The ganglion impar is a solitary neural structure located anterior to the sacrococcygeal joint (SCJ). It represents the fusion of the caudal end of the bilateral sympathetic chains. The ganglion impar innervates the perineum, distal rectum, anal canal, distal urethra, scrotum, distal third of the vagina, and the vulva [1, 2].
1. INDICATIONS
The ganglion impar (ganglion of Walther or sacrococcygeal ganglion) block is used in the diagnosis and management of visceral or sympathetic-maintained pain in the perineal and coccygeal areas. Ganglion impar neurolysis has been reported for the palliative treatment for malignant pain [1, 3].
2. LIMITATIONS OF THE CURRENT TECHNIQUE
Multiple approaches have been described for ganglion impar block. The most widely used approach is the trans- sacrococcygeal approach with fluoroscopy by introducing the needle through the SCJ [4, 5]. Impacted stool or gas in the rectum can easily obscure the SCJ in the anteroposterior fluoroscopy view. Also, a calcified sacrococcygeal disk will make it difficult to identify the SCJ even in the lateral fluoroscopy view. With fluoroscopy, the needle may get stuck in the SCJ; however, under ultrasound (US) guidance, we can easily penetrate the SCJ by changing the needle’s direction to match the angulation of the SCJ [6].
3. LITERATURE REVIEW ON ULTRASOUND-GUIDED GANGLION IMPAR BLOCK
The classic transanococcygeal approach (curved needle placed through the anococcygeal ligament) was described with ultrasound (US) guidance [7]. However, the authors prefer the trans-sacrococcygeal approach because it is more comfortable for the patient and it may avoid anal or rectal injuries.
