General Considerations The need for effective analgesia in the perioperative period for major lower limb surgery has generated interest in the field of regional anesthesia. These regional techniques are commonly performed before central neuraxial block, but they could potentially be used as the sole anesthetic technique in conjunction with monitored sedation techniques. Regional anesthesia of the lower limb in conjunction with a multimodal analgesic regimen could provide obvious advantages such as opioid sparing, shorter hospital stay, improved patient satisfaction, and better functional outcomes [1]. This chapter describes the current methods and reasons for performing specific blocks to the lower limb utilizing ultrasound guidance. Ultrasound imaging provides direct visualization of needle tip as it approaches the desired nerves and real-time control of the spread of local anesthetics [2, 3]. Inclusion of this tool requires the operator to have a working knowledge and understanding of the principles of ultrasound, in combination with good hand-eye coordination for optimization of probe and needle handling techniques [4]. The ultrasound device used ideally possesses a high-frequency (7–12 MHz) linear array probe, suited for looking at superficial structures (up to an approximate depth of 50 mm), and a low-frequency (2–5 MHz) curved array probe, which provides better tissue penetration and a wider field of view (but at the expense of resolution) (Fig. 1). When using the ultrasound machine to assist with blocks, the operator should practice good ergonomic positioning to prevent operator fatigue and thus improve block performance (Fig. 2). When holding the probe, it is often helpful to steady its position by gripping it lower down and placing the operator’s fingers against the patient’s skin [5].
1. FEMORAL NERVE BLOCK
Clinical Application
The femoral nerve block provides analgesia and anesthesia to the anterior aspect of the thigh and knee, as well as the medial aspect of the calf and foot via the saphenous nerve. A single injection or continuous catheter technique can be used. When combined with a sciatic nerve block, it provides complete anesthesia and analgesia below the knee joint.
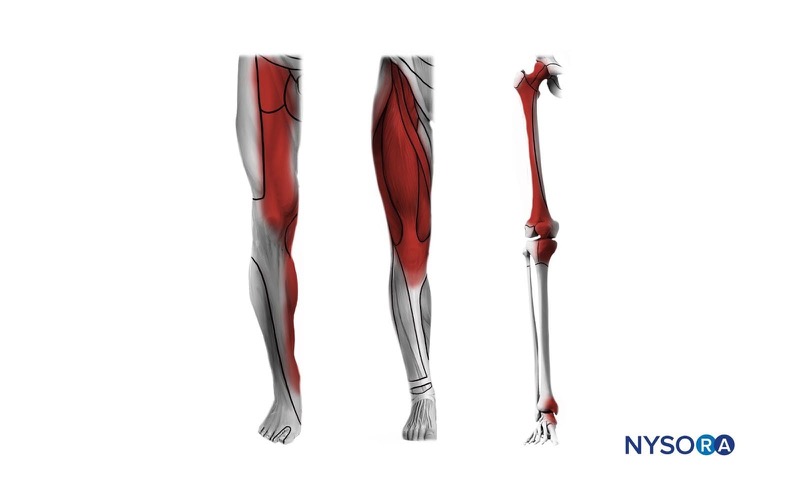
Cognitive aid: Anesthesia distribution of the femoral nerve block. Left: dermatomes, middle: myotomes, right: osteotomes.
For additional information check NYSORA Compendium: Femoral Nerve Block.

Fig.1 Linear probe (left), curvilinear probe (right)

Fig.2 Proper positioning of operator using an ultrasound machine
2. ANATOMY
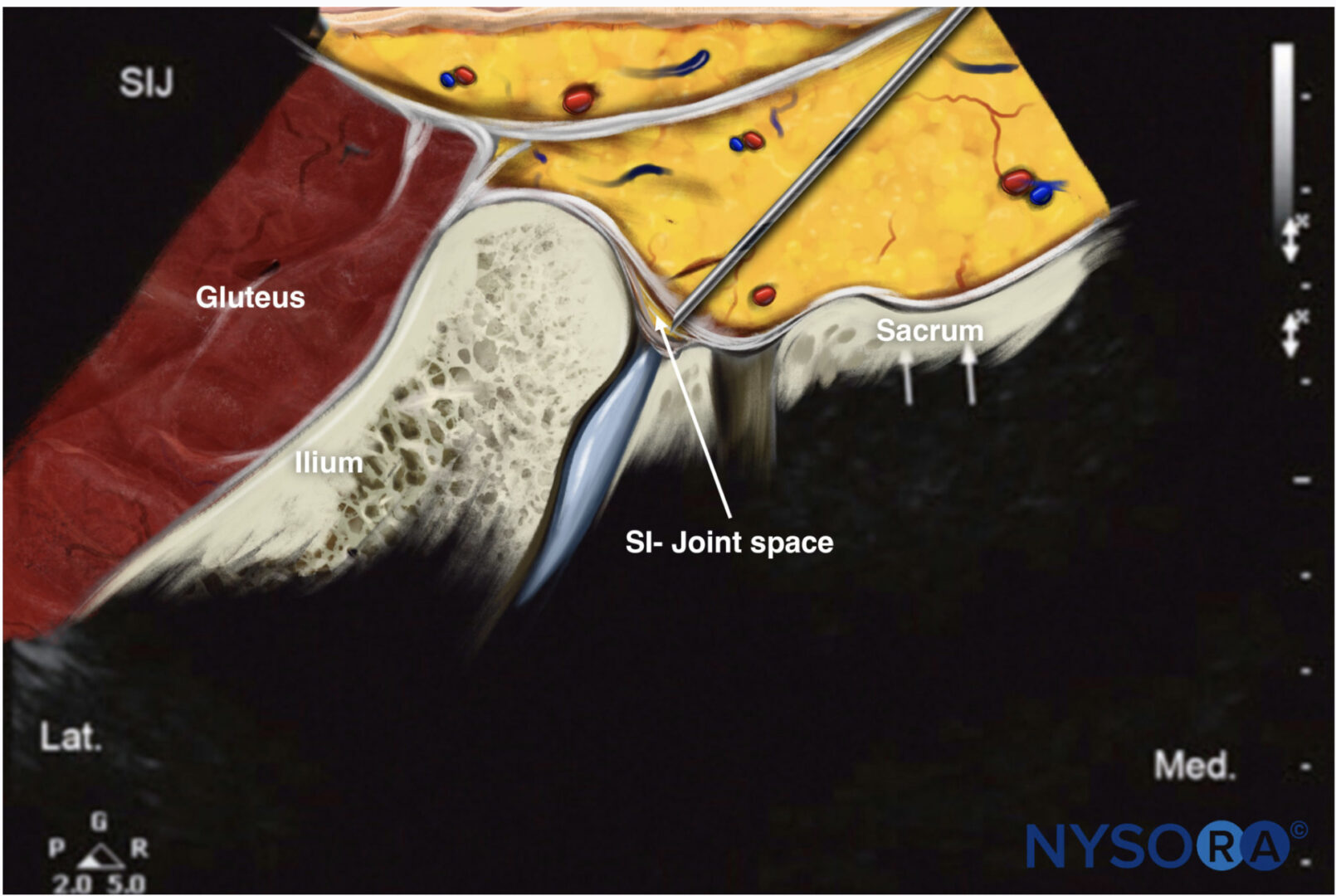
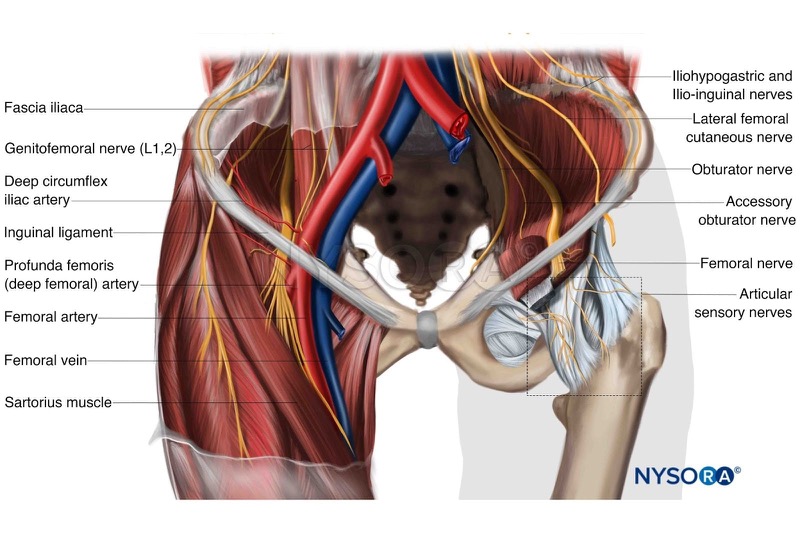
The femoral nerve arises from the lumbar plexus (L2, L3, and L4 spinal nerves) and travels through the body of the psoas muscle [6]. It lies deep to the fascia iliaca, which extends from the posterior and lateral walls of the pelvis and blends with the inguinal ligament, and superficial to the iliopsoas muscle. The femoral artery and vein lie anterior to the fascia iliaca. The vessels pass behind the inguinal ligament and become invested in the fascial sheath. Thus the femoral nerve, unlike the femoral vessels, does not lie within the fascial sheath, but lies posterior and lateral to it (Figs. 3 and 4). The fascia lata overlies all three femoral structures: nerve, artery, and vein. Thus the femoral nerve is amenable to sonographic examination, given its superficial location and consistent position lateral to the femoral artery.
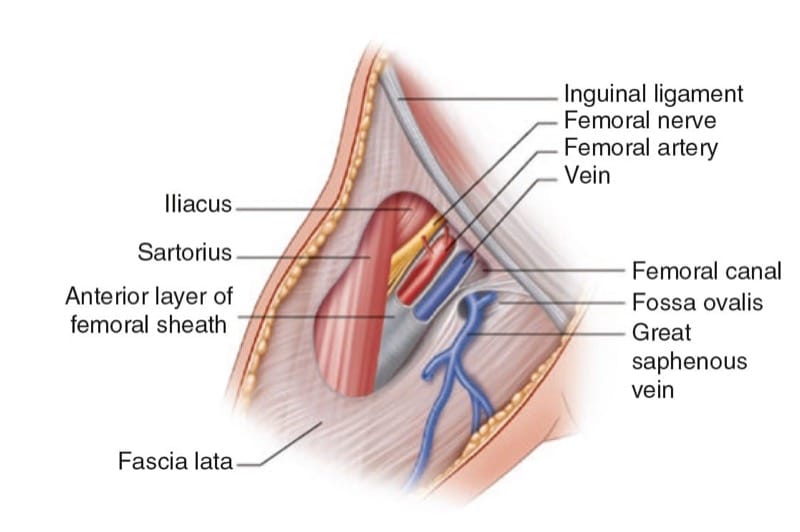
Fig.3 The femoral nerve and its relations to the femoral triangle
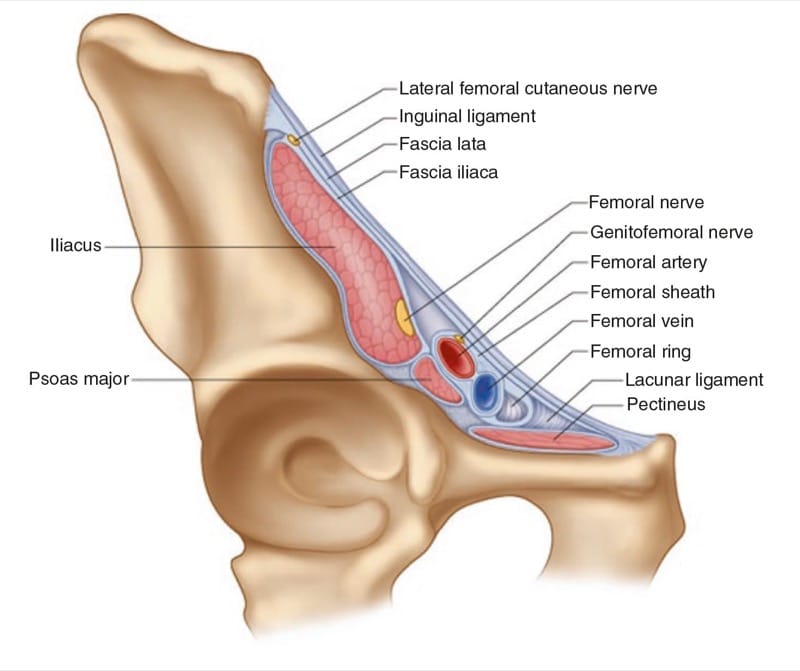
Fig.4 The femoral nerve
3. PREPARATION AND POSITIONING
Intravenous access is established and standard monitors are applied. The patient is placed supine with the leg in the neutral position. Intravenous sedative agents and oxygen therapy are administered as required. In patients with high body mass index, it may be necessary to retract the lower abdomen to expose the inguinal crease. This may be performed by an assistant or by using adhesive tape, going from the patient’s abdominal wall to an anchoring structure such as the side arms of the stretcher. Skin disinfection is then performed and a sterile technique observed.
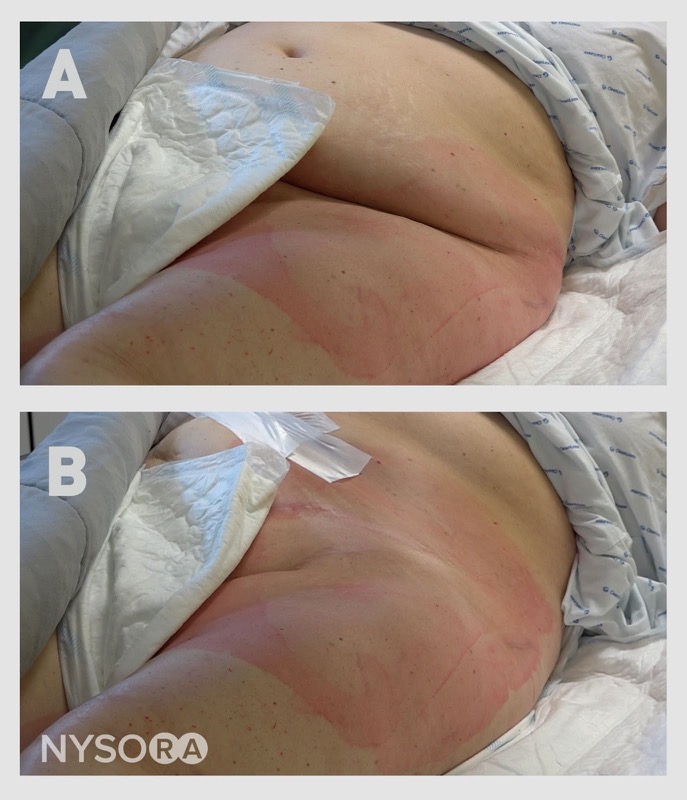
Cognitive aid: Taping of the lower abdomen to expose the inguinal crease.
For additional information check NYSORA Compendium: Femoral Nerve Block.
4. ULTRASOUND TECHNIQUE
A high-frequency (7–12 MHz) linear ultrasound is placed along the inguinal crease. Either an in-plane or out-of-plane approach may be used (Figs. 5 and 6).

