Blocks of the greater occipital nerve (GON) have been performed without target visualization for a long time, based on surface landmarks only. An ultrasound (US)-guided technique was first introduced by our group in 2010 [1]. GON blocks are effective not only in the treatment of occipital neuralgia, which is a relatively rare pathology, but also for other types of headache and even facial pain. Studies confirm pain relief in migraine [2, 3], cervicogenic headache [4], cluster headache [5, 6], and even post-dural puncture headache [7] but show no improvement in chronic tension-type headache [8]. Additionally, they can have a positive effect in trigeminal neuralgia but show no benefit in persistent idiopathic facial pain [9]. Convergence of cervical and trigeminal input seems to be the explanation for this phenomenon, as experimental stimulation of the GON increases metabolic activity both in the trigeminal caudal nucleus and in the cervical dorsal horn [10]. Because of their wide field of indications, GON blocks are performed frequently by pain physicians.
1. ANATOMY AND TOPOGRAPHY OF THE GON AND ADJACENT STRUCTURES
The GON is the sensory branch of the posterior ramus of the C2 spinal nerve. Together with the lesser occipital nerve, the GON innervates the skin of the occipital region up to the vertex. After leaving the C2 spinal nerve posterior to the lateral atlantoaxial joint, it travels inferiorly and laterally to appear at the inferior border of the obliquus capitis inferior muscle (OCIM). Then, the GON ascends on the posterior surface of the OCIM and lies sandwiched between the OCIM and the semispinalis capitis muscle (SsCM), before piercing the latter. The GON terminates as a superficial nerve by either piercing the upper part of the trapezius muscle or running through the tendinous arch between the trapezius muscle and the sternocleidomastoid muscle, where it lies medial to the occipital artery (Fig. 1). This is the classic site for “blind” blocks, at the level of the superior nuchal line where the palpable artery serves as a landmark. Finally, the nerve divides into many branches, some of which connect to those of the lesser occipital nerve.
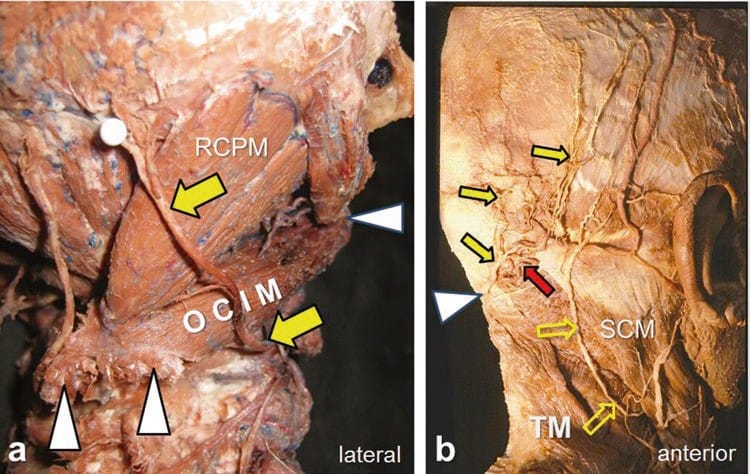
Fig.1 Topography of the greater occipital nerve (GON) (yellow arrows). (a) The specimen (right side, posterolateral view) shows the deep course of the GON prior to bifurcation; the semispinalis capitis muscle (SsCM) has been removed. The white pinhead indicates the level where the GON becomes superficial in the occipital region; this corresponds to the spot where it pierces the trapezius muscle. The white arrowheads indicate the right and left tubercles of the spinous process of the axis (medially) and the transverse process of the atlas (laterally). The obliquus capitis inferior muscle (OCIM) is the important deep muscular landmark for localizing the GON at the C2/C1 level because the GON is consistently found ascending on its dorsal surface. RCPM—rectus capitis posterior major muscle. (b) The superficial course of the GON and its relation to the lesser occipital nerve (open yellow arrows); note the anastomoses between them. The white arrowhead indicates the point where the GON pierces the trapezius muscle (TM); the nerve is seen medial to the occipital artery (red arrow). SCM sternocleidomas-toid muscle
Interestingly, Loukas et al. [11] found high variability of the GON’s distance to the midline (1.5–7.5 cm) at a horizontal level between the external occipital protuberance and the mastoid process in 100 cadavers. In contrast, the location of the GON as it curves around the OCIM is very constant. The OCIM is by far the thickest of the short muscles of the neck and spans from the spinous process (the right or left tubercle) of the axis medially to the transverse process of the atlas laterally (Fig. 2). The OCIM thus is the important deep muscular landmark for localizing and blocking the GON at the C2/C1 level under US guidance.