Lin and coworkers [6] reported the safety of the US-guided trans-sacrococcygeal approach in 15 patients. The needle was accurately placed in all patients, as confirmed by fluoroscopy. They reported that US was advantageous over fluoroscopy because the SCJ was easily identified in all 15 patients, whereas it was difficult to visualize in 5 patients with fluoroscopy alone because it was obscured by rectal gas, impacted stool, or ossified sacrococcygeal disks.
4. TECHNIQUE OF ULTRASOUND-GUIDED GANGLION IMPAR BLOCK
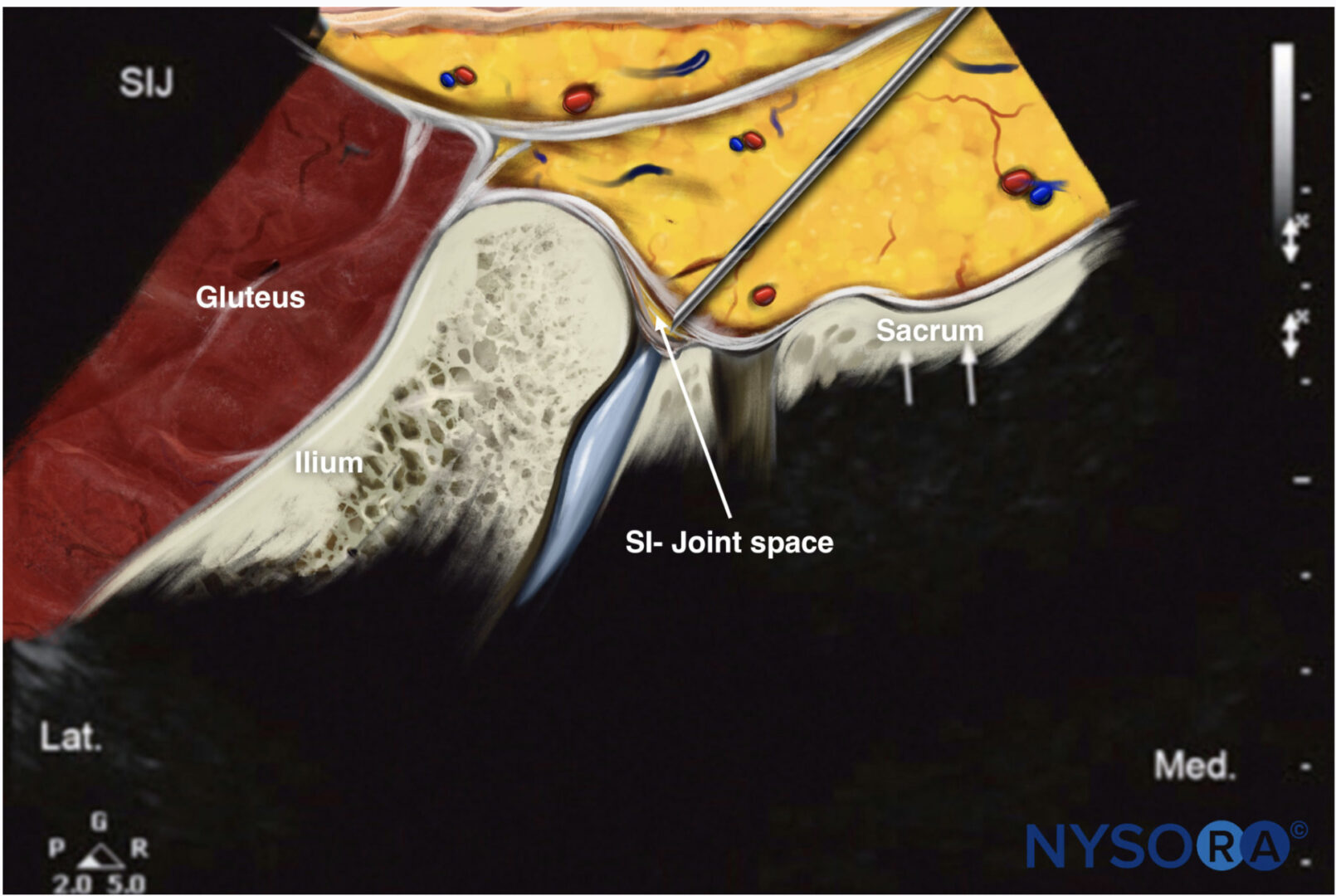
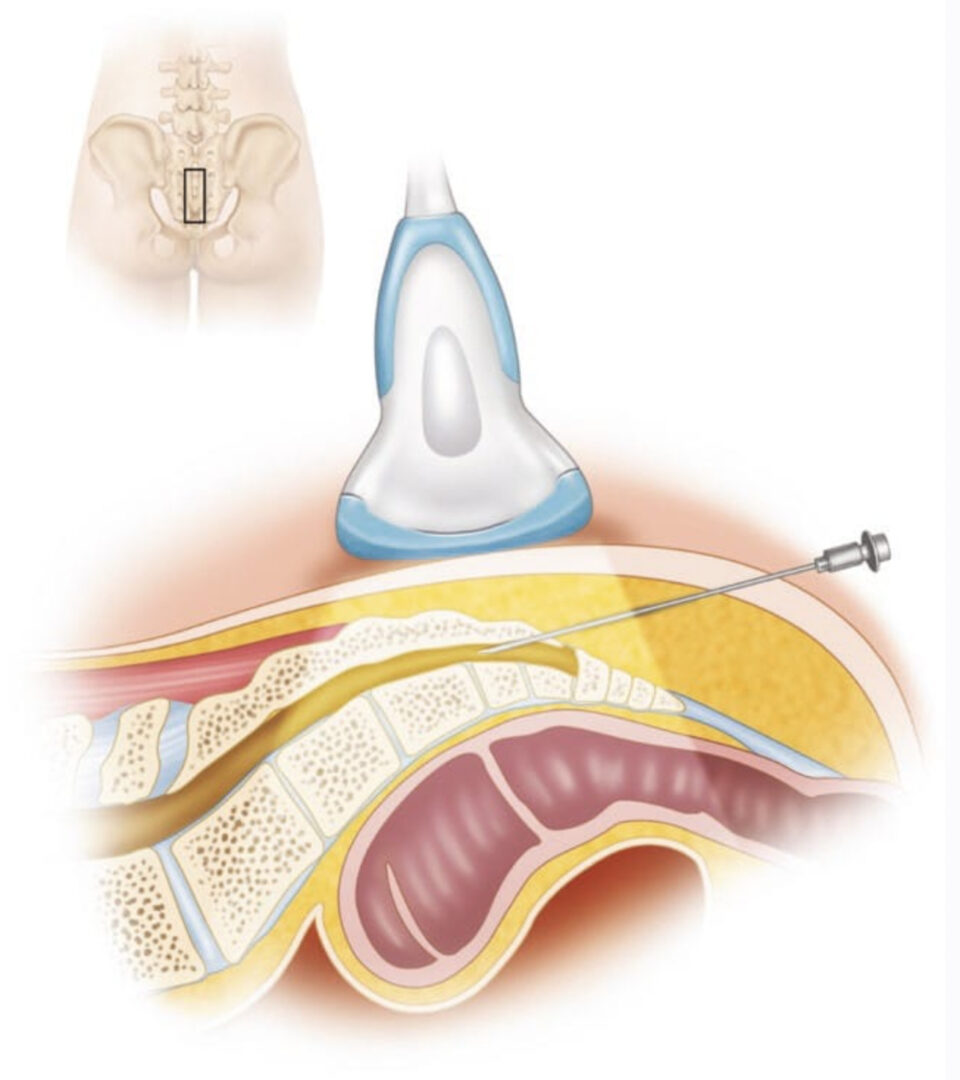
With the patient in the prone position, the sacral hiatus is palpated, and a linear high-frequency transducer (or curved low-frequency transducer in obese patients) is placed transversely in the midline to obtain a transverse view of the sacral hiatus as described in the course Caudal Block. The transducer is then rotated 90° to obtain a longitudinal view of the sacral hiatus and the coccyx (Fig. 1). The first cleft caudal to the sacral hiatus is the SCJ.
