Learning objectives
- Describe the posterior fossa
- Describe the indications for posterior fossa surgery
- Manage patients undergoing posterior fossa surgery
Background
- The posterior fossa is the deepest cranial fossa
- Surrounded by:
- Anteriorly: The dorsum sellae and basilar portion of the occipital bone (clivus)
- Laterally: The petrosal and mastoid components of the temporal bone
- Superiorly: The dural layer (tentorium cerebelli), and posteriorly and
- Inferiorly and posteriorly: The occipital bone
- Contains many important structures: the brainstem, cerebellum and lower cranial nerves
- The cerebrospinal fluid pathway is very narrow through the cerebral aqueduct and any obstruction can cause hydrocephalus which can result in a significant increase in intracranial pressure
Pathologies
- Tumors are the most common pathologies of the posterior fossa
- Pathologies which require surgical intervention:
| Tumors | Axial tumors | Medulloblastoma (most common) |
| Cerebellar astrocytoma | ||
| Brainstem glioma | ||
| Ependymoma | ||
| Choroid plexus papilloma | ||
| Dermoid tumours | ||
| Hemangioblastoma | ||
| Metastatic tumours | ||
| Cerebellopontine angle tumours | Schwannoma | |
| Meningioma | ||
| Acoustic neuroma | ||
| Glomus jugulare tumour | ||
| Vascular malformations | Posterior cerebellar artery aneurysm | |
| Vertebral/vertebrobasillar aneurysm | ||
| Basillar tip aneurysm | ||
| AV malformations | ||
| Cerebellar hematoma | ||
| Cerebellar infarction | ||
| Cysts | Epidermoid cyst | |
| Arachnoid cyst | ||
| Cranial nerve lesions | Trigeminal neuralgia (cranial nerve V) | |
| Hemifacial spasm (cranial nerve VII) | ||
| Glossopharyngeal neuralgia (cranial nerve IX) | ||
| Craniocervical abnormalities | Atlanto-occipital instability | Congenital |
| Acquired | ||
| Atlanto-axial instability | Congenital | |
| Acquired | ||
| Arnold–Chiarri malformation |
Management
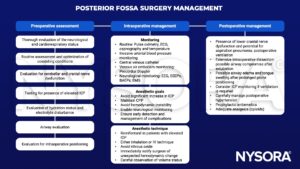
ICP, intracranial pressure; ECG, electrocardiography; EEG, electroencephalography; SSEP, somatosensory evoked potential; BAEP, brainstem auditory evoked potential; EMG, electromyography; CPP, cerebral perfusion pressure
Keep in mind
- Maintain consistent and modest levels of inhalation or IV anesthetic agents to minimize interference during SSEP monitoring
- Avoid neuromuscular blocking agents
- Use total IV anesthesia during motor evoked potential monitoring
- Intraoperative positioning
- The sitting position improves surgical access to the posterior fossa, but is associated with several potential complications:
| Complication | Management |
|---|---|
| Cardiovascular instability | Notify the surgeon of their proximity to vital structures |
| Venous air embolism | Administer high-concentration oxygen, discontinue nitrous oxide, maintain cardiovascular stability, central venous catheter to aspirate air from right atrium, immediate initiation of chest compression in the event of a massive air embolism with cardiac arrest |
| Pneumocephalus | High-flow oxygen, burr hole and aspiration of air in severe cases |
| Macroglossia | Ensure airway clearance |
| Quadriplegia | Avoid this complication by paying close attention to positioning and avoiding prolonged hypotension |
Suggested reading
- Sandhu K, Gupta N. Chapter 14 – Anesthesia for Posterior Fossa Surgery. In: Prabhakar H, editor. Essentials of Neuroanesthesia: Academic Press; 2017. p. 255-76.
- Jagannathan S, Krovvidi H. Anaesthetic considerations for posterior fossa surgery. Continuing Education in Anaesthesia Critical Care & Pain. 2014;14(5):202-6.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com