Fig.5 In-plane approach for the femoral nerve block

Fig.6 Out-of-plane approach for the femoral nerve block
The ultrasound probe is placed to identify the femoral artery and then is moved laterally, keeping the femoral artery visible on the medial aspect of the screen. It is often easier to see the femoral nerve when it is visualized more proximally beside the common femoral artery, rather than distal to the branching of the profunda femoris artery. Thus, if two arteries are identified, scan more proximally until only one artery is visible. The femoral nerve appears as a hyperechoic, flattened oval structure lateral to the femoral artery (Fig. 7).
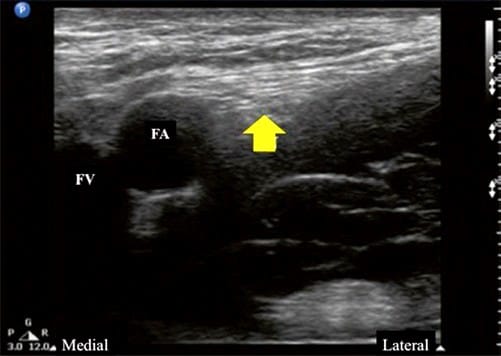
Fig.7 Transverse scan of inguinal region. The arrowhead indicates the femoral nerve. FA femoral artery, FV femoral vein
The femoral nerve is usually observed 1–2 cm lateral to the femoral artery. Once the femoral nerve has been identified, lidocaine is infiltrated into the overlying skin and subcutaneous tissue. The distension of the subcutaneous tissues with infiltration of the lidocaine can be seen on the ultrasound image.
5. SINGLE-INJECTION TECHNIQUE
A 20-mL syringe is attached to the 50-mm block needle. The block needle is inserted either in an in-plane or out-of-plane approach. Whether an in-plane or out-of-plane approach is used, the needle tip should be constantly visualized with ultrasound. The advantage of the in-plane approach is that it is usually possible to visualize the whole shaft of the needle, whereas only the tip may be visible with an out-of-plane approach. The needle is aimed adjacent to the nerve. Using ultrasound guidance alone, it is possible to deliberately direct the needle a few centimeters lateral to the femoral vessels and nerve under the fascia iliaca. If nerve stimulation is used, either a quadriceps muscle contraction (patellar twitch) or a sartorius muscle contraction is satisfactory as an end point. After a negative aspiration test for blood, 20 mL of local anesthetic is injected in 5-mL increments. The spread of the local anesthetic can be visualized in real time as hypoechoic solution surrounding the femoral nerve, and the needle tip is repositioned if required to ensure appropriate spread. Figures 8 and 9 illustrate the image of the femoral nerve before and after the injection of local anesthetic around it. In Fig. 8, the femoral structures are identified with the block needle in place. Figure 9 shows the spread of local anesthetic around the femoral nerve.
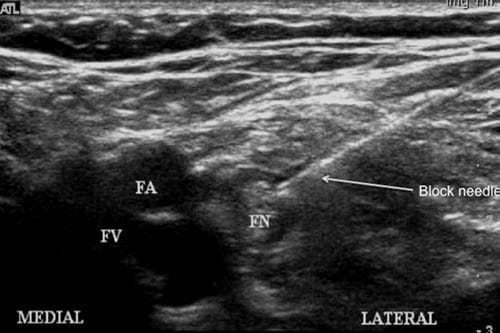
Fig.8 Femoral structures with block needle in place, using an in- plane approach. FA femoral artery, FN femoral nerve, FV femoral vein

