Continuous peripheral nerve block (CPNB) catheters, also known as “perineural” catheters, extend the potential duration of anesthesia and analgesia provided by peripheral nerve block techniques. In the ambulatory setting, the use of CPNB has been shown to increase the quality of pain control experienced by patients at home and to reduce the incidence of side effects produced by conventional opioid analgesics [1–3]. For hospitalized patients, CPNB techniques have similarly demonstrated postoperative analgesia efficacy following major surgery [4–7], facilitating early rehabilitation [4, 8], and shortening the time to achieve hospital discharge criteria in arthroplasty patients [6, 7, 9]. In select patients, joint replacement with only overnight hospitalization and outpatient management of perineural infusions is feasible [10–12] and offers potential economic benefits [13]. The use of electrical nerve stimulation guidance for CPNB performance, employing either stimulating or nonstimulating perineural catheters, is well established [1, 2, 14–16], but ultrasound guidance has emerged as a reliably effective and efficient technique for perineural catheter insertion [17–23].
1. APPLICATIONS
Ultrasound-guided CPNB techniques may be performed in a variety of locations: along the brachial plexus [17, 18, 22– 25], femoral nerve [21, 26, 27], sciatic nerve [19, 22, 27, 28], paravertebral space [29], and ilioinguinal and iliohypogastric nerves [30], as well as within the transversus abdominis plane [31, 32]. Essentially, perineural catheters for continuous local anesthetic infusion may be placed in the vicinity of nearly all peripheral nerves using ultrasound guidance. To date, most published ultrasound-guided perineural catheter insertion techniques share a common step of injecting fluid via the placement needle around the target nerve under direct visualization, creating sufficient space for subsequent catheter insertion [17, 19–22]. The specific techniques differ mainly in the choice of needle insertion site and trajectory relative to transducer position (in-plane versus out-of-plane) and transducer orientation relative to the target nerve (shortaxis versus long-axis) [33, 34].
2. OVERVIEW OF ULTRASOUND-GUIDED PERINEURAL CATHETER INSERTION
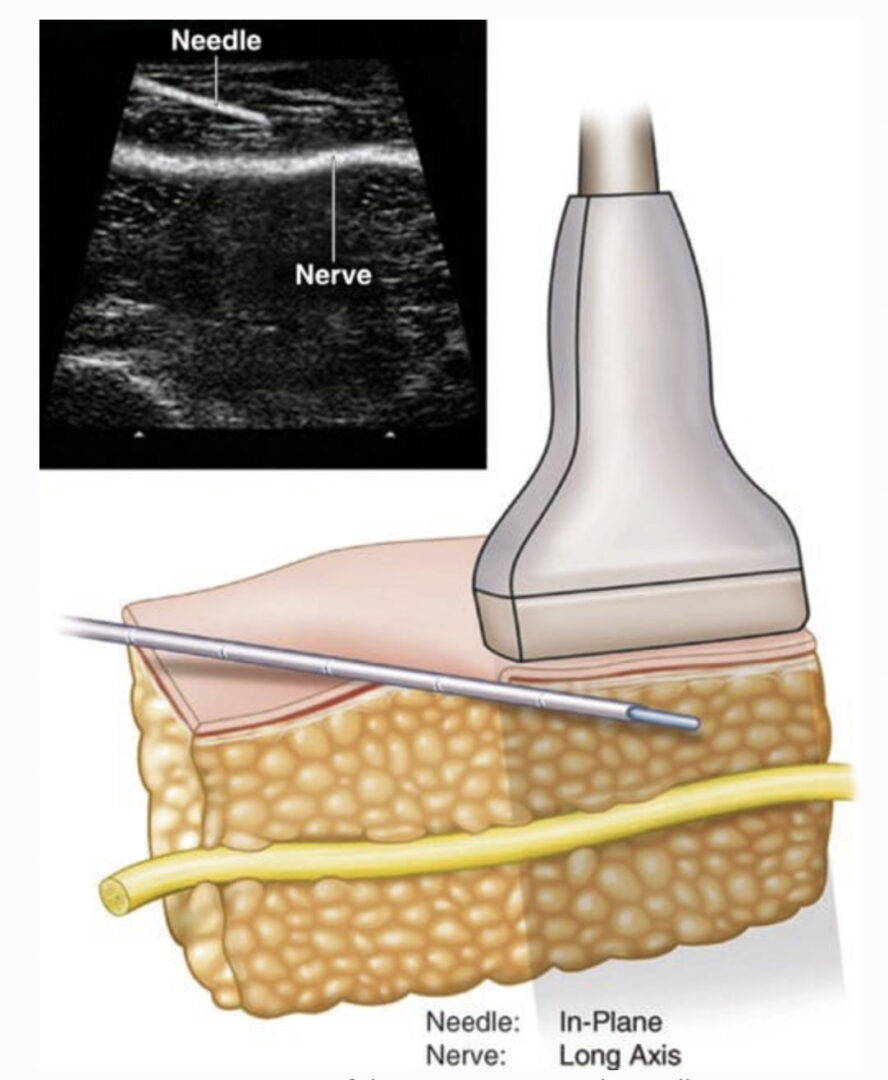
Nerve in Short Axis: Needle In-Plane Approach
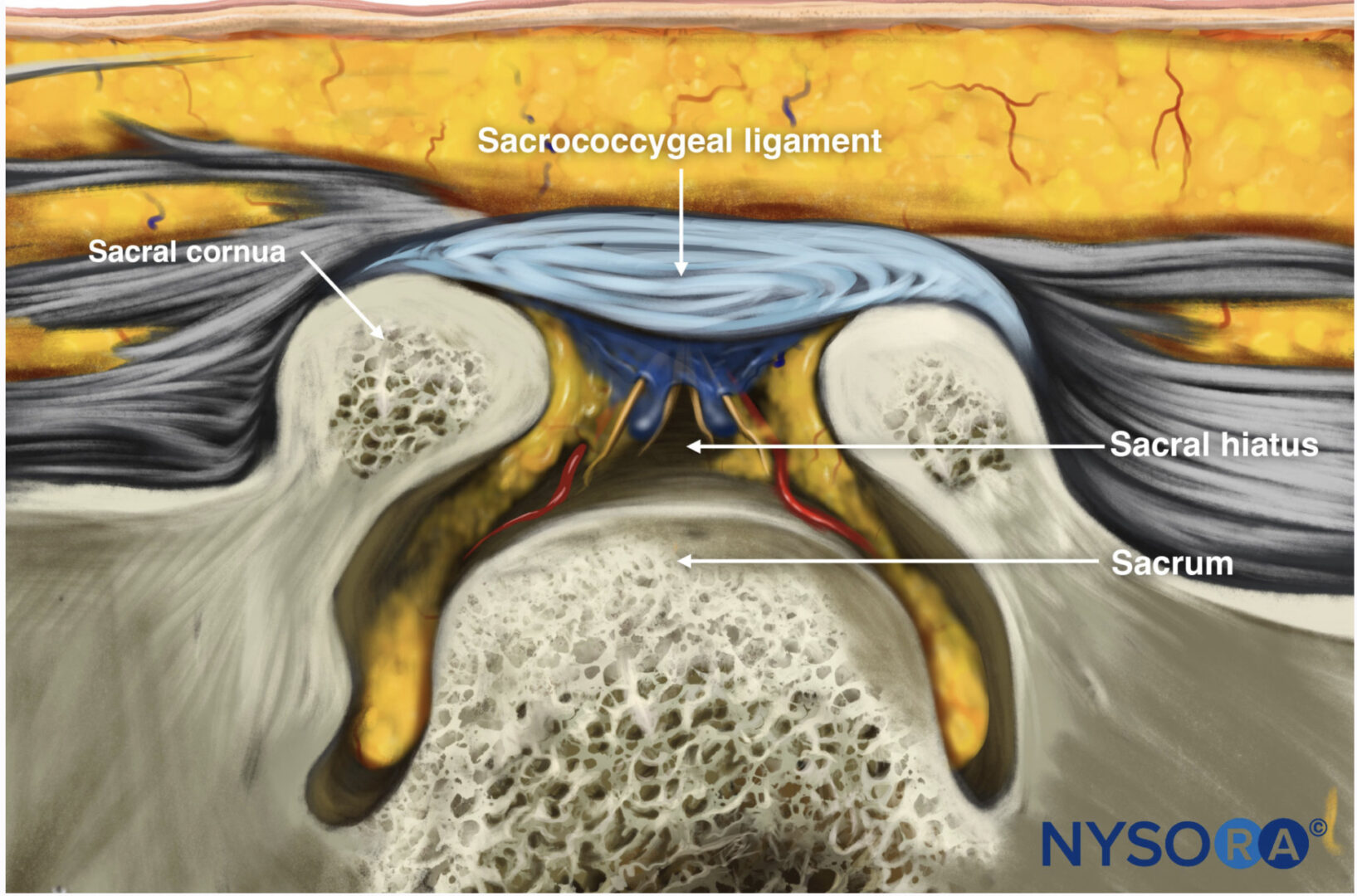