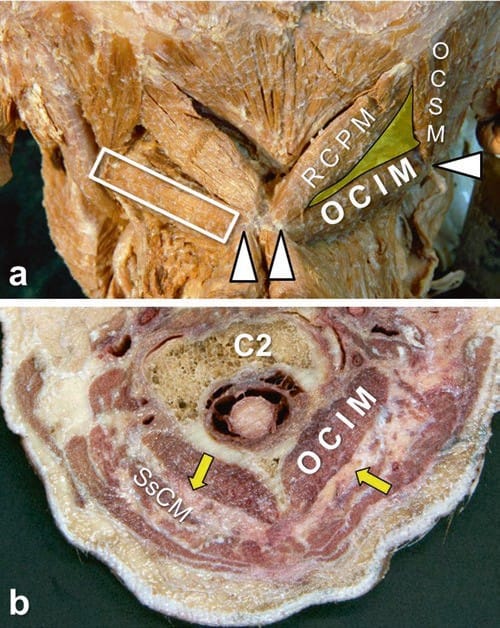
Fig.2 Short muscles of the neck, including the obliquus capitis inferior muscle (OCIM). (a) Posterior view of both suboccipital triangles (right one colored). The inferior border of the triangle is the promi-nent OCIM, which connects the spinous process of the axis with the transverse process of the atlas (white arrowheads). The remaining borders of the triangle are built by the rectus capitis posterior major muscle (RCPM) and the obliquus capitis superior muscle (OCSM); the white open rectangle indicates an accurate transducer position. (See also Fig.6.) (b) Cross section through the neck along both OCIMs (Cf. Fig.5); the GON (yellow arrows) lies sandwiched between the OCIM and the semispinalis capitis muscle (SsCM). C2 body of axis