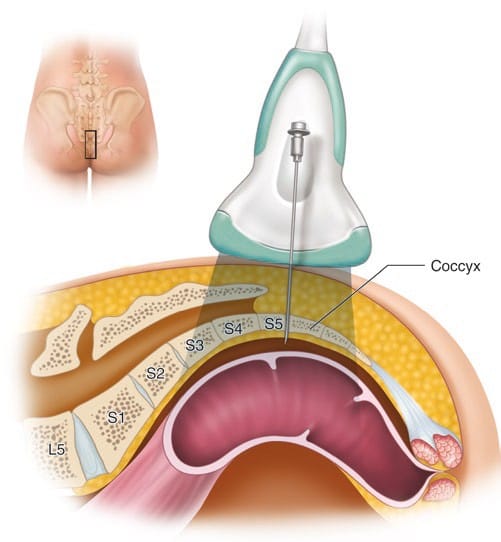
Fig. 1 The placement of the US probe over the SCJ to obtain a longitudinal scan is shown
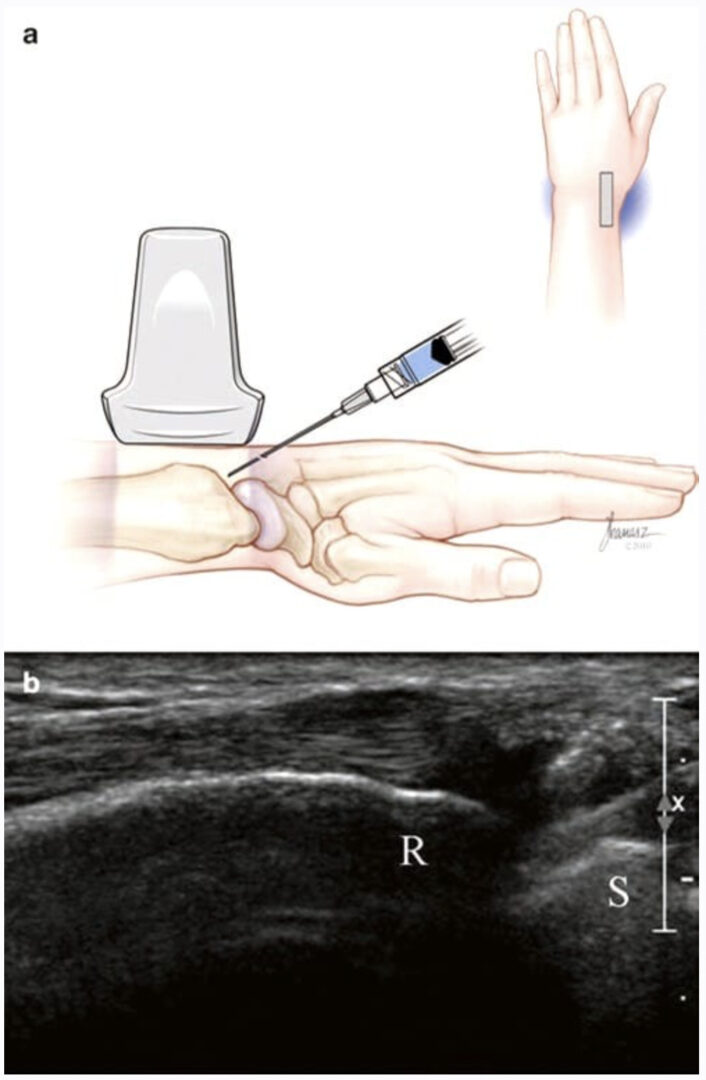
After local anesthesia infiltration of the skin and subcutaneous tissue, a 22- to 25-gauge needle is advanced into the SCJ under real-time ultrasonography. We use an out-of-plane approach while adjusting the needle’s path to match the angulation of the SCJ cleft to allow for a traumatic needle insertion (Fig. 2). The needle is advanced slightly through the SCJ cleft, and usually, loss of resistance is felt, indicating placement of the needle tip anterior to the ventral sacrococcygeal ligament. Lateral fluoroscopy may be obtained to confirm the depth of the needle and to monitor the spread of the injectate.