The short-axis imaging (cross-sectional imaging) of target nerves permits differentiation of neural tissue from surrounding anatomic structures such as muscle and adipose [34]. Insertion of a 17- or 18-gauge Tuohy-tip needle and real-time guidance within the ultrasound beam (in-plane) allows the practitioner to visualize the entire length of the needle including the tip, thereby avoiding inadvertent intravascular or intraneural needle insertion during the CPNB procedure (Fig. 1) [33]. Fluid injected via the needle may be directed around the target nerve in a deliberate fashion prior to perineural catheter placement. A potential disadvantage of the inplane needle guidance technique with short-axis imaging is the needle orientation perpendicular to the path of the target nerve, which may result in catheters being inserted beyond the nerve and misplacement of the subsequent local anesthetic infusion [35]. The use of a flexible, epidural-type catheter may prevent catheter tip misplacement and may be more appropriate for in-plane ultrasound-guided CPNB techniques utilizing short-axis imaging [17, 19, 21].
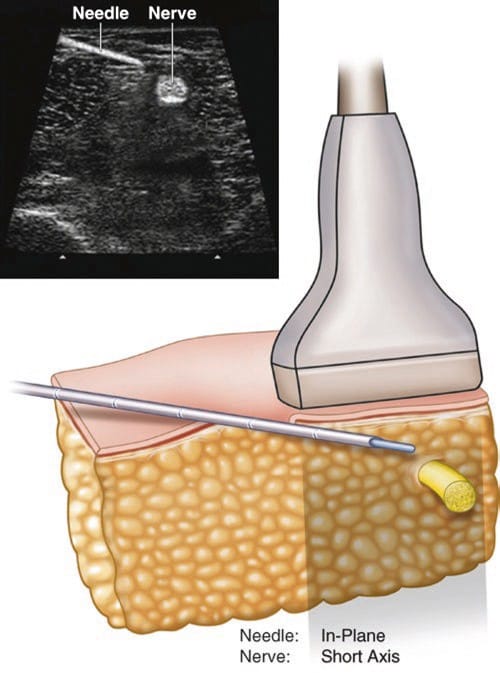
Fig.1 Short-axis imaging of the target nerve with needle advancement under in-plane ultrasound guidance
Specific challenges in adopting the in-plane needle guidance approach include acceptance of “new” needle insertion sites that differ from traditional nerve stimulation techniques [19, 21] and technical difficulty in visualizing the needle tip throughout the CPNB procedure.
3. NERVE IN SHORT AXIS: NEEDLE OUT-OF-PLANE APPROACH
In this approach, the target nerve is visualized in short axis, but the placement needle is inserted in approximately the same predicted sites recommended by nerve stimulation techniques, only aided by ultrasound-guided nerve localization (Fig. 2). Because the needle passes through the plane of the ultrasound beam, needle tip identification can be difficult or impossible [34, 36]. Practitioners have recommended the use of local tissue movement and intermittent injection of fluid via the placement needle to infer the position of the needle tip during advancement [22, 36]. Once the placement needle is in proximity to the target nerve, the possible advantage of this technique over the in-plane approach is the potential to advance the perineural catheter nearly parallel to the path of the nerve. Additionally, the needle insertion sites involved are more familiar to practitioners who practice stimulation-guided regional anesthesia.