Fig.9 Local anesthetic spread around femoral structures. FA femoral artery, FN femoral nerve, FV femoral vein
6. CONTINUOUS CATHETER TECHNIQUE
This technique is similar to the single-injection technique. An in-plane or out-of-plane approach may be employed. An 80-mm, 17 G insulated needle with a 20G catheter is used. If nerve stimulation is utilized, then it is attached to the catheter and not to the introducing needle. The catheter is placed within the introducer needle such that its tip is well within the introducer needle, in order to prevent any catheter tip damage as the introducer is positioned. Care must be taken to grip the catheter together with the introducer needle at its hub to prevent any unwanted migration of the catheter further into the introducer needle. An electrical circuit is still formed as current passes from the tip of the catheter to the tip of the introducer needle and into the patient. The introducer needle tip is visualized in the correct position by ultrasound, and the quadriceps contraction occurs at a current of 0.3– 0.5 mA if electrical stimulation is utilized. The needle may be repositioned at this point to a more horizontal position, to enable the threading of the catheter. The catheter is now advanced and electrical stimulation (if used) is maintained. Catheter insertion should be without resistance. If not, then the needle needs to be repositioned. The catheter is usually advanced further in the space as the introducer needle is removed, such that it is approximately 5 cm beyond where the tip of the introducer needle was placed. (Thus it is usually about 10 cm at the skin.) The catheter’s position is secured and dressings are applied. Local anesthetic spread can be visualized as it surrounds the femoral nerve in both the transverse and longitudinal planes.
7. SCIATIC NERVE BLOCK
Clinical Application
block of the sciatic nerve results in anesthesia and analgesia of the posterior thigh and lower leg. When combined with a femoral nerve, saphenous nerve, or lumbar plexus block, it provides complete anesthesia of the leg below the knee.
8. ANATOMY
The last two lumbar nerves (L4 and L5) merge with the anterior branch of the first sacral nerve to form the lumbosacral trunk. The sacral plexus is formed by the union of the lumbosacral trunk with the first three sacral nerves (Fig. 10). The roots form on the anterior surface of the lateral sacrum and become the sciatic nerve on the ventral surface of the piriformis muscle. It exits the pelvis through the greater sciatic foramen below the piriformis muscle and descends between the greater trochanter of the femur and the ischial tuberosity between the piriformis and gluteus maximus, and then the quadratus femoris and the gemelli muscles and gluteus maximus. More distally, it runs anterior to the biceps femoris before entering the popliteal triangle. At a variable point before the lower third of the femur, it divides into the tibial and common peroneal nerves.
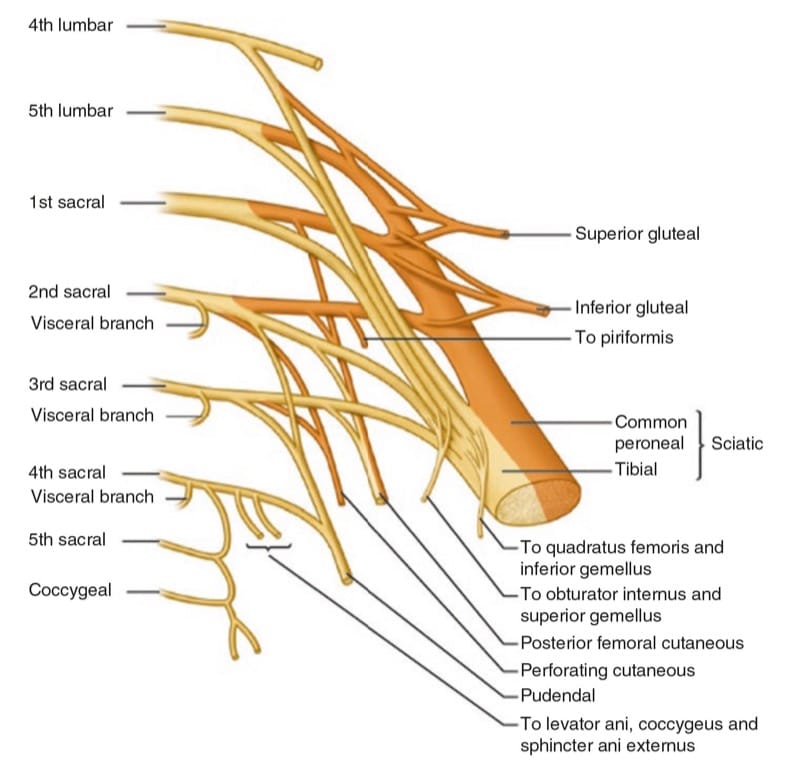
Fig.10 The sacral plexus
9. PREPARATION AND POSITIONING
After adequate monitoring and intravenous access is established, the patient is placed in a lateral decubitus position with the side to be blocked uppermost. The knee is flexed and the foot positioned so that twitches of the foot are easily seen. Bony landmarks are identified, which include the greater trochanter and the ischial tuberosity. The sciatic nerve lies within a palpable groove, which can be marked prior to using the ultrasound. Skin disinfection is then performed and a sterile technique observed.
10. ULTRASOUND TECHNIQUE
The sciatic nerve is the largest peripheral nerve in the body, measuring more than 1 cm in width at its origin and approximately 2 cm at its greatest width. Multiple different approaches are described using surface landmarks. The sciatic nerve is amenable to imaging with ultrasound, but it is considered a technically challenging block because of the lack of any adjacent vascular structures and its deep location relative to skin. It can be approached with either an in-plane approach (Fig. 11) or an out-of-plane approach (Fig. 12).
A low-frequency curved array probe (2–5 MHz) is preferred. The ultrasound probe is placed over the greater trochanter of the femur, and its curvilinear bony shadow is delineated. The probe is moved medially to identify the curvilinear bony shadow of the ischial tuberosity. The sciatic nerve is visible in a sling between these two hyperechoic bony shadows (Fig. 13). It usually appears as a wedgeshaped hyperechoic structure that is easier to identify more proximally, and then followed down to the infragluteal region. It is often easier to identify it from its surrounding structures by decreasing the gain on the ultrasound machine.