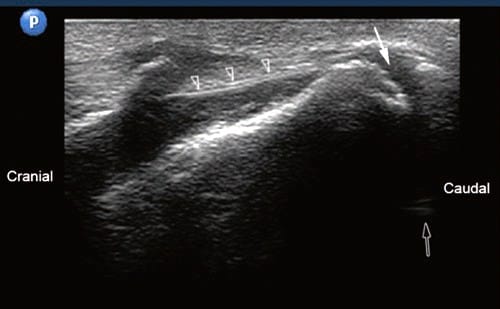
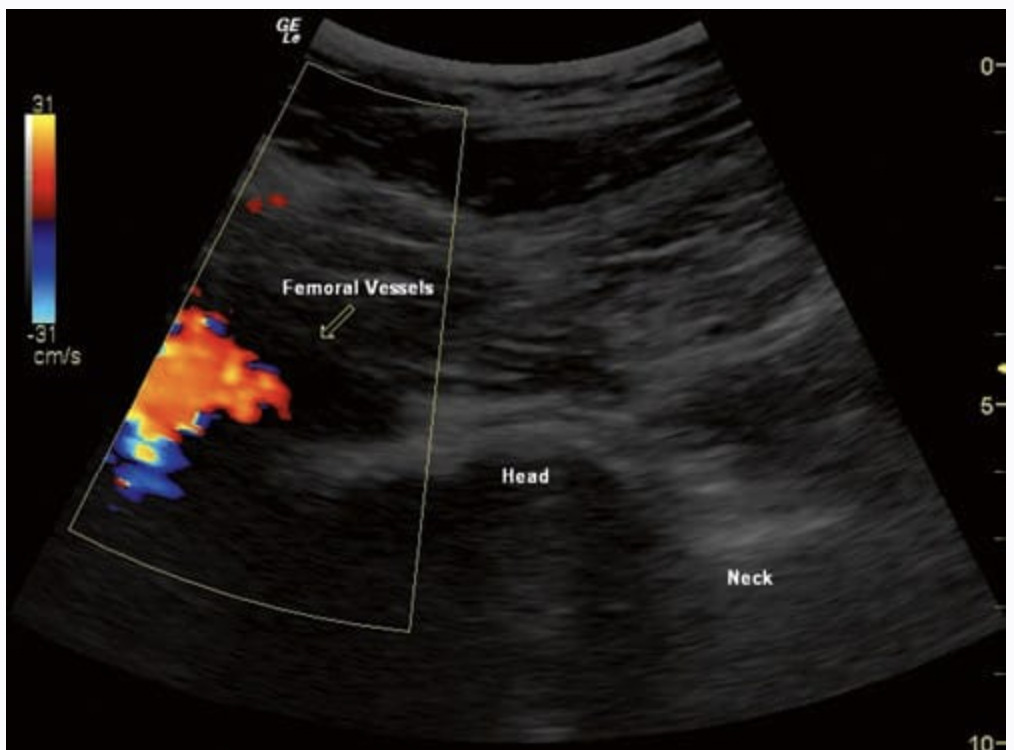
Fig. 2 Long-axis sonogram showing the SCJ (solid arrow) and the sacrococcygeal ligament (arrowheads). Notice that the rectum (hollow arrow) can be insonated through the sacrococcygeal cleft (Reprinted with permission from Ohio Pain and Headache Institute)
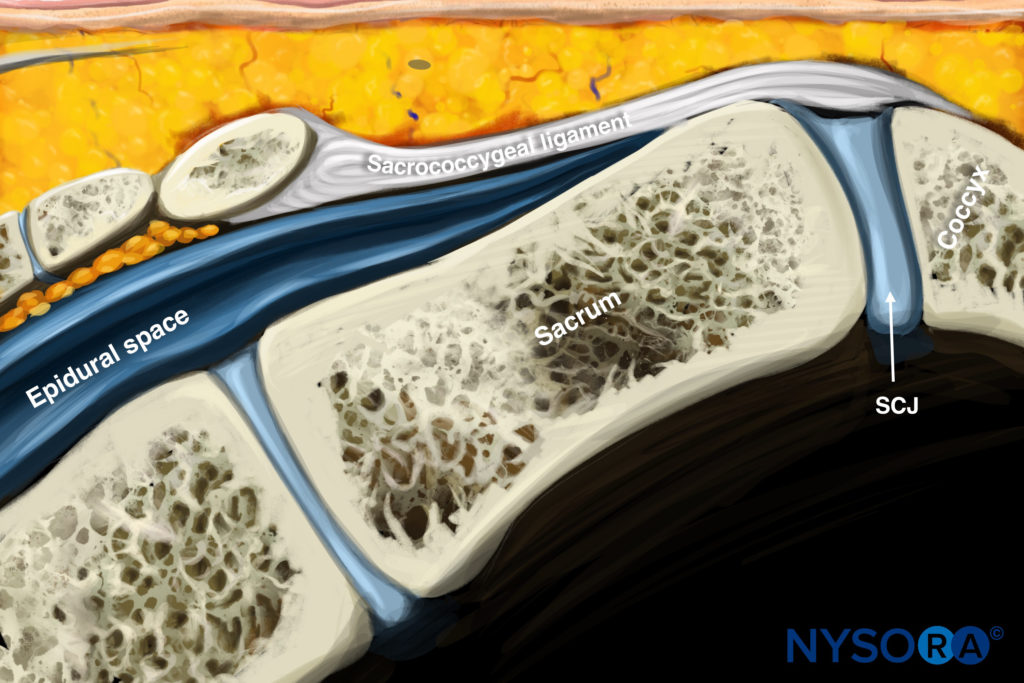
Reverse Ultrasound Anatomy illustration of figure 2. SCJ, sacrococcygeal joint.
5. LIMITATIONS OF THE ULTRASOUND-GUIDED TECHNIQUE
US cannot accurately monitor the needle depth or the spread of the injectate because of the sacral and coccygeal bony artifacts. It can be helpful when fluoroscopy is not available or is insufficient to identify the SCJ. We recommend using a lateral fluoroscopic view to monitor the depth of the needle, especially with neurolytic injections [6].