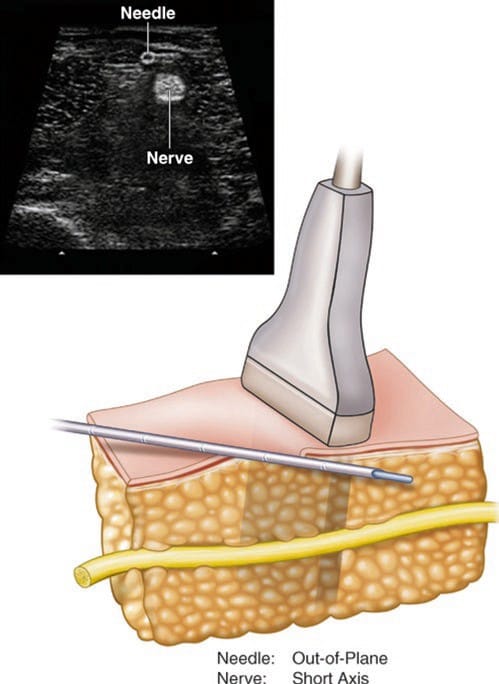
Fig.2 Short-axis imaging of the target nerve with the needle advancement under out-of-plane ultrasound guidance
4. NERVE IN LONG AXIS: NEEDLE IN-PLANE
In theory, visualizing the target nerve in the long axis while using in-plane guidance of the needle and perineural catheter should be the optimal approach (Fig. 3). Unfortunately, imaging these structures within the same plane is challenging, to say the least, and is limited to specific circumstances [27, 37]. Anatomically, few nerves maintain a trajectory that is straight enough to permit long-axis imaging [27, 38], and though this technique may potentially place the catheter tip in closer proximity to the target nerve, the time required to perform this technique is longer than required by the short-axis in-plane technique, without any clinical advantages when using standard perineural infusion regimens [37]. To date, this approach has not been validated in randomized clinical trials for brachial plexus perineural catheter insertion.
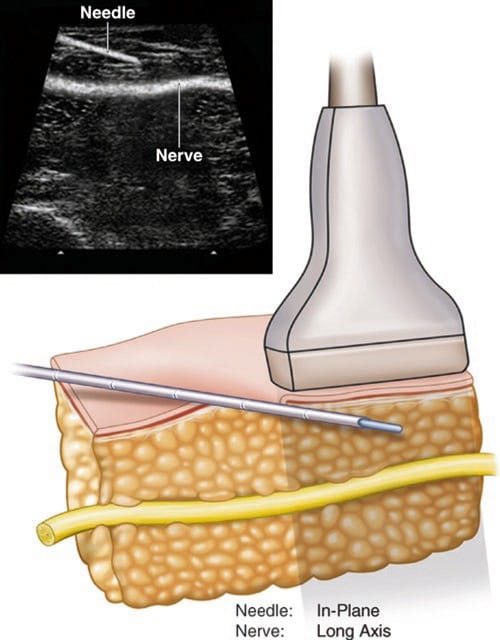
Fig.3 Long-axis imaging of the target nerve with needle advancement under in-plane ultrasound guidance
5. PREPARATION FOR ULTRASOUND-GUIDED PERINEURAL CATHETER INSERTION
Sterile Technique
Prior to perineural catheter insertion, the planned procedural site should be shaved, if necessary, to accommodate catheter dressings. For all perineural catheter insertion procedures, sterile technique is recommended [39]. Included are skin preparation with chlorhexidine gluconate solution; a sterile fenestrated surgical drape; sterile equipment, including a protective ultrasound transducer sleeve and conductive gel; sterile gloves; and surgical cap and mask.
6. STANDARD PERINEURAL CATHETER EQUIPMENT
Various needle and perineural catheter equipment sets have been presented. For practitioners employing short-axis imaging and in-plane needle guidance technique, the nonstimulating, flexible epidural-type catheter and Tuohy-tip placement needle are preferred [17, 19–21]. Stimulating perineural catheters may also be used with ultrasound guidance [18, 23, 25, 28, 35].
Many other nonstimulating catheter and placement needle combinations have been employed for ultrasound-guided perineural catheter techniques [22, 36, 40]. The number of catheter orifices may have clinical effects depending on the catheter insertion technique and perineural infusion regimen [41], but these effects have not been rigorously studied to date. An electrical nerve stimulator will also be required if using a combined technique of ultrasound guidance and electrical stimulation. Local anesthetic (e.g., 1% lidocaine) should also be included within the perineural catheter set for skin infiltration and injection within the subcutaneous and muscular tissues that comprise the trajectory of the placement needle.