Fig.11 In-plane approach for the sciatic nerve block, subgluteal approach

Fig.12 Out-of-plane approach for the sciatic nerve block, subgluteal approach
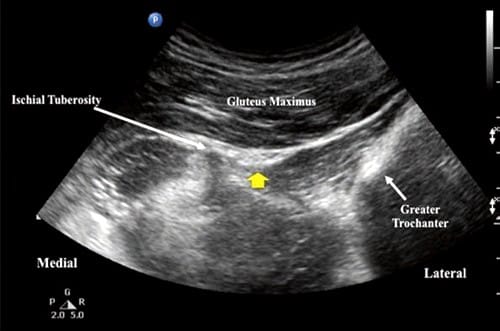
Fig.13 Transverse scan of sciatic nerve (arrowhead)
The depth of the sciatic nerve varies mainly with body habitus. To reach the target, the angle of approach of the needle is often close to perpendicular to the skin [7]. This makes visualization of the entire needle shaft using the inplane approach more difficult. An out-of-plane approach is often used, whereby only a cross-sectional view of the needle is visible. The skin is infiltrated with lidocaine at the point of insertion of the block needle. The needle tip is tracked at all times. Imaging of the needle tip, this deep can be problematic, and its position is often inferred from the movement of the tissues around it, and by injections of small volumes of D5W, local anesthetic, or air. Electrical stimulation can be used to help confirm needle-to-nerve contact. It is useful to use the ultrasound to observe the pattern of local anesthetic spread around the sciatic nerve in real time. The aim is to reposition the needle tip if required to obtain circumferential spread around the nerve, but this goal cannot always be achieved, as moving the needle around the nerve can be technically challenging.
11. SCIATIC NERVE block IN THE POPLITEAL FOSSA
Clinical Application
Sciatic nerve block distally at the popliteal fossa is used for anesthesia and analgesia of the lower leg. As opposed to more proximal sciatic nerve block, popliteal fossa block anesthetizes the leg distal to the hamstring muscles, allowing patients to retain knee flexion.
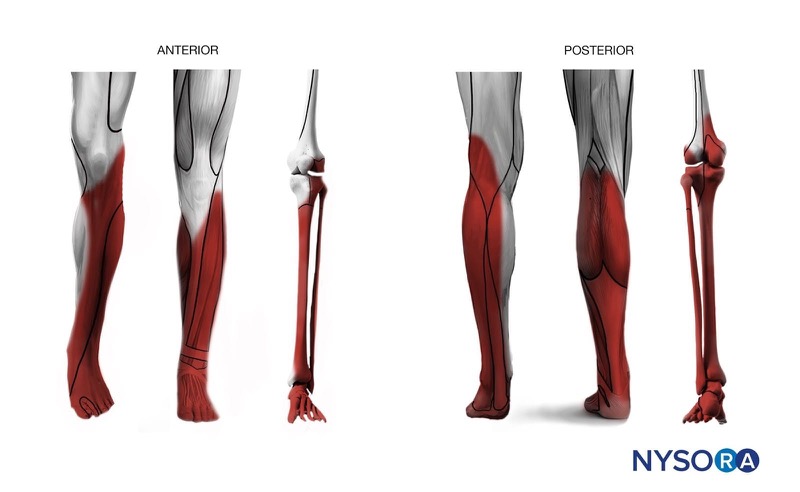
Cognitive aid: Anesthesia distribution with a popliteal sciatic nerve block. Left: dermatomes, middle: myotomes, right: osteotomes.
For additional information check NYSORA Compendium: Popliteal Sciatic Nerve Block.
12. ANATOMY
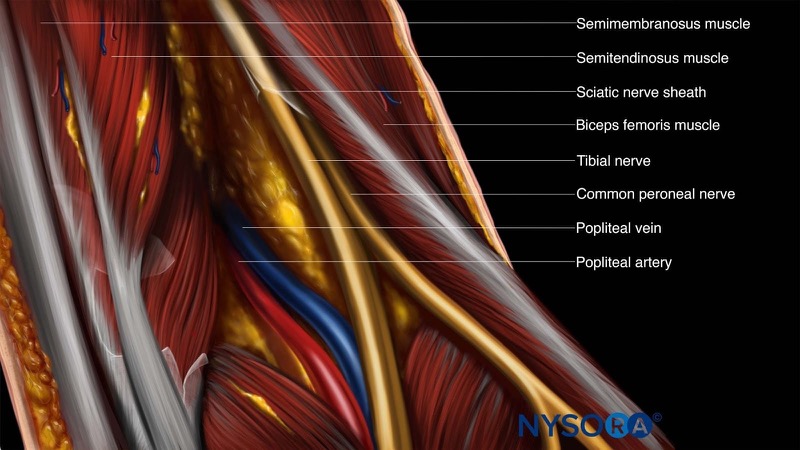
The sciatic nerve is a nerve bundle containing two separate nerve trunks, the tibial and common peroneal nerves. The sciatic nerve passes into the thigh and lies anterior to the hamstring muscles (semimembranosus, semitendinosus, and biceps femoris [long and short heads]), lateral to the adductor magnus, and posterior and lateral to the popliteal artery and vein. At a variable level, usually between 30 and 120 mm above the popliteal crease, the sciatic nerve divides into the tibial (medial) and common peroneal (lateral) components [8]. The tibial nerve, the larger of the two divisions, descends vertically through the popliteal fossa, where distally it accompanies the popliteal vessels. Its terminal branches are the medial and lateral plantar nerves. The common peroneal nerve continues downward and descends along the head and neck of the fibula. Its superficial branches are the superficial and deep peroneal nerves. Since most foot and ankle surgical procedures involve both tibial and common peroneal components of the nerve, it is essential to anesthetize both nerve components. block of the nerve before it divides therefore simplifies the technique.
Cognitive aid: Anatomy of the sciatic nerve in the popliteal fossa.
For additional information check NYSORA Compendium: Popliteal Sciatic Nerve Block.
13. PREPARATION AND POSITIONING
Noninvasive monitors are applied and intravenous access obtained. The patient is placed prone. The foot on the side to be blocked is positioned so that any movement of the foot can be easily seen, placed with the foot hanging off the end of the bed with a pillow under the ankle. Oxygen therapy and adequate intravenous sedation are administered. The popliteal crease is identified, and the inner borders of the popliteal fossa are marked. Skin disinfection is performed and a sterile technique is observed. Once the block has been inserted, the patient is moved supine for the operative procedure.
14. ULTRASOUND TECHNIQUE
Ultrasound imaging allows the nerves to be followed to determine their exact level of division, removing the need to perform the procedure an arbitrary distance above the popliteal fossa. Thus an insertion point can be chosen that minimizes the distance to the nerve from the skin. Both the in-plane and out-of-plane approach may be used (Figs.14 and 15).
A high-frequency (7–12 MHz) linear array probe is appropriate for this block. Start with the ultrasound probe in a transverse plane above the popliteal crease. The easiest method for finding the sciatic nerve is to follow the tibial nerve. Locate the popliteal artery at the popliteal crease. The tibial nerve will be found lateral and posterior to it, as a hyperechoic structure. Follow this hyperechoic structure until it is joined further proximal in the popliteal fossa by the peroneal nerve. The sciatic nerve can also be found directly above the popliteal fossa by looking deep and medial to the biceps femoris and semitendinosus muscles and superficial and lateral to the popliteal artery (Fig. 16).