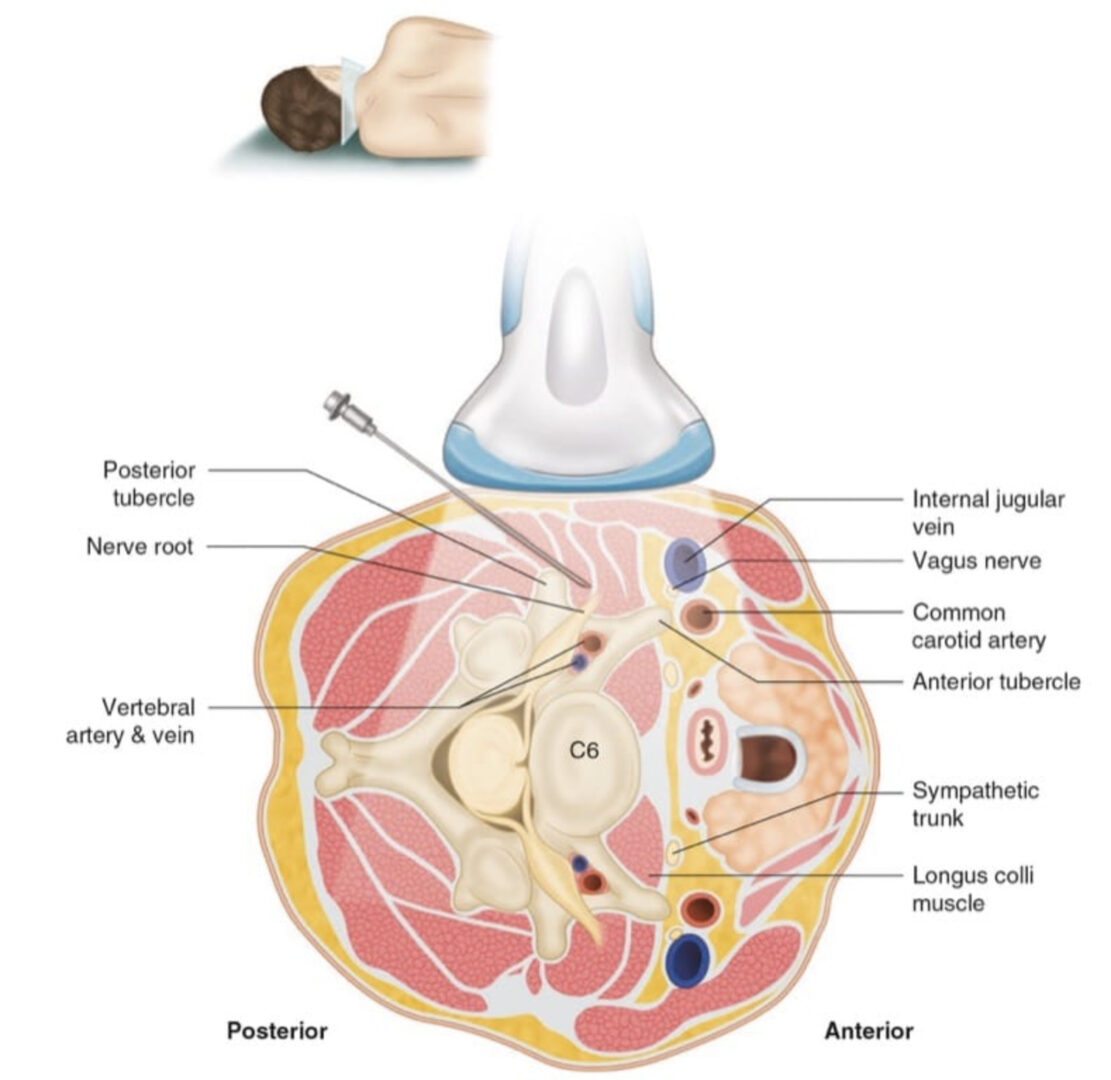
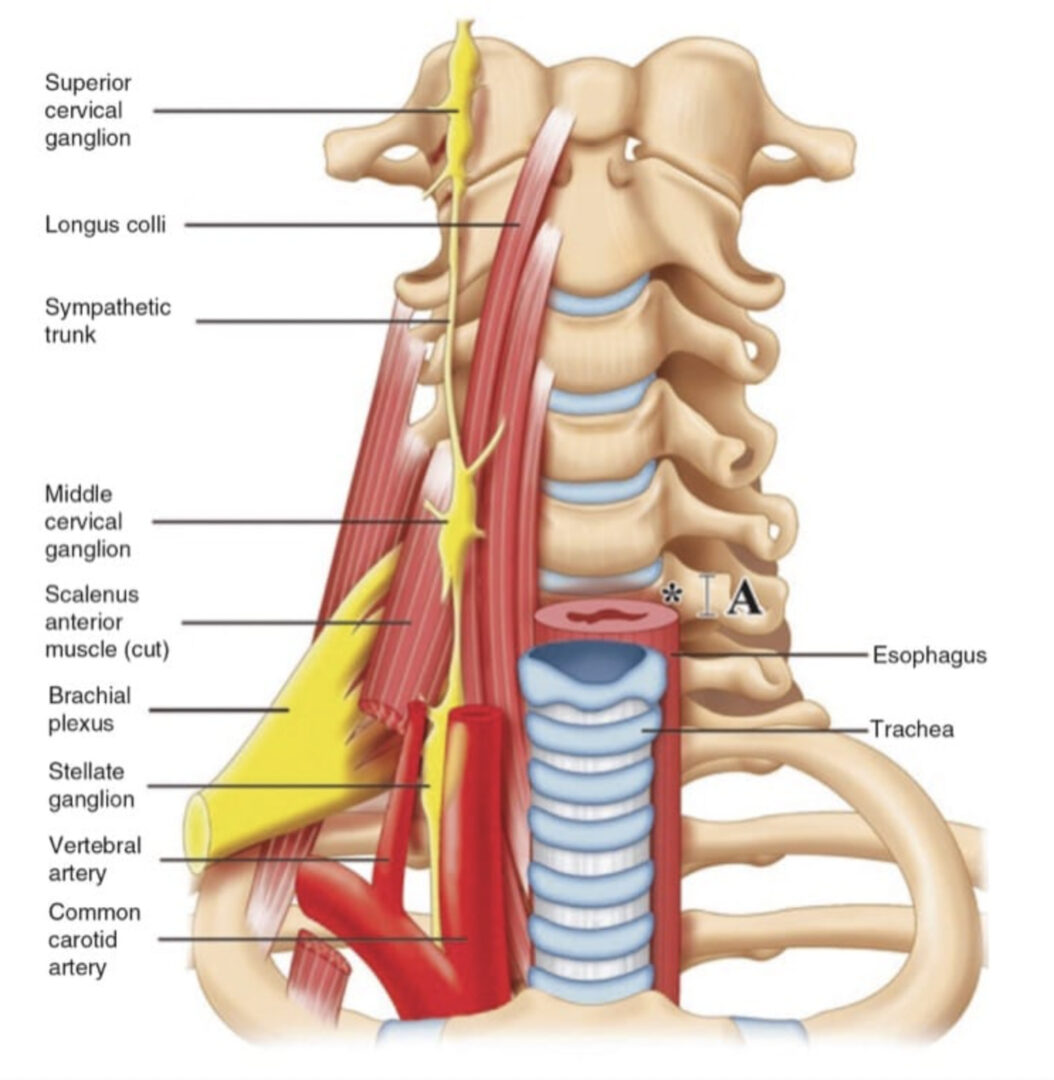
It is equally important to pay attention to the course and location of the vertebral artery (VA) when performing a GON block at the dorsal surface of the OCIM. Before entering the suboccipital triangle, the VA is located anterior to the OCIM and in close proximity to the transverse process of the atlas. Here, the VA is also significantly lateral to the GON. After ascending through the foramen transversarium of C1, the VA reaches the suboccipital triangle (Fig. 3), where it passes through a groove over the posterior arch of the atlas.