7. ULTRASOUND-GUIDED PERINEURAL CATHETER INSERTION TECHNIQUES FOR COMMON SURGICAL PROCEDURES
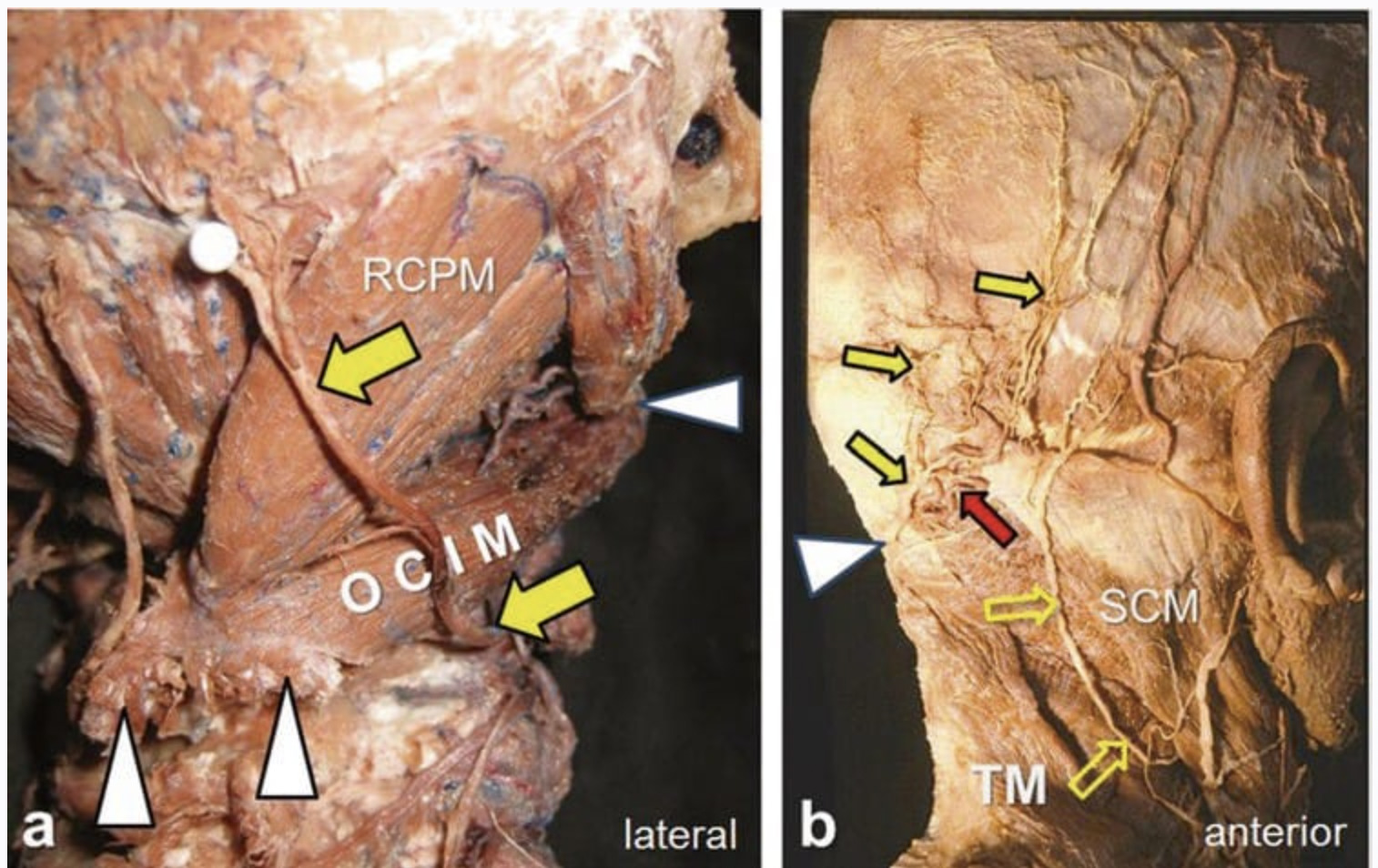
Interscalene CPNB
Indications: Shoulder or proximal humerus surgery
Transducer Selection: High-frequency, linear
Preparation and Equipment: As above
Patient Positioning: Supine, with the head turned away from the affected side [42], or lateral decubitus with the affected side nondependent [18, 25]
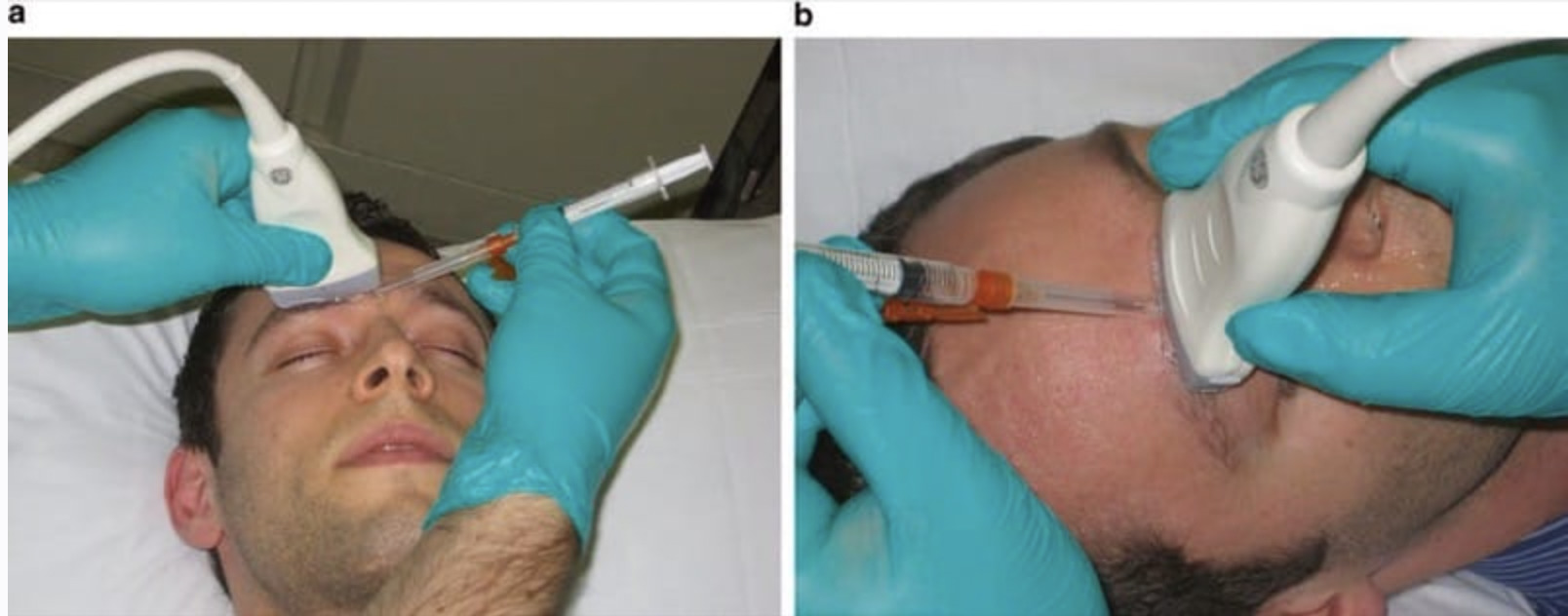
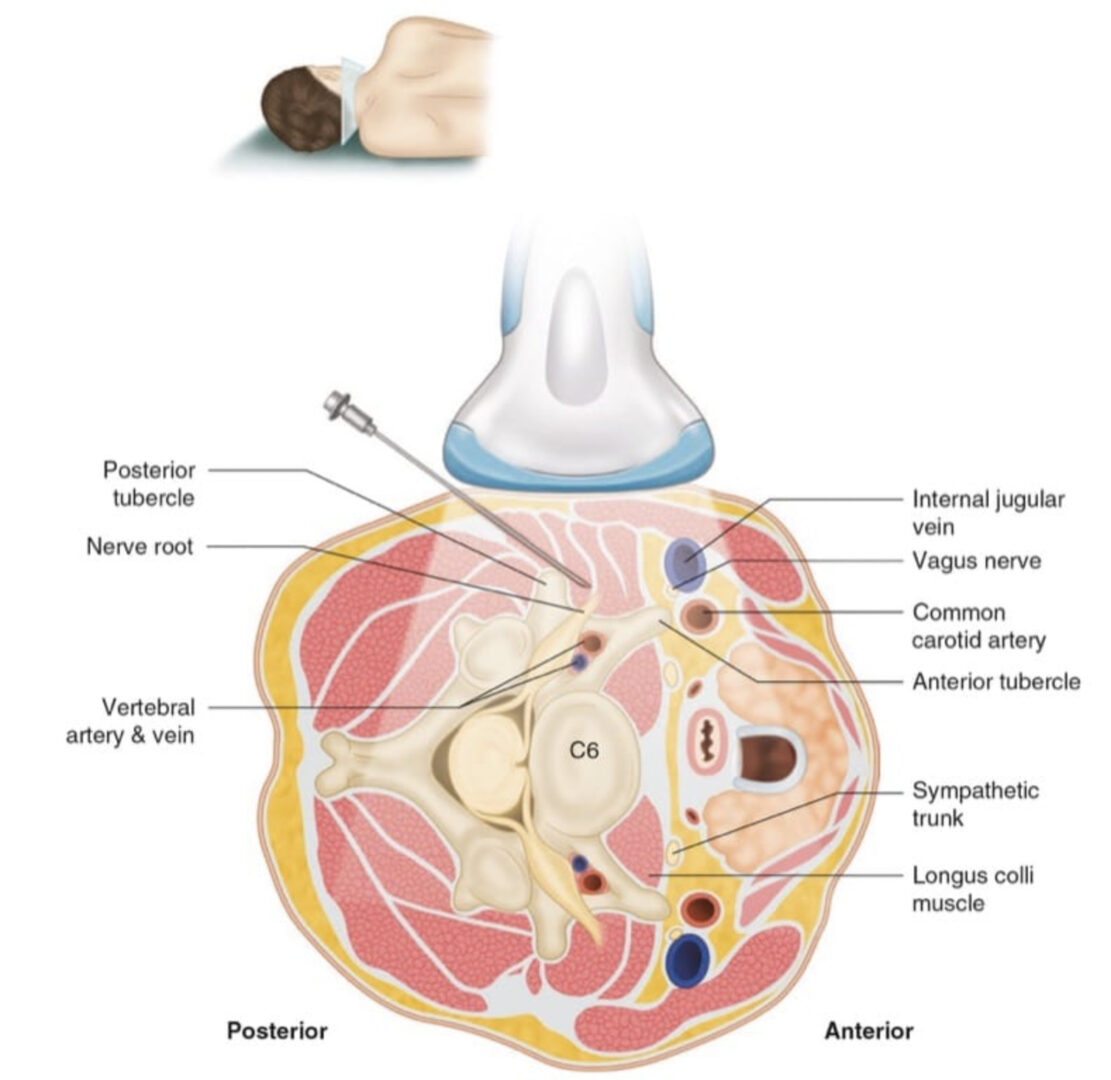
Technique: The ultrasound transducer should be placed at the level of the cricoid cartilage perpendicular to the skin, with the anterior portion of the transducer over the clavicular head of the sternocleidomastoid (SCM) muscle (Fig. 4a). After identifying the brachial plexus between the anterior and middle scalene muscles (Fig. 4b), insert the placement needle in either a cephalad-to-caudad direction out-of-plane [36, 43] or in a posterior-to-anterior direction in-plane [18, 24, 25], and advance the needle until the tip is in proximity to the target nerve. Injectate solution (local