Fig.14 In-plane approach for the popliteal nerve block

Fig.15 Out-of-plane approach for the popliteal nerve block

Fig.16 Transverse section of the popliteal region. PA popliteal artery, BF biceps femoris muscle, TN popliteal nerve, SM semimem-branosus muscle, PV popliteal vein
It is often useful to angle the ultrasound probe caudally to enhance nerve visibility. If nerve visualization is difficult, the patient is asked to plantarflex and dorsiflex the foot. This causes the tibial and peroneal components to move during foot movement, called the “seesaw sign.”
Once the sciatic nerve has been identified in the popliteal fossa, the skin is infiltrated with lidocaine at the desired point of insertion of the block needle. The out-of-plane technique is commonly used, as it is simpler and less uncomfortable for the patient, but it does not allow visualization of the whole needle shaft.
The block needle is inserted and directed next to the sciatic nerve. Once the needle tip lies adjacent to the nerve, a muscle contraction can be elicited, if preferred, by slowly increasing the nerve stimulator current until a twitch is seen (commonly less than 0.5 mA). After negative aspiration for blood, local anesthetic is incrementally injected. It is important to examine the spread of local anesthetic and ensure that spread is seen encircling the nerve. Needle repositioning may be needed to ensure adequate spread on either side of the nerve (Fig. 17).
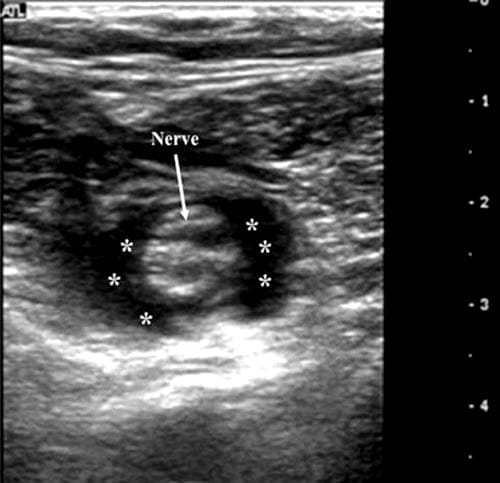
Fig.17 View of popliteal nerve after injection of local anesthetic (asterisk)
15. LUMBAR PLEXUS BLOCK
Clinical Application
Lumbar plexus block (psoas compartment block) leads to anesthesia and analgesia of the hip, knee, and anterior thigh. Combined with sciatic nerve block, it provides anesthesia and analgesia for the whole leg.
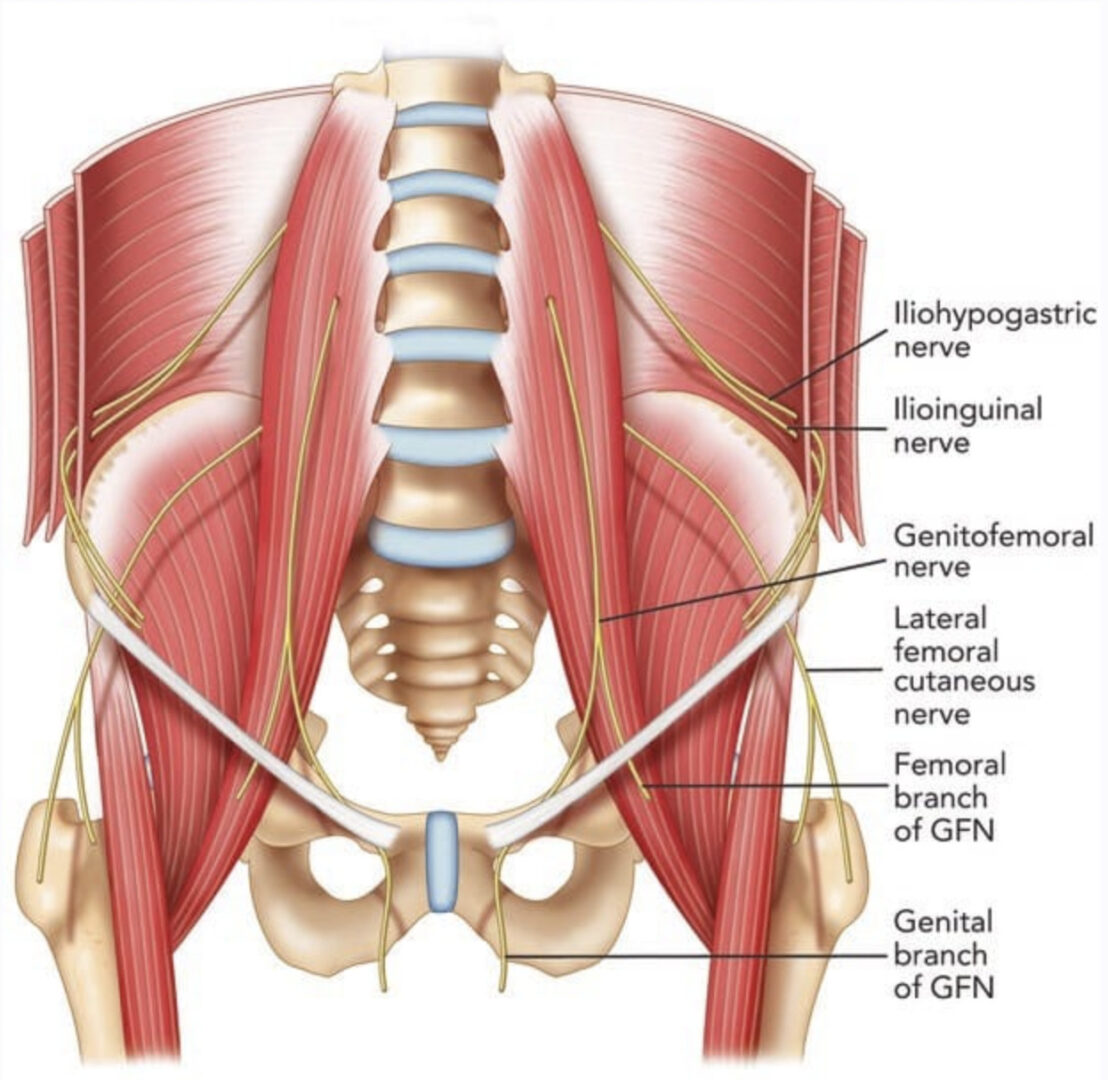
16. ANATOMY
The lumbar plexus is formed from the anterior divisions of L1, L2, L3, and part of L4 (Fig. 18). The L1 root often receives a branch from T12. The lumbar plexus is situated most commonly in the posterior one third of the psoas major muscle, anterior to the transverse processes of the lumbar vertebrae. The major branches of the lumbar plexus are the genitofemoral nerve, the lateral cutaneous femoral nerve of the thigh, and the femoral and obturator nerves.
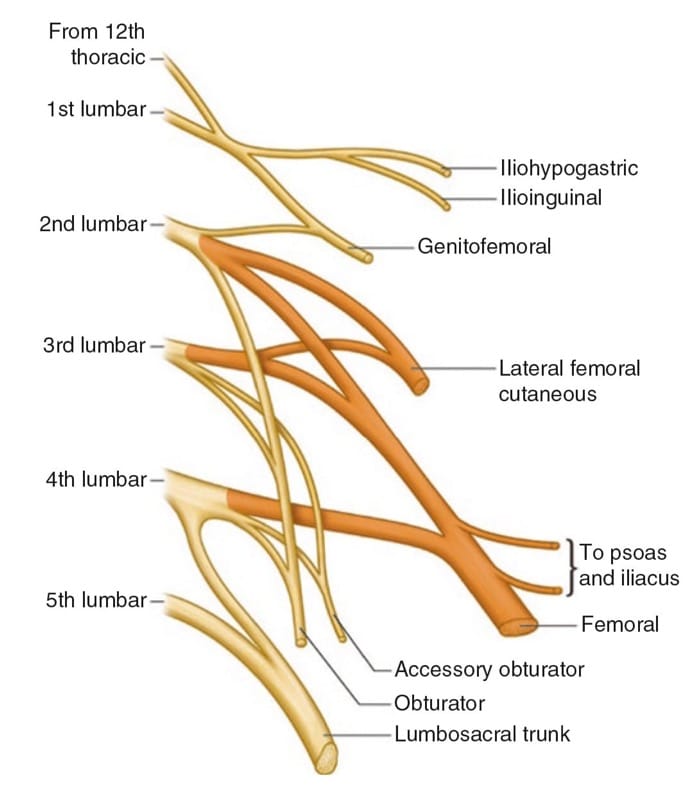
Fig.18 The lumbar plexus
17. PREPARATION AND POSITIONING
The patient is placed in the lateral decubitus position with the side to be blocked uppermost. The leg must be positioned such that contractions of the quadriceps muscle are visible. Noninvasive monitors are applied and intravenous access obtained. Intravenous sedative agents and oxygen therapy are administered as required. More sedation is usually required for lumbar plexus blocks than for other techniques, as the block needle has to pass through multiple muscle planes. Skin disinfection is performed and a sterile technique observed.
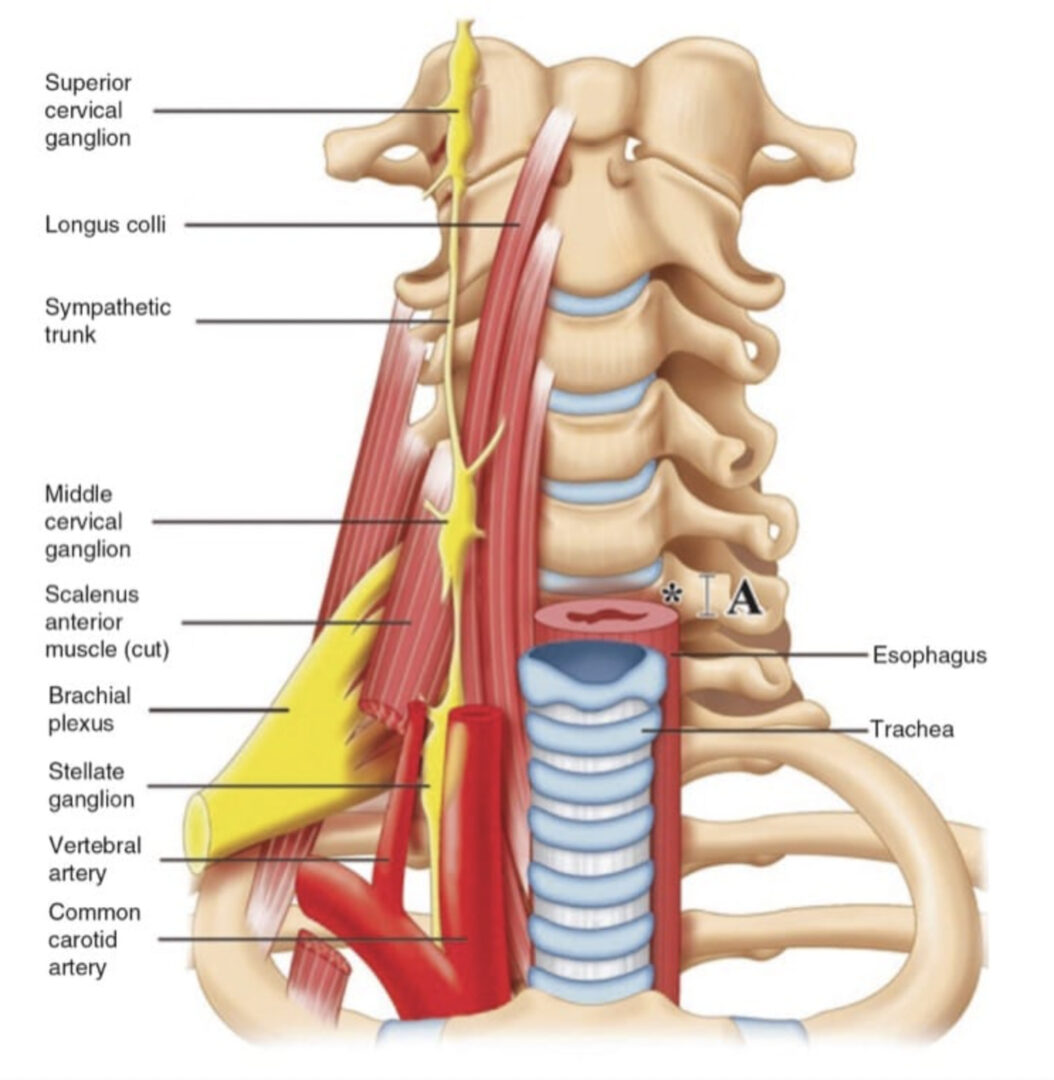
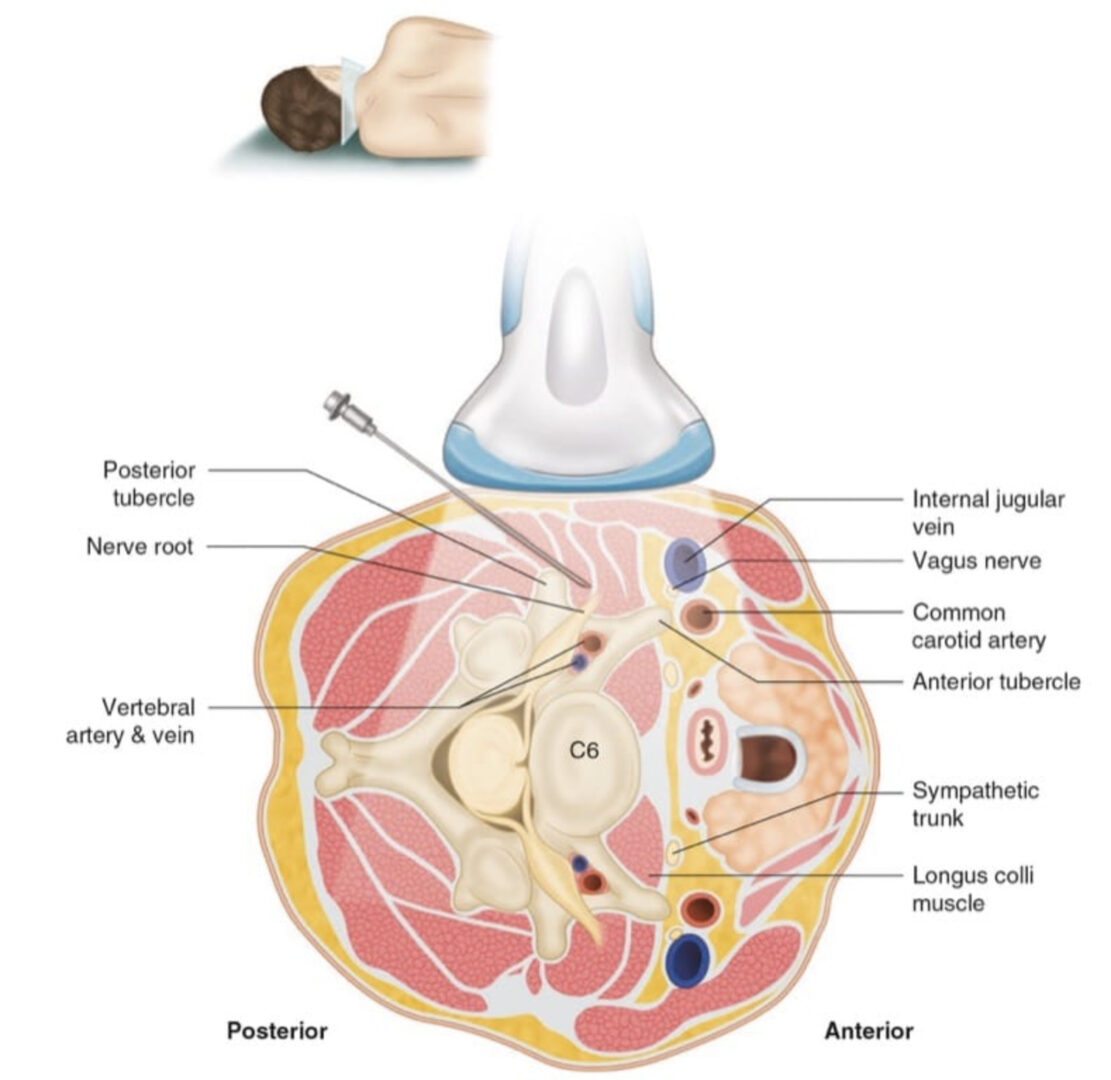
18. ULTRASOUND TECHNIQUE
This is considered to be an advanced technique because of the depth of the target from the skin and the technical difficulty of using the ultrasound to perform real-time imaging as the block is performed.
The target is to place the needle in the paraspinal area at the level of L3/4. Ultrasound can be used both to confirm the correct vertebral level and to guide the needle tip under direct vision. A low-frequency (2–5 MHz) curved array probe is used. It is placed in a paramedian longitudinal position (Fig. 19). Firm pressure is required to obtain good-quality images. The transverse processes are identified at the L3/4 space by moving the ultrasound probe laterally from the spinous processes in the midline, staying in the longitudinal plane. Going from the midline and moving the probe laterally, the articular processes are seen, with the adjoining superior and inferior articular processes of the facets forming a continuous “sawtooth” hyperechoic line. As the probe is moved further laterally, the transverse processes are seen, with the psoas muscle lying between them. The image is of a “trident” (Fig. 20), with the transverse processes causing bony shadows and the psoas muscle lying in between.

