Case Study: Complex Regional Pain Syndrome
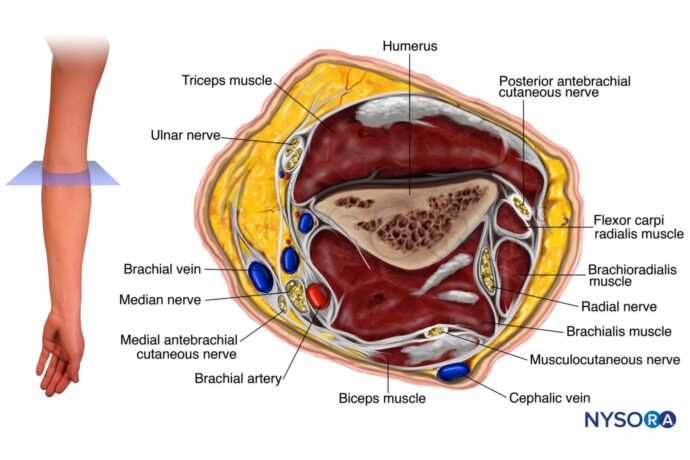
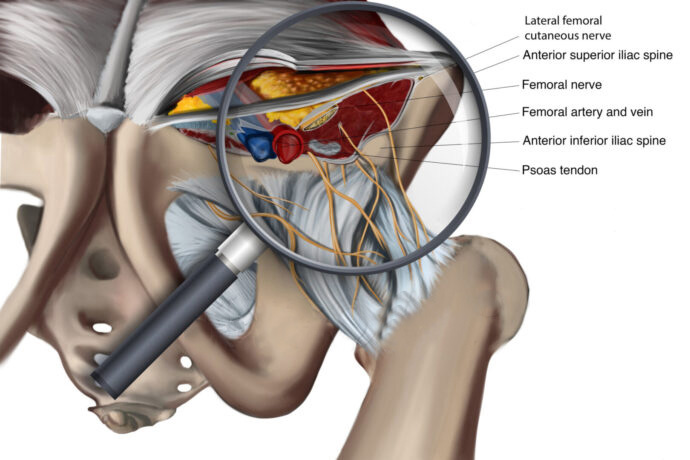
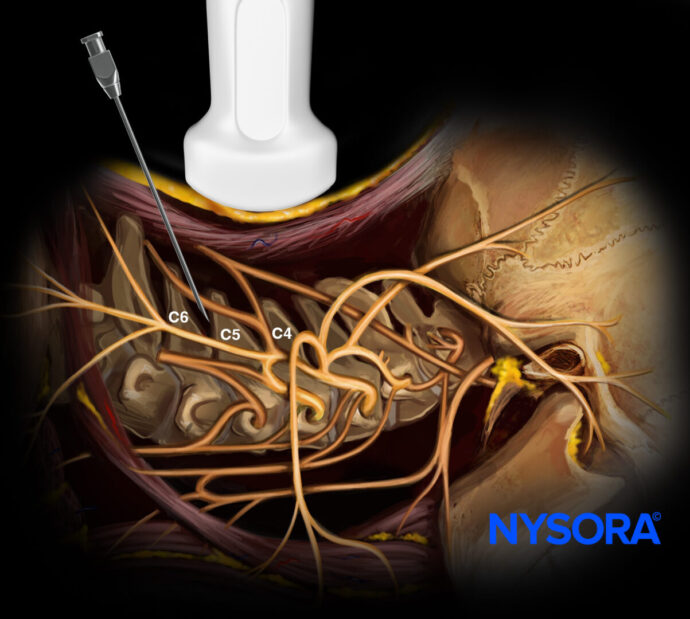
Case Presentation A 56-year-old diabetic woman presents with a two-year history of increasing right shoulder pain, stiffness, night pain, and upper limb swelling, significantly impacting her ability to perform household tasks. Diagnosis Physical Exam Findings Painful shoulder abduction Painful external rotation Painful arc present Positive O’Brien’s Test Clinical Observations Edematous right upper limb Shiny, pale, and cold skin, suggestive of complex regional pain syndrome (CRPS) Laboratory and Imaging Studies Fasting Blood Sugar: 188 mg% Hemoglobin A1c: 9.0% Normal ESR and CRP Normal Nerve Conduction Study and Doppler X-ray: Rotator cuff arthropathy Ultrasound: Rotator cuff tendinopathy, supraspinatus tendinopathy Final Diagnosis Adhesive Capsulitis (Frozen Shoulder) Rotator Cuff Tendinopathy Complex Regional Pain Syndrome (CRPS) CRPS Diagnosis Budapest Criteria To diagnose CRPS, the patient must have at least one symptom in three of the following categories and one sign in two or more categories: Symptoms: Sensory: Hyperesthesia, allodynia Vasomotor: Temperature asymmetry, skin color changes Sudomotor/Edema: Edema, sweating changes Motor/Trophic: Decreased range of motion, motor dysfunction, trophic changes Signs: Sensory: Hyperalgesia, allodynia Vasomotor: Skin temperature asymmetry, skin color changes Sudomotor/Edema: Edema, sweating changes Motor/Trophic: Decreased range of motion, motor dysfunction, trophic changes CRPS Overview Complex Regional Pain Syndrome (CRPS) is a chronic pain condition affecting one limb, often after injury. Symptoms include severe pain, sensitivity to touch, temperature changes, skin color changes, and swelling. Early diagnosis and intervention are crucial. Treatment includes physical therapy, pain medications, nerve blocks, and psychological support. Conclusion Understanding and diagnosing CRPS early is vital for managing symptoms effectively. Proper clinical evaluation and diagnostic criteria, such as the Budapest Criteria, are essential for accurate diagnosis. For more detailed information on CRPS and how Dr. Madhan Pandian treated this patient, download NYSORA’s US Pain app!