anesthetic, saline, or dextrose-containing water) via the placement needle facilitates subsequent perineural catheter insertion. Catheter tip position may be inferred using electrical stimulation [25], agitated injectate [44], or air injected via the catheter [45].
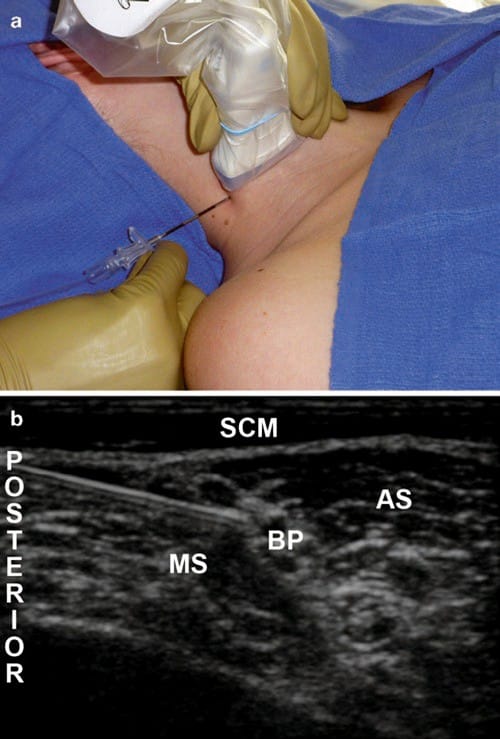
Fig.4 (a) Demonstration of ultrasound transducer position and needle insertion site for the right interscalene brachial plexus perineural catheter insertion. The patient is positioned supine with the head turned away from the side to be blocked. (b) Sample image from ultrasound- guided interscalene brachial plexus perineural catheter insertion. AS anterior scalene muscle, B brachial plexus, MS middle scalene muscle, SCM sternocleidomastoid muscle
Pearls: Identify the SCM over the internal jugular vein, and follow the deep fascia of the SCM posteriorly. The adjacent group of muscles posterior and deep to the SCM are the scalene muscles. If the plane between the anterior and middle scalene muscles is not apparent, slide the transducer caudad until the separation of the two muscles can be visualized.