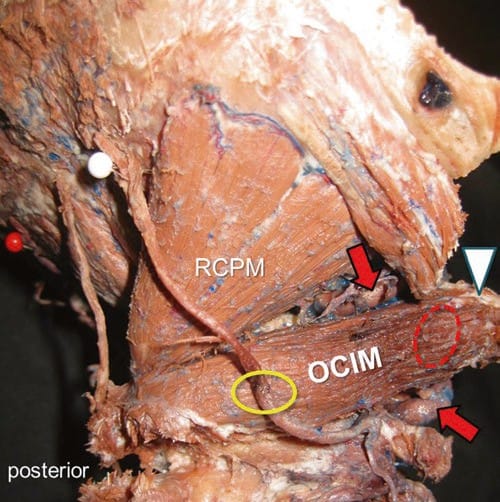
Fig.3 Topography of the vertebral artery (VA) at C2/C1 level (detail of specimen in Fig.1, more lateral view). Before entering the suboccipital triangle, the VA (red arrows) courses anterior (red oval) to the obliquus capitis inferior muscle (OCIM) near its attachment at the transverse process of the atlas (white arrowhead). The yellow oval indicates the site of GON block on the posterior surface of the OCIM. RCPM rectus capitis posterior major muscle
2. TRADITIONAL METHOD OF GON BLOCK: LIMITATIONS AND DISADVANTAGES
The traditional “blind” technique of GON block just medial to the pulsation of the occipital artery at the level of the superior nuchal line has several limitations and shortcomings. Because of the noticeable variability and multiple branching of the GON at this peripheral location, relatively high volumes are needed to get a reliable block effect. The inevitable result is intramuscular infiltration and blocks of other nearby nerves, such as branches of the lesser and third occipital nerve and even the greater auricular nerve. This technique is therefore not at all specific and misses diagnostic properties. In cases with altered anatomy, “blind” injection in this area can cause unwanted and alarming complications such as sudden coma [12, 13]. Finally, US identification of the GON at the classic site is more difficult than at a more central location [1].
3. ULTRASOUND-GUIDED GON BLOCK: OUR TECHNIQUE AND EXPERIENCE
Scanning Techniques
The patient can be positioned prone, sitting, or in lateral decubitus (our preference), with the head in neutral position and the cervical spine in anteflexion. We usually place a linear high-frequency (10–12 MHz) transducer on the skin, positioned along the course of the OCIM: slightly oblique, with the medial end pointing toward the spinous process of the axis and the lateral end pointing toward the transverse process of the atlas, to obtain the best possible transverse view of the GON (see Figs. 2a and 4c). A transducer with a larger footprint or a convex transducer with low frequency may help by offering an expanded field of view in this area. If available, the virtual sector technique may equally be applied (Fig. 4d). That way, the OCIM may be visualized in its entirety from the attachment to the axis on the medial end to the atlas on the lateral end. Even with the use of a lower frequency, the GON is seen in most individuals. This technique is especially helpful for “big necks.”
