Learning objectives
- Describe the common indications for pituitary surgery
- Manage patients undergoing pituitary surgery
Background
- Pituitary adenomas are common in clinical practice
- Pituitary adenomas can be classified as either functioning or nonfunctioning, depending on whether they are hormone-secreting
- Patients with functioning adenomas frequently present with symptoms of hormone excess
- Patients with nonfunctioning adenomas often present later and have symptoms resulting from the mass effect of the tumor (headache, visual loss due to compression of the optic chiasm, hypopituitarism due to compression of the anterior pituitary)
- Common clinical conditions resulting from pituitary adenomas: Cushing’s disease, acromegaly, prolactin overproduction, panhypopituitarism
- Surgical resection has become the primary therapy when medical therapy fails with transsphenoidal pituitary surgery being the most common technique
- Transsphenoidal pituitary surgery presents unique challenges for anesthesia due to both the endocrine and neurosurgical management
Preoperative assessment
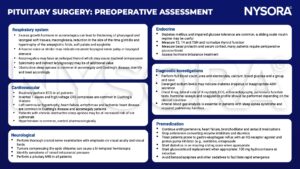
T3, triiodothyronine; T4, thyroxine; TSH, thyroid-stimulating hormone; ADH, antidiuretic hormone
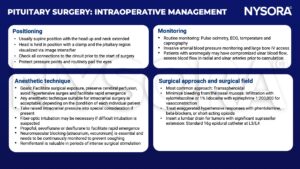
Intraoperative management
Postoperative management
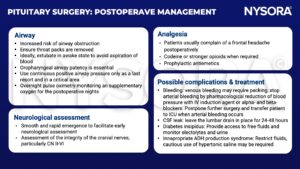
ADH, antidiuretic hormone
Suggested reading
- Dunn LK, Nemergut EC. Anesthesia for transsphenoidal pituitary surgery. Curr Opin Anaesthesiol. 2013;26(5):549-554.
- Griffiths S, Perks A. The Hypothalamic Pituitary Axis Part 2: Anaesthesia For Pituitary Surgery. WFSA. Published July 26, 2010. Accessed January 19, 2023. https://resources.wfsahq.org/atotw/the-hypothalamic-pituitary-axis-part-2-anaesthesia-for-pituitary-surgery/
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com