When advancing the placement needle through the middle scalene muscle using an in-plane technique, direct the tip of the needle toward hyperechoic connective tissue or perineural fat, rather than toward the hypoechoic neural structures, to avoid inducing paresthesias.
8. INFRACLAVICULAR CPNB
Indications: Distal humerus, elbow, forearm, and hand surgery
Transducer Selection: Low-frequency, small curvilinear (preferred) or high-frequency, linear
Preparation and Equipment: As above
Patient Positioning: Supine, with the affected arm abducted, if feasible, and the head turned away from the side to be blocked [17, 20]
Technique: The ultrasound transducer is applied medial and caudad to the ipsilateral coracoid process and oriented in a parasagittal plane (Fig. 5a). After identifying the brachial plexus cords around the axillary artery in a short-axis image (Fig. 5b), the placement needle is directed cephalad-to-caudad in-plane to permit needle tip visualization and avoid inadvertent vascular puncture [17, 20]. Injectate solution can be distributed via the placement needle around each of the three cords separately [17] or as a single deposit posterior to the axillary artery [46] prior to perineural catheter insertion. A nonstimulating, flexible epidural-type catheter [17, 20] or stimulating catheter [23] should be placed posterior to the axillary artery.
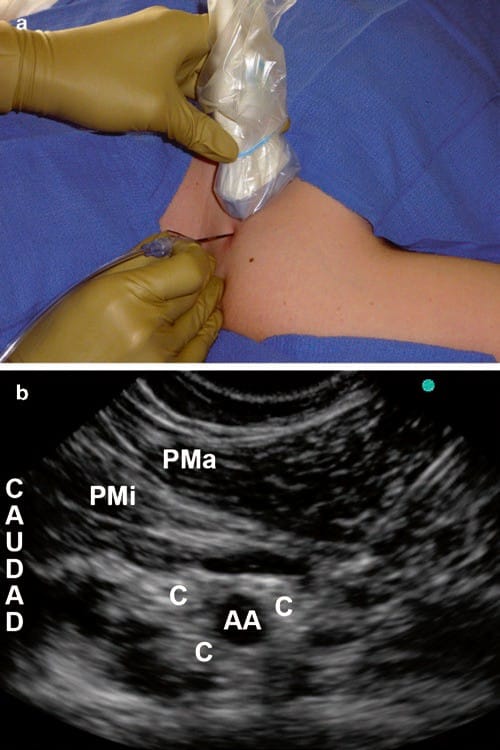
Fig.5 (a) Demonstration of ultrasound transducer position and needle insertion site for the right infraclavicular brachial plexus peri-neural catheter insertion. The patient is positioned supine with the head turned away from the side to be blocked and the right arm abducted. (b) Sample image from ultrasound-guided infraclavicular brachial plexus perineural catheter insertion. AA axillary artery, C cord of the brachial plexus, PMa pectoralis major muscle, PMi pectoralis minor muscle
Pearls: Although the infraclavicular CPNB can be placed with the arm in any position, abducting the arm at the shoulder facilitates cross-sectional imaging of the brachial plexus and vasculature and reduces the depth of these structures by stretching the pectoralis muscles and moving them further away from the chest wall. Based on a study demonstrating equal efficacy for single-injection and triple-injection techniques for infraclavicular CPNB [46], a single injection posterior to the axillary artery with subsequent perineural catheter insertion is recommended for procedures performed solely for postoperative pain. For perineural infusion settings, consider a higher basal rate of dilute local anesthetic solution (e.g., 0.2% ropivacaine) to maximize analgesia and minimize the incidence of an insensate extremity [47]. When used for similar surgical indications (distal upper extremity surgery), infraclavicular CPNB provides more effective analgesia than supraclavicular perineural catheters, when ultrasound guidance is used for both techniques [48]
9. FEMORAL CPNB
Indications: Thigh and knee surgery
Transducer Selection: High-frequency, linear Preparation and Equipment: As above
Patient Positioning: Supine, with the affected leg straight
Technique: The ultrasound transducer should be applied perpendicular to the skin at the level of the inguinal crease, oriented parallel to the inguinal ligament and immediately lateral to the femoral artery pulse (Fig. 6a). After identifying the femoral nerve below the fascia iliaca lateral to the femoral artery (Fig. 6b), the placement needle may be inserted and directed cephalad-to-caudad out-of-plane [22, 26], lateral-to-medial in-plane [21], or cephalad-to-caudad inplane [27] until the tip is in proximity to the femoral nerve and injectate solution can be deposited around the nerve via the needle. A perineural catheter can then be inserted through the placement needle, either anterior or posterior to the nerve; both catheter positions produce an equal degree of motor block in volunteers [49].