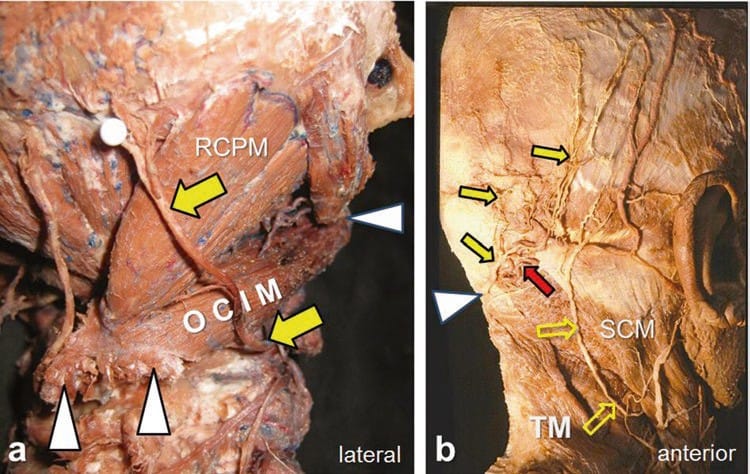
Fig.1 Topography of the greater occipital nerve (GON) (yellow arrows). (a) The specimen (right side, posterolateral view) shows the deep course of the GON prior to bifurcation; the semispinalis capitis muscle (SsCM) has been removed. The white pinhead indicates the level where the GON becomes superficial in the occipital region; this corresponds to the spot where it pierces the trapezius muscle. The white arrowheads indicate the right and left tubercles of the spinous process of the axis (medially) and the transverse process of the atlas (laterally). The obliquus capitis inferior muscle (OCIM) is the important deep muscular landmark for localizing the GON at the C2/C1 level because the GON is consistently found ascending on its dorsal surface. RCPM—rectus capitis posterior major muscle. (b) The superficial course of the GON and its relation to the lesser occipital nerve (open yellow arrows); note the anastomoses between them. The white arrowhead indicates the point where the GON pierces the trapezius muscle (TM); the nerve is seen medial to the occipital artery (red arrow). SCM sternocleidomastoid muscle
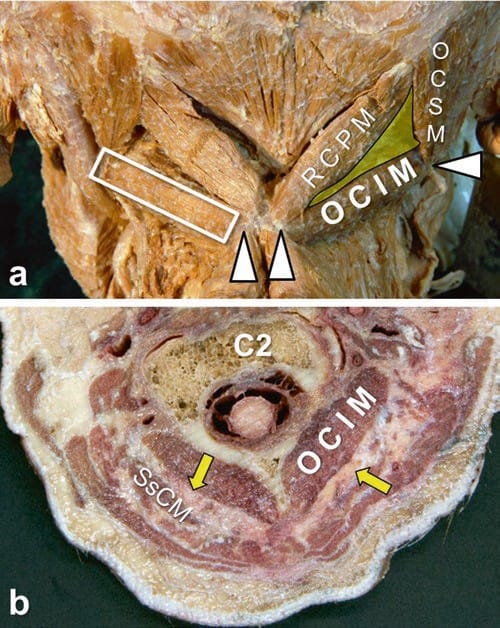
Fig.2 Short muscles of the neck, including the obliquus capitis inferior muscle (OCIM). (a) Posterior view of both suboccipital triangles (right one colored). The inferior border of the triangle is the prominent OCIM, which connects the spinous process of the axis with the transverse process of the atlas (white arrowheads). The remaining borders of the triangle are built by the rectus capitis posterior major muscle (RCPM) and the obliquus capitis superior muscle (OCSM); the white open rectangle indicates an accurate transducer position. (See also Fig.6.) (b) Cross section through the neck along both OCIMs (Cf. Fig.5); the GON (yellow arrows) lies sandwiched between the OCIM and the semispinalis capitis muscle (SsCM). C2 body of axis
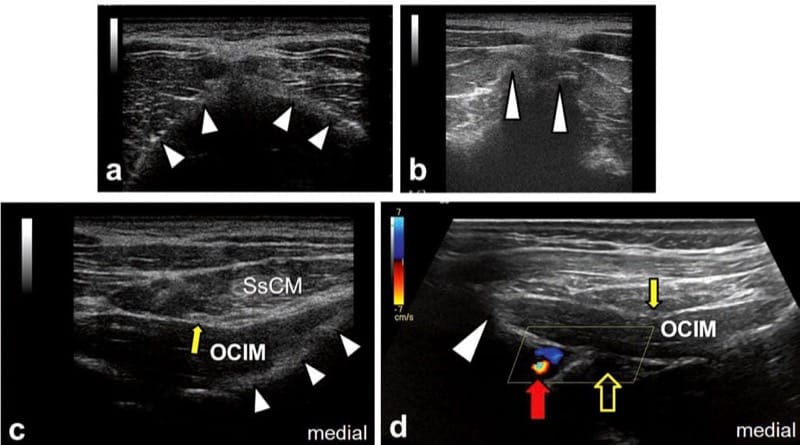