Fig.19 Positioning for ultrasound-guided lumbar plexus block
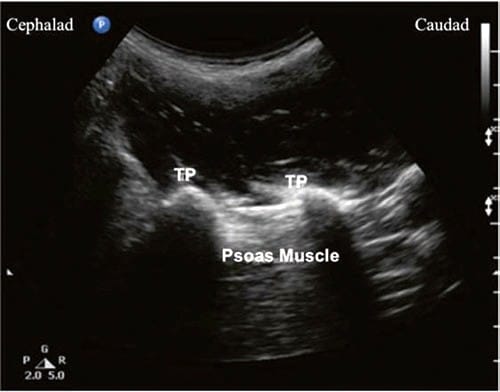
Fig.20 Paravertebral scan of the L3–L4 region using a curved transducer. TP transverse process
At this point, the ultrasound probe is usually 3–5 cm off the midline. The lumbar plexus is not usually directly visualized but lies within the posterior third of the psoas muscle (i.e., the closest third of the psoas muscle seen with the ultrasound probe). The distance from the skin to the psoas muscle can be measured using the caliper function of the ultrasound machine. This gives an estimate of the depth of the lumbar plexus before needle insertion. Note that the peritoneal cavity, the great vessels, and the kidney lie anterior to the psoas muscle (further away from the skin in this ultrasound view). Thus care with needle tip placement should be maintained at all times.
The depth of the plexus is most often between 50 and 100 mm from the skin surface. An in-plane or an out-ofplane technique may be used. If an in-plane approach is used, the usual direction for insertion is from caudad to cephalad. For the out-of-plane approach, the site for the block needle is on the medial side of the ultrasound probe (which is maintained in its longitudinal position). The needle must be placed at the center of the probe, directed slightly laterally so that in its path it comes directly under the ultrasound beam. Advancing the needle from a medial to a lateral direction is also preferred, to avoid insertion into the dural cuff, which can extend laterally beyond the neural foramina. Lidocaine is infiltrated into the skin and subcutaneous tissue at the point where the block needle is to be inserted. The needle is observed in real time and targeted toward the posterior third of the psoas muscle bulk. Electrical stimulation is commonly used to confirm proximity to the lumbar plexus. The target is to elicit quadriceps muscle contraction. When satisfied with the needle tip position, the local anesthetic is injected incrementally (with frequent aspiration to monitor for blood or CSF), and its spread is observed, looking for fluid and tissue expansion in the psoas muscle bulk.
19. OBTURATOR NERVE BLOCK
Clinical Application
The obturator nerve sends articular branches to the hip and knee joints and innervates a relatively small dermatome area on the medial aspect of the knee. The obturator nerve also supplies the adductor muscles on the medial aspect of the thigh. block of the obturator nerve using the “3-in-1” technique is unreliable, and ultrasonography again offers an excellent opportunity for direct visualization and subsequent effective block of that nerve.
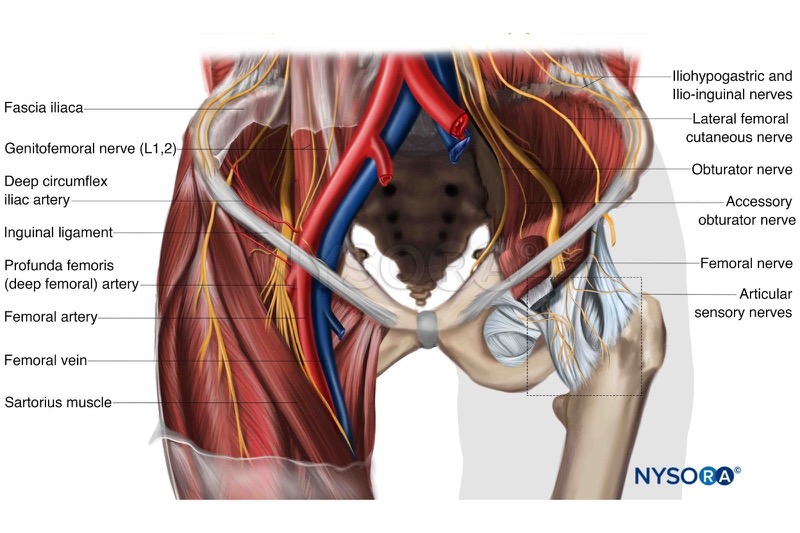
20. ANATOMY
The anterior divisions of L2-4 ventral rami form this nerve. It descends toward the pelvis from the medial border of the psoas major muscle and travels through the obturator canal. Once it emerges from the obturator canal, it enters the medial aspect of the thigh and divides into anterior and posterior divisions, which run anterior and posterior to the adductor brevis. The anterior division supplies the adductor brevis and longus, and the posterior division supplies the knee joint and adductor magnus.
Cognitive aid: Anatomy of the obturator nerve.
For additional information check NYSORA Compendium.
21. PREPARATION AND POSITIONING
Noninvasive monitors are applied and intravenous access obtained. Intravenous sedative agents and oxygen therapy are administered as required. The groin is exposed on the side to be blocked. Slight abduction of the hip and external rotation of the thigh help in improving the probe placement and image optimization. Skin disinfection is then performed and a sterile technique observed.
22. ULTRASOUND TECHNIQUE
A high-frequency (7–12 MHz) linear array probe is appropriate for this block. Ultrasonography is performed just below the inguinal ligament, to see the femoral artery and vein. The probe should be moved medially and slightly caudal, maintaining its horizontal position (Fig. 21). The obturator nerve lies between the pectineus, adductor longus, and short adductor brevis muscles. The anterior branch of the obturator nerve lies in a fascial layer between the pectineus, adductor longus, and adductor brevis muscles. The posterior branch lies between the adductor brevis and the adductor magnus muscles.
Going laterally, the pectineus is identified, and then the adductor muscles. The anterior branch of the obturator nerve can be found between the adductor longus and the (deeper) adductor brevis. The posterior branch is found between the adductor brevis and the (deeper) adductor magnus muscles. In both cases (anterior and posterior), the obturator nerve is often seen as a hyperechoic structure, although sometimes only the fascial planes can be distinguished (Fig. 22).

