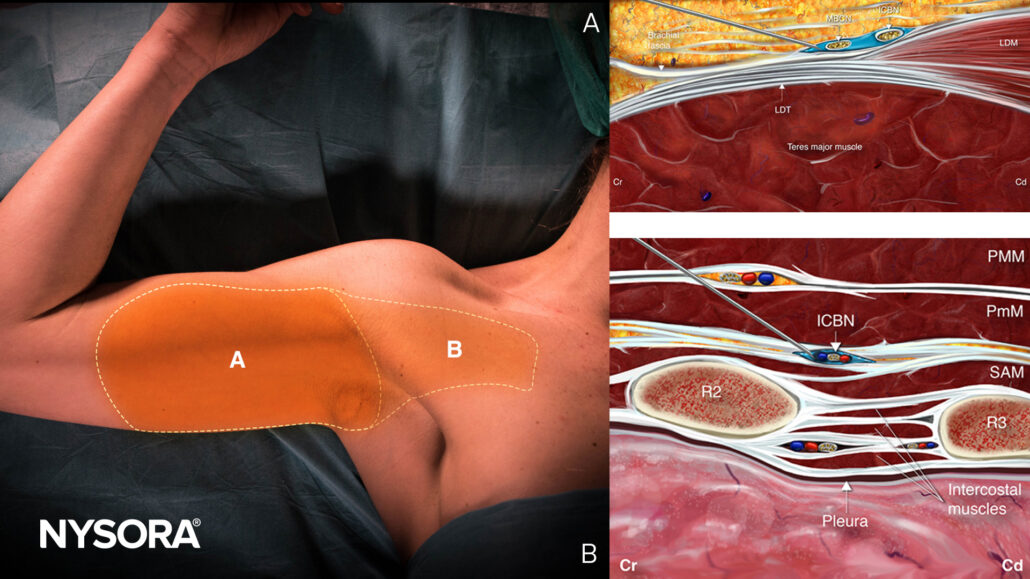
With the increasing prevalence of end-stage renal disease (ESRD), patients often require repeated upper arm arteriovenous (AV) access procedures for hemodialysis. Effective anesthesia techniques are essential for these surgeries, as they must cover specific areas of the upper arm and axilla while minimizing discomfort and improving patient outcomes. The intercostobrachial nerve (ICBN) block, commonly paired with a supraclavicular brachial plexus block, is one approach that helps anesthetize the medial upper arm and axilla. However, the effectiveness of this block can vary depending on the approach. A recent study compared two ultrasound-guided approaches—proximal and distal ICBN blocks—to determine their efficacy in achieving a successful sensory block.
Study objective and methods
The study aimed to evaluate the effectiveness of proximal versus distal ICBN block approaches in providing adequate anesthesia during upper arm AV access surgeries. This randomized controlled trial included 60 ESRD patients who were randomly assigned to receive either a proximal or distal ICBN block, both administered as adjuncts to a supraclavicular brachial plexus block. Patients and outcome assessors were blinded to the block type to ensure objectivity. The anesthetic mixture for each block was 10 mL of a solution containing 0.25% levobupivacaine, 1% lidocaine, and 2.5 µg/mL epinephrine.
- Proximal ICBN block: This approach was applied near the second rib on the chest wall, targeting the point where the ICBN branches from the lateral cutaneous nerve.
- Distal ICBN block: This approach was delivered on the medial side of the upper arm, approximately 3-4 cm below the axilla.
The primary outcome was achieving a successful sensory block in both the medial upper arm and axilla. Secondary outcomes included block performance, complications, and the need for additional anesthesia.
Key findings
- Sensory block: The proximal approach achieved significantly higher sensory block in the axilla, with a success rate of 96.7% compared to 73.3% in the distal approach (p = 0.03). Both approaches had similar sensory block rates in the medial upper arm, each at 96.7% (p = 1.00).
- Overall success rate: The proximal approach demonstrated a higher overall success rate of 96.7% versus 73.3% in the distal approach, reflecting a difference of 23.3% (95% CI: 6.3%, 40.4%; p = 0.03).
- Surgical anesthesia: Both groups had similar rates of achieving surgical anesthesia when combined with the supraclavicular block, each at 93.3%, showing that both methods are adequate for surgery (p = 1.00).
- Efficiency and safety: No significant differences were observed in performance time, procedural pain, or postoperative pain intensity between the groups, underscoring the safety and efficiency of both approaches.
Conclusion
The findings suggest that the proximal ICBN block may be preferable when axillary anesthesia is specifically required, as it has a higher success rate in providing complete sensory coverage of the axilla. This could make the proximal approach particularly valuable in procedures involving the axillary region. However, with similar surgical anesthesia rates between the groups, both the proximal and distal approaches, when combined with the supraclavicular block, offer effective pain control for upper arm AV access surgeries. This flexibility can be beneficial for clinicians, allowing them to choose the most appropriate technique based on the patient’s anatomy, access site, and surgical needs.
Future research
Further research could explore the effectiveness of these approaches in surgeries with greater axillary involvement and assess optimal injection volumes and techniques.
For more detailed information, refer to the full article in RAPM.
Samerchua A, Supphapipat K, Leurcharusmee P, et al. Randomized comparison between ultrasound-guided proximal and distal approaches of intercostobrachial nerve block as an adjunct to supraclavicular brachial plexus block for upper arm arteriovenous access procedures. Reg Anesth Pain Med. Published online October, 24 2024.
Download the Nerve Blocks App HERE for in-depth insights on the intercostobrachial nerve block. Prefer a physical copy? The bestselling NYSORA Nerve Blocks App is available in book format — an essential resource for mastering nerve blocks!