Learning objectives
- Describe porphyria
- Recognize the symptoms and signs of porphyria
- Anesthetic management of a patient with porphyria
Definition and mechanisms
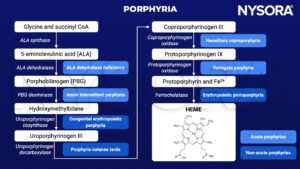
- Porphyrias are a heterogeneous group of inherited genetic disorders of heme biosynthesis
- The heme biosynthetic pathway is most active in the liver and bone marrow
- Porphyrins are organic cyclical compounds found in heme, the iron-containing ring structure found in hemoglobin, myoglobin, and all of the cytochromes
Classification
- Acute porphyrias: Potential to develop acute neurovisceral crises
- Acute intermittent porphyria (AIP)
- Variegate porphyria (VP)
- Hereditary coproporphyria (HCP)
- 5-aminolaevulinic acid (ALA) dehydrase deficiency
- Triggers for an acute crisis
- Fasting
- Dehydration
- Infection
- Drugs
- Endogenous hormones
- Stress
- Smoking
- Alcohol
- Non-acute: Do not deteriorate into acute crises, less relevant for anesthesiologists
- Porphyria cutanea tarda
- Congenital erythropoietic porphyria
- Erythropoietic protoporphyria
Signs and symptoms
Presentation of an acute crisis
- Almost all patients have severe abdominal pain, usually associated with tachycardia
- Symptoms and signs of acute crises vary greatly and can mimic other conditions
| Symptoms and signs | Features | May be misdiagnosed as |
|---|---|---|
| Abdominal pain | Recurrent, severe, poorly localized Associated nausea and vomiting Absence of fever or leucocytosis | Another cause of acute abdomen Endometriosis/pelvic inflammatory disease Irritable bowel syndrome Opiate addiction |
| Cardiovascular signs | Tachycardia Tachyarrhythmia Hypertension | |
| Weakness | Proximal > distal Upper limbs > lower Up to 20% develop respiratory failure May progress to bulbar paresis in severe cases | Guillain-Barré syndrome Poliomyelitis Acute lead poisoning Vasculitis |
| Psychiatric features | Mood disturbance Confusion Psychosis | Anxiety disorder Somatization disorder Acute psychosis Acute confusional state |
| Pain and sensory disturbance | Back, thigh, or extremity pain Sensory neuropathy over the trunk | Chronic fatigue syndrome Fibromyalgia Chronic pain syndromes |
| Seizures | CNS manifestation of porphyria Secondary to hyponatremia | Epilepsy |
| Other autonomic features | Constipation Gastoparesis Postural hypotension | |
| Cutaneous lesions | Only in VP and HCP Vesicular rash Photosensitivity | Porphyria cutanea tarda Bullous skin disease |
| Hyponatremia and other electrolyte disturbance | Low serum sodium Low serum magnesium | Other disorders of sodium and water balance |
Risk factors
- Women are 4 to 5 times more likely to develop crises in their early thirties
Pathophysiology
Treatment
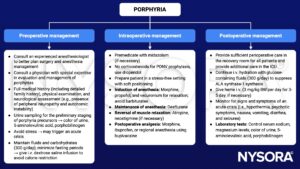
Once an acute crisis has been diagnosed, management consists of the following:
- Remove or treat potential triggering factors and avoid a catabolic state
- Administration of i.v. heme arginate 3 mg/kg daily for 4 days
- Supportive measures
- May require large doses of morphine to control pain
- Antiemetics prochlorperazine and ondansetron are safe
- Control tachycardia and hypertension with β-blockers
- Avoid seizures via correcting hyponatremia and treating with gabapentin, vigabatrin, or levetiracetam
- Sedation with propofol and alfentanil is safe
Management
Commonly used drugs and their safety profile
| Drug | Safe | Unsafe | Undetermined |
|---|---|---|---|
| I.v. anesthetic agents | Propofol | Thiopentone, ketamine | Etomidate |
| Inhalational anesthetic agents | Isoflurane, desflurane, nitrous oxide | Sevoflurane | |
| Local anesthetics | Bupivacaine, prilocaine, lidocaine | Levobupivacaine, ropivacaine | |
| Neuromuscular blocking agents and removal | Succinylcholine, all non-depolarizing muscle relaxants, neostigmine | ||
| Analgesics | Fentanyl, alfentanil, remifentanil, morphine, hydromorphone, meperidine, tramadol, ibuprofen, aspirin | Oxycodone, diclofenac | Pentazocine, mefenamic acid |
| Sedative premedication | Lorazepam, phenothiazines (chlorpromazine), temazepam | ||
| Antibiotics | Gentamicin, co-amoxiclav, penicillins, vancomycin, tazocin, meropenem | Rifampicin, erythromycin | |
| Cardiovascular drugs | Adrenaline, noradrenaline, milrinone, atropine, glycopyrrolate, β-blockers, phenylephrine, magnesium, angiotensin 2 inhibitors, fibrinolytic drugs | Ephedrine | Vasopressin, metaraminol |
| Miscellaneous | Syntocin, carboprost, tranexamic acid, aprotinin | Dexamethasone, hydrocortisone |
Keep in mind
- Anesthesiologists should be aware of the perioperative factors that may trigger or worsen an acute crisis in porphyria
Suggested reading
- Findley H, Philips A, Cole D, Nair A. Porphyrias: implications for anaesthesia, critical care, and pain medicine. Continuing Education in Anaesthesia Critical Care & Pain. 2012;12(3):128-133.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com