Fig.4 Systematic procedure for ultrasound detection of the greater occipital nerve (GON). (a) After moving the probe downward from its initial position over the external occipital protuberance, the surface of the posterior arch of the atlas (white arrowheads) comes into sight. Note that the atlas has no spinous process. (b) Shifting the transducer further caudally, the two tubercles of the massive spinous process of the axis become obvious (white arrowheads). This is the most important osseous sonoanatomic landmark to locate the obliquus capitis inferior muscle (OCIM). (c) Relative to the overlying semispinalis capitis muscle (SsCM), the OCIM is typically hypoechoic; the oval-shaped GON (yellow arrow) is clearly seen “on top of” the OCIM; white arrowheads outline the lamina of the axis. (d) The vertebral artery (red arrow) can be depicted near the transverse process of the atlas (white arrowhead) and anterior to the OCIM, either by moving the probe more laterally or using appropriate transducers; in this case, the virtual sector technique is used. Note that the GON (yellow arrow) is within a safe distance to the vertebral artery. The yellow open arrow indicates the position of the second dorsal root ganglion
We recommend that beginners perform the following systematic sonoanatomic survey from cephalad to caudad, starting in the midline: first, the transducer is placed over the palpable external occipital protuberance to capture a transverse view of this bony landmark and the surface of the occiput. Then the transducer is moved slowly caudad to capture a transverse view of the posterior arch of the atlas below the occiput (Fig.4a). It is then moved further caudad to the C2 level, where the axis has a characteristically prominent bifid spinous process with left and right tubercles (Figs. 4b and 1a). After identification of this important landmark, the transducer is moved laterally to visualize the OCIM. The best images are obtained if the lateral end of the transducer is oriented slightly inferior to another palpable landmark, the tip of the mastoid process. The muscle is seen posterior