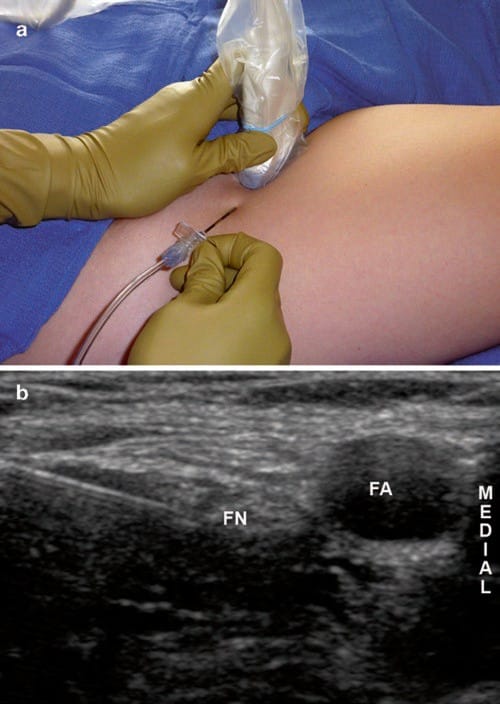
Fig.6 (a) Demonstration of ultrasound transducer position and needle insertion site for the right femoral perineural catheter insertion. The patient is positioned supine with the affected leg straight. (b) Sample image from ultrasound-guided femoral perineural catheter insertion; FA femoral artery, FN femoral nerve
Pearls: Utilize color Doppler to aid in the identification of the femoral artery. If the profunda femoris artery is visualized, follow this branch cephalad until it joins the femoral artery. The femoral nerve will typically be at the same depth as the femoral artery. Identify the curved fascia iliaca over the iliacus muscle from lateral to medial. The femoral nerve is located where the fascia iliaca separates off of the iliacus muscle medially. To avoid inadvertently traumatizing the nerve, consider using a hydrodissection technique after piercing the fascia iliaca. Perineural catheters placed for knee surgery should be positioned along the lateral aspect of the femoral nerve on the anterior or posterior side [49, 50]; low-dose infusions should be used for ambulatory patients, to minimize quadriceps weakness [7, 51].
10. SUBGLUTEAL SCIATIC CPNB
Indications: Foot and ankle surgery
Transducer Selection: High-frequency linear or large, lowfrequency curvilinear (preferred)
Preparation and Equipment: As above
Patient Positioning: Semi-prone (Sims position) with the knee on the affected side flexed and crossed over the dependent, unaffected leg
Technique: Apply the ultrasound transducer in axial orientation perpendicular to the skin between the ischial tuberosity and the greater trochanter of the femur (Fig. 7a) [52, 53]. Identify the sciatic nerve medial to the femur and deep to the fascia of the gluteus maximus muscle (Fig. 7b) [52]. Insert the placement needle in a lateral-to-medial direction with inplane guidance or in a caudad-to-cephalad direction with out-of-plane guidance [28]. When the needle tip is in proximity to the sciatic nerve, injectate solution is administered via the placement needle. Following confirmation of circumferential injectate spread around the sciatic nerve, the flexible epiduraltype catheter or styleted stimulating perineural catheter [28] can be inserted through the placement needle.
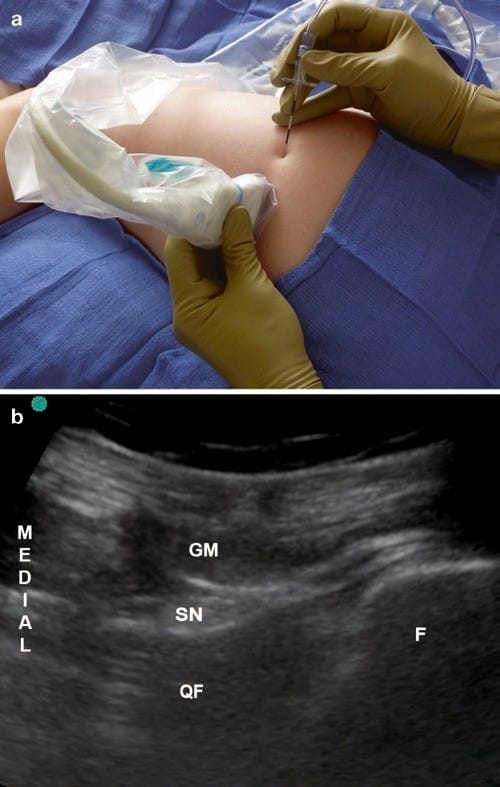
Fig.7 (a) Demonstration of ultrasound transducer position and needle insertion site for left subgluteal sciatic perineural catheter insertion. The patient is in Sims position with the right side dependent. (b) Sample image from ultrasound-guided subgluteal sciatic perineural catheter insertion. F femur, GM gluteus maximus muscle, QF quadratus femoris muscle, SN sciatic nerve
Pearls: The subgluteal approach can also be performed in the prone position, although the Sims position offers the advantage of stretching the gluteus muscles and reducing the depth from skin to target nerve. The sciatic nerve is reliably located between the femur and the ischial tuberosity. When subgluteal sciatic perineural catheters are used for postoperative analgesia in a basal-bolus infusion regimen, local anesthetic consumption can be expected to be lower than with popliteal catheter infusions for similar surgical indications [54].
11. POPLITEAL SCIATIC CPNB
Indications: Foot and ankle surgery
Transducer Selection: High-frequency linear (preferred) or low-frequency curvilinear (obese patients)
Preparation and Equipment: As above
Patient Positioning: Prone with the ankle of the affected side supported by a pillow or towel
Technique: Apply the ultrasound transducer in axial orientation perpendicular to the skin at the level of the intertendinous junction (Fig. 8a) [55]. After identifying the sciatic nerve anterior and medial to the fascia of the biceps femoris muscle (Fig. 8b), the placement needle may be inserted in a cephalad-to-caudad direction out-of-plane [22] or lateral-tomedial with in-plane guidance [19]. When the needle tip is in proximity to the sciatic nerve, injectate solution is administered via the placement needle. Following confirmation of circumferential injectate spread around the sciatic nerve, the flexible [19] or standard [22] epidural-type perineural catheter is deployed through the placement needle.