Fig.21 In-plane approach for the obturator nerve block
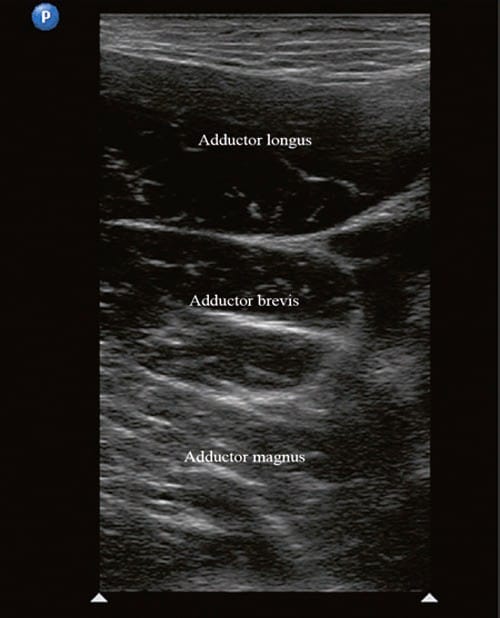
Fig.22 Transverse image of the medial aspect of upper thigh, showing adductor longus, brevis, and magnus muscles
An in-plane or an out-of-plane approach may be used. It is useful to obtain an ultrasound image where both branches are visible, and then choose a single needle insertion point from which both branches of the nerve may be blocked. The skin is infiltrated with lidocaine at this point. When the block needle tip is positioned at the correct site between the fascial planes, local anesthetic solution is injected. The local anesthetic should be observed to cause distension of the intermuscular fascial planes and surround the nerve (if visible).
To aid localization of the obturator nerve, low-current nerve stimulation may be used to elicit adductor muscle contraction. It is possible to perform the block without the use of nerve stimulation and also without exactly identifying the obturator nerve branches themselves [9]. The important steps when using ultrasound guidance are correct identification of the muscle layers and deposition of the local anesthetic into the appropriate interfascial planes.
23. LATERAL FEMORAL CUTANEOUS NERVE BLOCK
Clinical Application
The lateral femoral cutaneous nerve (LFCN) provides sensory innervation to the lateral thigh. block of the LFCN can be used for analgesia for femoral neck surgery in older patients. It can also be used for the diagnosis and management of meralgia paresthetica, a chronic pain syndrome caused by entrapment of the nerve (frequently by adipose layers over the iliac crest) [10]. The LFCN has a highly variable course, so the success rate in blocking this nerve is much higher with ultrasound guidance than with blind approaches [11].
24. ANATOMY
The LFCN is a pure sensory nerve arising from the dorsal divisions of L2/3. After emerging from the lateral border of the psoas major muscle, it follows a highly variable path: it may pass inferior or superior to the anterior superior iliac spine (ASIS) (Fig. 23). If it passes medial to the ASIS, it can be less than 1 cm or more than 7 cm away from it [12]. It is located between the fascia lata and fascia iliaca. It passes under the inguinal ligament and crosses the lateral border of the sartorius muscle at a variable distance (between 2 and 11 cm) inferior to the ASIS, where it divides into anterior and superior branches.
Cognitive aid: Anatomy of the lateral femoral cutaneous nerve.
For additional information check NYSORA Compendium.

Fig.23 In-plane approach for blocking the lateral femoral cutaneous nerve of the thigh
25. PREPARATION AND POSITIONING
The patient is positioned supine with the leg in a neutral position. Noninvasive monitors are applied and intravenous access obtained. The groin is exposed and the ASIS marked. Intravenous sedative agents and oxygen therapy are administered as required. Skin disinfection is then performed over the ASIS/groin area and a sterile technique observed.
26. ULTRASOUND TECHNIQUE
For this superficial technique, a 7–12 MHz high-frequency linear array probe is placed immediately medial to the ASIS along the inguinal ligament, with the lateral end of the probe on the ASIS. The ASIS casts a bony shadow on the ultrasound image. The ultrasound probe is moved medially and inferiorly from this point. An in-plane or out-of-plane approach may be used. The fascia lata, fascia iliaca, and sartorius muscle are identified. The nerve is identified as a small, hypoechoic structure found between the fascias above the sartorius muscle. As it is a superficial structure, an inplane approach is used, with a shallow angle of approach. The skin is infiltrated with lidocaine, and the block needle is inserted to reach the desired skin plane immediately medial and inferior to the ASIS. Using ultrasound guidance, the LFCN can be blocked with a much lower dose of local anesthetic; blockage with as little as 0.3 mL of lidocaine has been reported in the literature [13].
27. SAPHENOUS NERVE BLOCK
Clinical Application
The saphenous nerve is a sensory branch of the femoral nerve. It innervates the skin over the medial, anteromedial, and posteromedial aspects of the lower limb from above the knee to the foot. Thus block of the saphenous nerve produces anesthesia and analgesia of the anteromedial aspect of the lower leg, ankle, and foot, but without producing quadriceps muscle weakness. It is commonly used with a sciatic nerve block to provide complete anesthesia and analgesia of the lower leg. Its small size and lack of a motor component make it difficult to localize with conventional nerve localization techniques, so ultrasound increases the success rate of blocking this nerve [14].

Cognitive aid: Anesthesia distribution of the saphenous nerve block at the adductor canal. Left: dermatomes, middle: myotomes, right: osteotomes.
For additional information check NYSORA Compendium: Saphenous Nerve Block at the Adductor Canal.
28. ANATOMY
The saphenous nerve is a terminal branch of the femoral nerve, leaving the femoral canal proximally in the femoral triangle, descending within the adductor canal, and remaining deep to the sartorius muscle with the superficial femoral artery (Fig. 24). It is initially found lateral to the femoral artery and then becomes more medial and superior to the vessel at the distal end of the adductor magnus muscle [15]. It is a sensory nerve, covering the medial aspect of the calf, ankle, foot, and great toe.
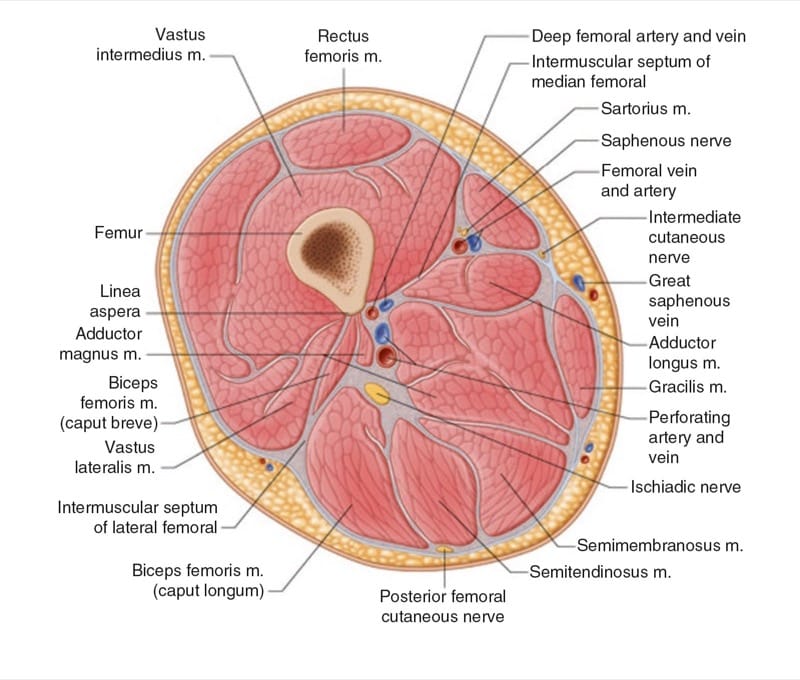
Fig.24 Cross-section of the thigh showing the position of the saphenous nerve
29. PREPARATION AND POSITIONING
The patient is in a supine position, with the leg slightly externally rotated and the knee flexed. Noninvasive monitors are applied and intravenous access obtained. Intravenous sedative agents and oxygen therapy are administered as required. The medial aspect of the thigh is exposed down to the knee. Skin disinfection is then performed here and a sterile technique observed.
30. ULTRASOUND TECHNIQUE
In the mid to distal thigh, the saphenous nerve can be easily approached. The nerve can be blocked with an in-plane approach (Fig. 25) or an out-of-plane approach. A highfrequency (7–12 MHz) linear ultrasound is placed transverse to the longitudinal axis and is used to scan the medial aspect of the thigh. The saphenous nerve is frequently difficult to visualize, but its relationship to the sartorius muscle and vessels is relatively constant. At the medial side of the mid-thigh region (approximately 15 cm proximal to the patella), the sartorius muscle and femoral artery are identified. The saphenous nerve lies in a position below the sartorius muscle. The ultrasound probe is moved in a caudal direction from this point along the long axis of the thigh until the femoral artery is seen “diving” deeper, toward the posterior aspect of the thigh, where it becomes the popliteal artery. This area is the “adductor hiatus.” From here, the ultrasound probe is brought 2–3 cm proximally, to the distal adductor canal, and the saphenous nerve is blocked at this level (Fig. 26).