to the lamina of the axis and deep to the SsCM. As a rule, the OCIM is hypoechoic compared with the overlying SsCM. Sandwiched between the SsCM and OCIM, the GON appears as an oval-shaped, hypoechoic structure (Fig. 4c). It is advisable to follow the OCIM laterally as far as its attachment to the atlas, to locate the vertebral artery (which can be confirmed by color Doppler if necessary), anterior to the OCIM (Fig. 4d). Finally, the transducer is repositioned more medially to perform the block.
In summary, quite a number of internal sonographic bony, muscular, and vascular landmarks help to localize the GON. The bony landmarks are the occiput, with the sonographic prominent external occipital protuberance; the arch of the atlas, with no spinous process; and the axis, with its big, bifid spinous process. The muscular landmarks are the OCIM and the SsCM. The vascular landmark is the vertebral artery, which is lateral to the GON and anterior to the lateral part of the OCIM. A neural landmark, the second dorsal root ganglion, is medial to the vertebral artery and anterior to OCIM (Figs. 5 and 4d).
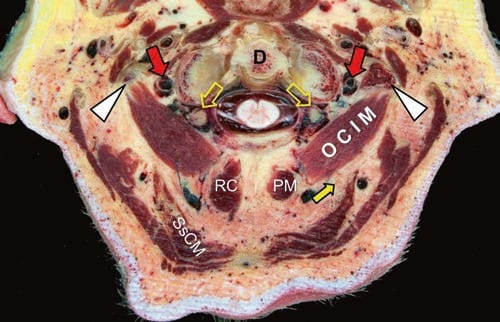
Fig.5 Cross section through the neck at C1 level (Cf. Fig.2b) and topography of the vertebral artery (VA). Near the transverse processes of the atlas (white arrowheads), the VAs (red arrows) are located anterior to the OCIMs; also in front of the OCIM but medial to the VAs, the second dorsal root ganglia (yellow open arrows) are clearly seen (Cf. Fig.4d). At this level, the GON (yellow arrow) has already lifted from the dorsal surface of the OCIM as it starts entering the SsCM. D dens of axis; RCPM rectus capitis posterior major muscles
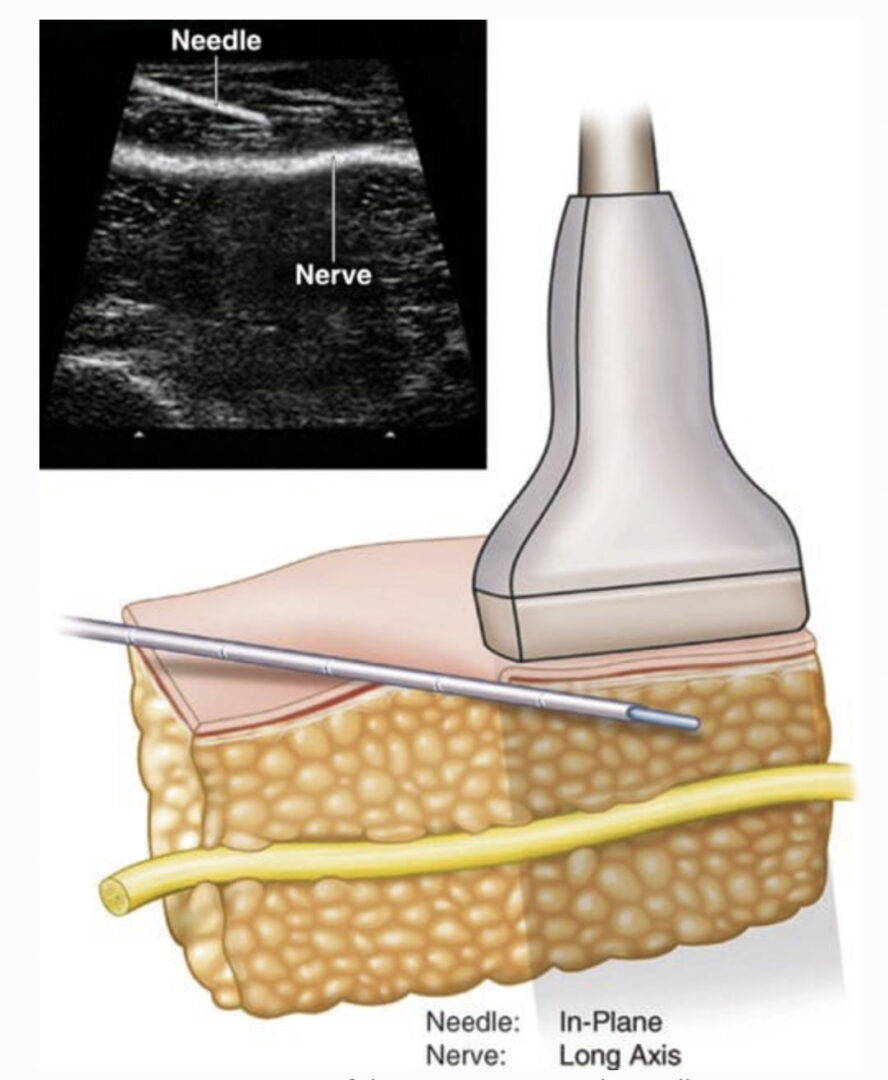
4. NERVE BLOCK
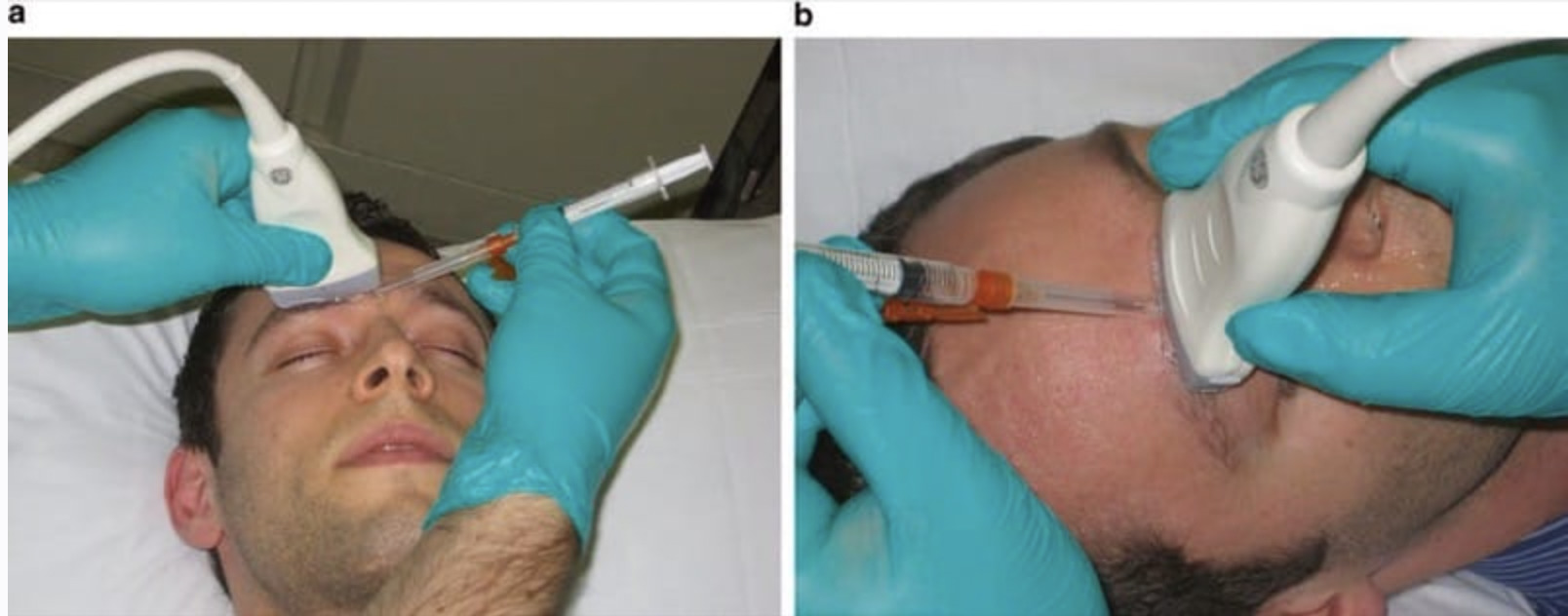