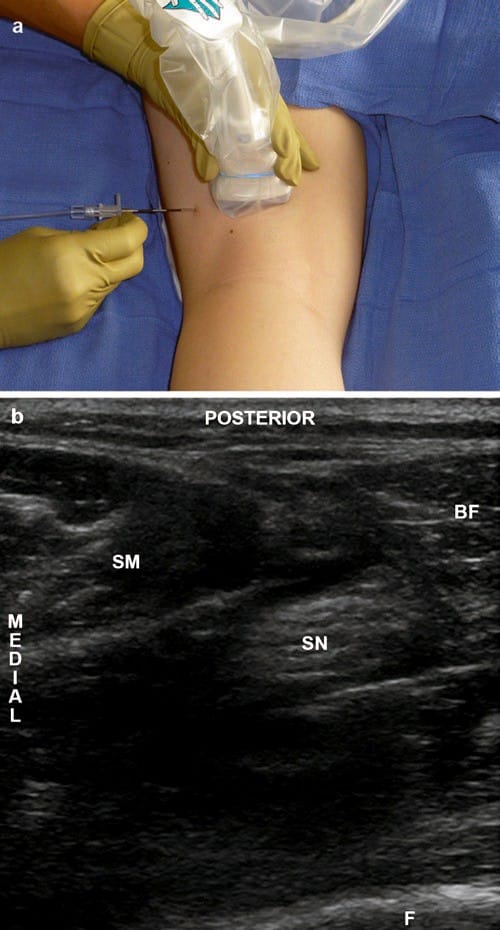
Fig.8 (a) Demonstration of ultrasound transducer position and needle insertion site for the left popliteal sciatic perineural catheter insertion. The patient is positioned prone with the affected extremity slightly flexed at the knee. (b) Sample image from ultrasound-guided popliteal sciatic perineural catheter insertion. BF biceps femoris muscle, F femur, SM semimembranosus muscle, SN sciatic nerve
Pearls: The use of ultrasound guidance also facilitates the performance of popliteal sciatic CPNB in the supine and lateral positions. When searching for the nerve, first identify the surface of the femur, which serves as a lateral landmark and depth limit; the sciatic nerve will always be medial and posterior to the femur. Follow the biceps femoris muscle and investing fascia posteriorly and medially from the femur. The sciatic nerve is reliably located medial to the fascia of the biceps femoris muscle. For postoperative perineural infusion, avoid high basal rates of dilute local anesthetic, to minimize the likelihood of an insensate extremity [56].
12. TRANSVERSUS ABDOMINIS PLANE (TAP) CPNB
Indications: Abdominal wall surgery (e.g., inguinal and ventral hernia repairs or laparotomy)
Transducer Selection: High-frequency, linear or lowfrequency, curvilinear (obese patients)
Preparation and Equipment: As above
Patient Positioning: Supine or lateral decubitus with the affected side up
Technique: Apply the ultrasound transducer in axial orientation perpendicular to the skin at approximately the midaxillary line between the costal margin and the iliac crest (Fig. 9a). After identifying the three layers of the abdominal wall (external oblique, internal oblique, and transversus abdominis muscles), direct the needle anterior-to-posterior [30] or posterior-to-anterior until the needle tip enters the plane between the internal oblique and transversus abdominis muscles (Fig. 9b). Approximately 20 mL of local anesthetic solution injected via the placement needle will produce reliable anesthesia of the ipsilateral T10 to L1 dermatomes [57, 58]. For postoperative local anesthetic infusion, a flexible, epidural-type catheter can be placed into the transversus abdominis plane (TAP) through the placement needle, with midline incisions requiring bilateral TAP catheters [30]. The subcostal TAP can be visualized by placing the ultrasound transducer along the medial costal margin; catheters inserted at this level can provide analgesia in the T7 to T9 dermatomal distribution [32].
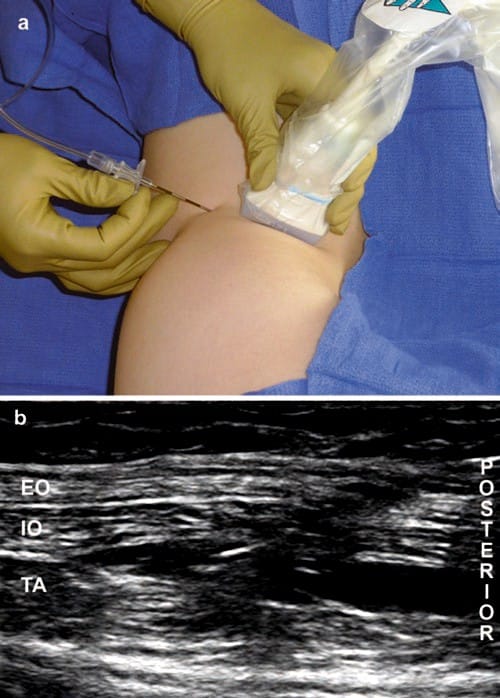
Fig.9 (a) Demonstration of ultrasound transducer position and needle insertion site for the right transversus abdominis plane (TAP) perineural catheter insertion. The patient is positioned left lateral decubitus. (b) Sample image from ultrasound-guided TAP perineural cath-eter insertion. EO external oblique muscle, IO internal oblique muscle, TA transversus abdominis muscle
Pearls: The use of bilateral TAP catheters is not a replacement for epidural analgesia, but for patients in whom epidural analgesia is not indicated, TAP blocks have demonstrated efficacy in reducing postoperative pain following various abdominal and pelvic procedures [59–62]. Insertion of the TAP catheter from the posterior approach offers the advantage of further displacement away from the surgical field, therefore permitting preoperative placement. The optimal infusion regimen for TAP catheters has not yet been determined.
13. CONCLUSIONS
Ultrasound-guided continuous peripheral nerve blocks (CPNB) and subsequent perineural local anesthetic infusions offer superior pain relief for a variety of surgical indications. The application of ultrasound guidance has improved the success rate and efficiency of CPNB procedures [19–21], but the effect, if any, on the optimal perineural infusion rates and drug dosage remains unknown. Further research is required to explore various catheter designs (e.g., stimulating versus nonstimulating, single-orifice versus multi-orifice), placement needles, ultrasound transducers and machines, infusion regimens for specific ultrasound-guided perineural catheter locations, and application of emerging technology.