Learning objectives
- Describe the mechanisms, risk factors, and symptoms of postoperative nerve injuries
- Diagnose postoperative nerve injuries
- Prevent and manage postoperative nerve injuries
Background
- Postoperative peripheral nerve injuries are complications of both general and regional anesthesia
- Third-most common cause of anesthesia-related medical litigation
- Very rare
- Potentially results in significant morbidity for the patient
Mechanisms
- Direct nerve damage from surgery, needle trauma, or secondary to regional anesthesia or peripheral catheter
- Stretch and compression: Poor padding and positioning of limbs, use of tourniquets and surgical retractors
- Ischemia: Caused primarily by tourniquets, prolonged immobility, hematoma surrounding a nerve, and local anesthetic agents
- Local anesthetic toxicity: High concentrations and prolonged exposure increase risk
- Double crush syndrome: Decreased tolerance of a nerve to compression after previous compression
- Idiopathic
- Combination of mechanisms
Risk factors
| Surgical | Neurosurgery |
| Cardiac surgery | |
| Gastrointestinal surgery | |
| Orthopedic surgery | |
| Patient-specific | Hypertension |
| Diabetes mellitus | |
| Smoking | |
| Double crush syndrome | |
| Preexisting peripheral neuropathy | |
| Anatomical abnormalities | |
| Anesthetic | General anesthesia |
| Epidural anesthesia | |
| Perioperative | Hypovolemia |
| Dehydration | |
| Hypotension | |
| Hypoxia | |
| Electrolyte disturbance | |
| Hypothermia |
Classification
| Seddon | Sunderland | Pathophysiology |
|---|---|---|
| Neuropraxia (compression) | Type 1 | Local myelin damage with the nerve still intact |
| Axonotmesis (crush) | Type 2 | Continuity of axons is lost Endoneurium, perineurium, and epineurium remain intact Loss of continuity of axons with Wallerian degeneration due to disruption of axoplasmic flow |
| Type 3 | Type 2 with endoneurial injury | |
| Type 4 | Type 2 with endoneurial and perineurial injury but an intact epineurium | |
| Neurotmesis (transection) | Type 5 | Complete physiological disruption of the entire nerve trunk Early surgical intervention necessary Prognosis guarded |
Symptoms
- Sensory
- Anesthesia
- Paresthesia
- Hypoesthesia
- Hyperesthesia
- Pain in the areas supplied by the affected nerves
- Motor
- Paresis
- Paralysis
- Autonomic dysfunction
- Trophic changes
Upper extremity nerve injuries
| Affected nerve(s) | Mechanism of injury | Clinical presentation |
|---|---|---|
| Ulnar nerve | Direct pressure on the ulnar groove Prolonged forearm flexion | Tingling or numbness along the little finger Weakness of abduction/adduction of the fingers |
| Brachial plexus | Compression, stretching, or direct injury resulting from a regional technique | C5-6 lesion: Arm hangs by side, medially rotated and pronated C8-T1 lesion: Claw hand and numbness in the ulnar distribution |
| Radial nerve | Tourniquet/arterial pressure cuffs Compression against a patient screen Arm board at incorrect height | Wrist drop Numbness along posterior surface of the lower arm and a variable area of the dorsum of the hand and lateral fingers |
| Median nerve | Direct nerve damage from regional techniques Invasive procedures around the elbow Compression in the carpal tunnel | Paresthesia along the palmar aspect of the lateral fingers Weakness of abduction and opposition of the thumb Weak wirst flexion Forearm kept in supination Hand appears flattened |
| Axillary (C5-6) and musculocutaneous nerve (C5-7) | Shoulder surgery or shoulder dislocation | Weakness of shoulder abduction and anesthesia along upper lateral border of the arm (axillary nerve) Weakness of elbow flexion and numbness along the lateral border of the forearm (musculocutaneous nerve) |
Lower extremity nerve injuries
| Affected nerve | Mechanism of injury | Clinical presentation |
|---|---|---|
| Sciatic nerve (L4-S3) | Stretch, compression, ischemia, direct damage Lithotomy, frog leg, and sitting positions Regional techniques | Paralysis of the hamstring muscles and all the muscles below the knee Weak knee flexion and foot drop Impaired sensation below the knee except the medial aspect of the leg and foot |
| Femoral nerve (L2-4) | Compression at the pelvic brim by retractors Ischemia associated with aortic cross-clamp Lithotomy position Invasive procedures to access the femoral vessels Hip arthroplasty | Loss of sensation at the front of the thigh and medial aspect of the leg Weak hip flexion Loss of knee extension Decreased or absent knee jerk reflex |
| Superficial peroneal nerve (L4-5, S1-2) | Lithotomy Lateral position | Loss of dorsiflexion and eversion of the foot Loss of sensation along the anterolateral border of the leg and dorsum of the digits except those supplied by the saphenous and sural nerves |
Diagnosis
- Thorough history and clinical examination to localize the lesion and identify preexisting peripheral neuropathy
- Electromyography
- Nerve conduction studies
- Imaging: MRI, high-resolution ultrasound
- Early consultation with a neurologist
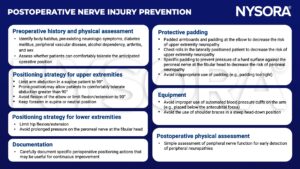
Prevention
Management
- Correct underlying pathology and alleviate symptoms
- Consult neurology
- Surgical correction is rarely indicated
- Physiotherapy
- Orthotic measures (foot care, splints, and limb supports)
Suggested reading
- Hewson DW, Bedforth NM, Hardman JG. Peripheral nerve injury arising in anaesthesia practice. Anaesthesia. 2018;73(S1):51-60.
- Chui J, Murkin JM, Posner KL, Domino KB. Perioperative Peripheral Nerve Injury After General Anesthesia: A Qualitative Systematic Review. Anesth Analg. 2018;127(1):134-143.
- Practice Advisory for the Prevention of Perioperative Peripheral Neuropathies 2018: An Updated Report by the American Society of Anesthesiologists Task Force on Prevention of Perioperative Peripheral Neuropathies*. Anesthesiology. 2018;128(1):11-26.
- Lalkhen AG, Bhatia K. Perioperative peripheral nerve injuries. Continuing Education in Anaesthesia Critical Care & Pain. 2012;12(1):38-42.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com