We prefer to position the patient in lateral decubitus position because it is more comfortable for the performer and better for the patient’s circulatory stability. The cervical spine must be in anteflexion, but there must be absolutely no lateral flexion. After appropriate skin and transducer preparation, a 5-cm 25-G needle connected to a 5-mL syringe with an extension line is inserted, preferably in-plane and in the lateral-to-medial direction. More experienced practitioners may also advance the needle in an out-of-plane manner. Usually, 3–5 mL of local anesthetic are injected slowly around the GON after a negative aspiration test. Studies regarding the addition of steroids are mixed [14, 15]. Ultrasound visualization of nearby vessels (Fig. 6) helps to avoid inadvertent intravascular injection. In rare cases where the GON is not clearly seen, the needle tip can be placed in the plane between the OCIM and SsCM. By using hydrodissection, the plane is carefully distended and the nerve is finally exposed.
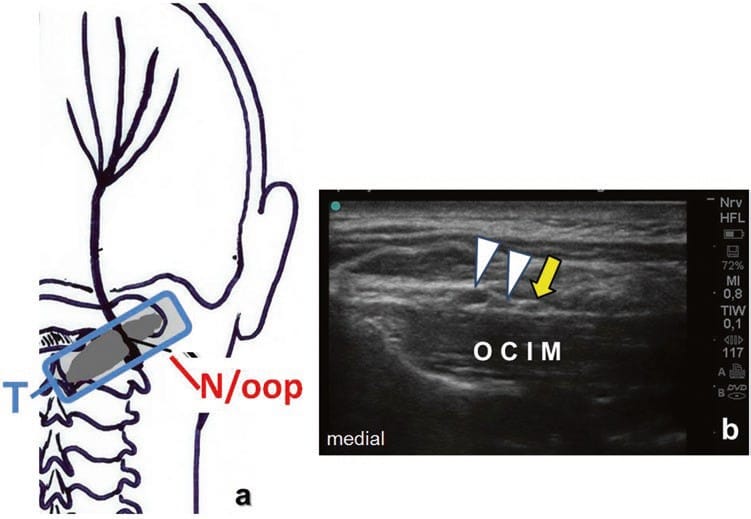
Fig.6 Ultrasound-guided GON block. (a) Transducer position (T) and the needle insertion point with out-of- plane technique (N/oop). (b) Corresponding ultrasound image showing the OCIM, two compressible veins (white arrowheads), and the GON (yellow arrow)
5. EXPERIENCE AND OUTLOOK
Sonographic studies have provided standard measurements for the GON at both the superior nuchal line [16] and at the OCIM [17]. The technique described for visualizing the OCIM for GON blocks is potentially useful also for ultrasound-guided placement of occipital stimulation devices [18]. This sonographic technique also may gain importance for ultrasound-guided trigger point injection or botulinum toxin injection around the GON [19] or into the OCIM.
6. CONCLUSION
Ultrasound-guided GON blocks at the level of the OCIM are target-specific and are very useful for the diagnosis of occipital neuralgia and the treatment of this disorder, as well as other types of headache (like migraine or cervicogenic headache) and even some types of facial pain, such as trigeminal neuralgia. Following our technique, the GON can reliably be identified and block complications can be avoided through direct visualization of the needle tip, the target, and the local anesthetic spread.