Fig.25 In-plane approach for saphenous nerve block at the level of the adductor canal
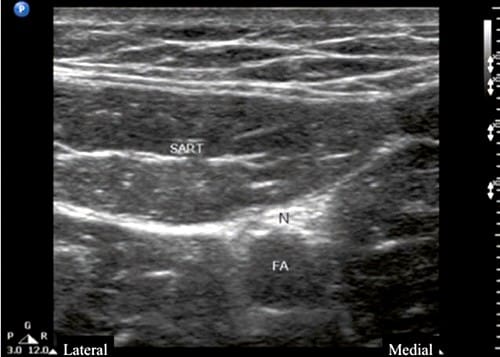
Fig.26 Transverse view showing the saphenous nerve (N) and sartorius muscle (SART). FA femoral artery
Note that the diameter of the saphenous nerve varies widely. The aim is to insert the needle deep to the sartorius and deposit the local anesthetic medial to the artery. More distally in the thigh, 5–7 cm proximal to the popliteal crease, the saphenous nerve is superficial to the descending branch of the femoral artery, deep to the sartorius muscle, and posterior to the vastus medialis muscle.
More distally, the saphenous nerve pierces the fascia lata between the sartorius and gracilis tendons to join the subcutaneous saphenous vein. The saphenous nerve is posteromedial to the vein at the level of the tibial tuberosity, although it is difficult to visualize using ultrasound. Ultrasound-guided paravenous injection of local anesthetic using light pressure with a high-frequency linear transducer probe is easily performed at this level.
31. ANKLE BLOCK
Clinical Application
Ankle block can be used for anesthesia and analgesia of the foot (midfoot and forefoot). It can be used for diagnostic and therapeutic purposes with spastic talipes equinovarus and sympathetically mediated pain. It is useful for postoperative pain relief, as it causes no motor block of the foot; patients can ambulate with crutches immediately after surgery, which facilitates faster discharge home.
32. ANATOMY
Five peripheral nerves innervate the foot area (Fig. 27):
• The saphenous nerve, a terminal branch of the femoral nerve, supplies the medial side of the foot. Branches of the sciatic nerve innervate the remainder of the foot.
• The sural nerve innervates the lateral aspect of the foot. This is formed from the tibial and communicating superficial peroneal branches.
• The posterior tibial nerve supplies the deep plantar structures, the muscles, and the sole of the foot.
• The superficial peroneal nerve innervates the dorsal aspect of the foot.
• The deep peroneal nerve supplies the deep dorsal structures and the web space between the first and second toes.
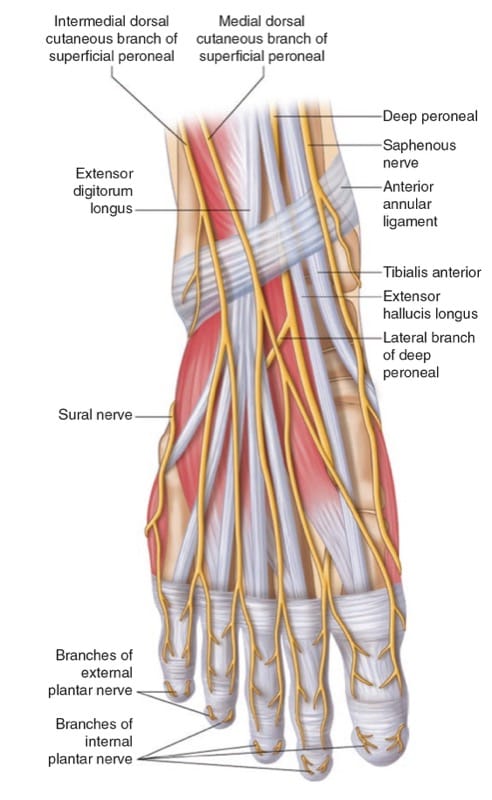
Fig.27 Nerve supply to the ankle
The saphenous, superficial peroneal, and sural nerves lie subcutaneously at the level of the malleoli. The posterior tibial nerve and deep peroneal nerve lie deeper in the tissues: the tibial nerve lies under the flexor retinaculum, and the deep peroneal nerve lies under the extensor retinaculum. The posterior tibial nerve passes with the posterior tibial artery posterior to the medial malleolus. The deep peroneal nerve passes lateral to the anterior tibial artery under the flexor retinaculum before emerging more superficially to travel with the dorsalis pedis artery on the dorsum of the foot.
The exact areas of the foot supplied by each nerve vary significantly in the population. Thus for surgical procedures that require a tourniquet, blockage of all five nerves is required.

Cognitive aid: Sensory distribution of an ankle block.
For additional information check NYSORA Compendium: Ankle Block.
33. PREPARATION AND POSITIONING
The patient is placed supine. Noninvasive monitors are applied and intravenous access obtained. Intravenous sedative agents and oxygen therapy are administered as required. The foot is elevated with a pillow (or similar) such that the anterior and medial aspects of the ankle are accessible. Skin disinfection is then performed and a sterile technique observed.
34. ULTRASOUND TECHNIQUE
block of the Superficial Peroneal, Saphenous, and Sural Nerves
Traditionally, block of the superficial peroneal, saphenous, and sural nerves is performed by infiltration subcutaneously without the use of ultrasound. This is performed by a circumferential subcutaneous injection of 10 to 15 mL of local anesthetic solution over the anterior aspect of the ankle, in a line just proximal to the malleoli. However, a newer technique using ultrasound to locate the sural nerve has been described in the literature. This was performed applying a tourniquet and looking 1 cm proximal to the lateral malleolus for the distended lesser saphenous vein [16]. No attempt is made to identify the sural nerve itself, and the local anesthetic is inserted using an out-of-plane approach to obtain circumferential perivascular spread (usually achieved with less than 5 mL of local anesthetic).
Ultrasound also facilitates block of the posterior tibial and deep peroneal nerves, the two deep nerves that supply the foot.
35. block OF THE POSTERIOR TIBIAL NERVE
A 7–12 MHz linear array ultrasound probe is used, as the structures usually lie within 2–3 cm of the skin. If present on the ultrasound machine, the 10–15 MHz “hockey stick” ultrasound probe also may be used for this block. The probe is placed immediately superior and slightly posterior to the medial malleolus, in the transverse plane. The bony landmark of the medial malleolus is easily identified as a hyperechoic, curvilinear shadow. The tibial arterial pulsation and the hyperechoic tibial nerve are seen posterior and superficial to the medial malleolus. The order of the structures (seen going posteriorly from the medial malleolus) is tendons, then artery, and then nerve (“TAN”).
An in-plane or an out-of-plane approach may be used (Figs.28 and 29). An in-plane approach is most often used, and nerve stimulation can be used to confirm position if required before insertion of local anesthetic. Ultrasound can be used to confirm circumferential spread of local anesthetic around the nerve; 5 mL of local anesthetic is sufficient with the use of this method.

Fig.28 In-plane approach to block the posterior tibial nerve

Fig.29 Out-of-plane approach to block the posterior tibial nerve
36. block OF THE DEEP PERONEAL NERVE
The deep peroneal nerve is not readily visualized using ultrasound. Thus its position is usually inferred by locating the dorsalis pedis artery. The ultrasound probe is placed on the dorsum of the foot at the intermalleolar line. The dorsalis pedis pulsation is identified, and sometimes the deep peroneal nerve is seen as a round, hyperechoic structure lateral to the artery.
The dorsal foot is convex in shape, and the nerve is in a superficial location, making it difficult to use the in-plane approach for this block. Thus the out-of-plane approach is commonly used for needle insertion. Once it is identified, 2–3 mL of local anesthetic is deposited around the deep peroneal nerve. If the nerve is not seen, the local anesthetic can be deposited lateral to the dorsalis pedis artery.
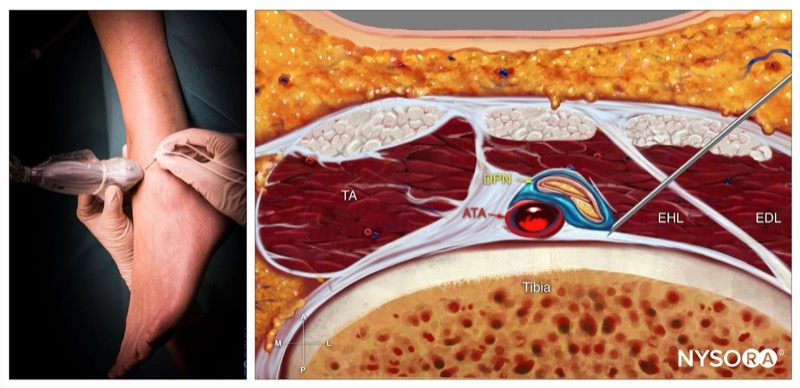
Cognitive aid: Deep peroneal nerve block; Reverse Ultrasound Anatomy with needle insertion in-plane and local anesthetic spread (blue). TA, tibialis anterior muscle; ATA, anterior tibial artery; DPN, deep peroneal nerve; EHL, extensor hallucis longus; EDL, extensor digitorum longus.
For additional information check NYSORA Compendium: Ankle Block.
37. block OF THE PROXIMAL SUPERFICIAL PERONEAL NERVE
Recently, a new approach for ultrasound visualization of the superficial peroneal nerve has been described [17, 18]. With the patient in supine position, the leg is flexed at the knee. Using a high-frequency (7–12 MHz) linear array ultrasound probe, the common peroneal nerve is visualized at the level of the knee, winding around the head of the fibula. The nerve is followed down distally until it divides into the deep and superficial branches. The superficial peroneal nerve can be visualized lying along the fascial plane between the peroneus brevis muscle laterally and the extensor digitorum longus muscle medially. An in-plane technique using a 22 G blunt needle is used to deposit 5 mL of the local anesthetic solution (Figs. 30 and 31).

Fig.30 In-plane approach for ultrasound-guided block of the proximal superficial peroneal nerve
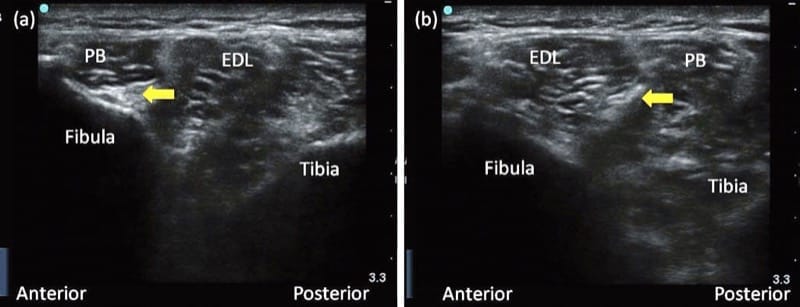
Fig.31 (a, b), Ultrasound images of the superficial peroneal nerve lying between the peroneus brevis muscle laterally and the extensor digitorum longus muscle medially. EDL extensor digitorum longus, PB peroneus brevis