Learning objectives
- Defining, diagnosing, and treating pulmonary embolism
Definition
- A pulmonary embolism (PE) is a blood clot that blocks blood flow to an artery in the lung
- Most often the blood clot originates in a deep leg vein and moves through the venous circulation to the heart
- Severe PE is an immediately life-threatening situation
- Low cardiac output and a ventilation/perfusion mismatch contribute to hypoxemia
- Right ventricular failure due to acute pressure overload is considered the primary cause of death in severe PE
Risk factors
Predisposing factors for venous thromboembolism (VTE) are:
| Strong (OR > 10) | Moderate (OR 2–9) | Weak risk factors (OR < 2) |
|---|---|---|
| Fracture of the lower limb Hospitalization for heart failure or atrial fibrillation/flutter ≤ 3 months Hip or knee replacement Major trauma Myocardial infarction ≤ 3 months Previous VTE spinal cord injury | Arthroscopic knee surgery Autoimmune diseases Blood transfusion CVCs IVs Chemotherapy Congestive heart failure Respiratory failure Erythropoiesis-stimulating agents IVF Oral contraceptive therapy Postpartum period Infection IBD Cancer Paralytic stroke Superficial vein thrombosis Thrombophilia | Bed rest > 3 days Diabetes mellitus Arterial hypertension Immobility due to sitting (e.g. prolonged car or air travel) Increasing age Laparoscopic surgery Obesity Pregnancy Varicose veins |
Symptoms
Symptoms of PE are aspecific and can include:
| Respiratory | Dyspnea Hemoptysis Hypoxemia Hypocapnia Chest pain |
| Cerebral | Syncope |
| Cardiac | Hemodynamic instability ECG might show sinus tachycardia, S1Q3T3 pattern, incomplete or complete right bundle branch block (usually in more severe cases), or atrial arrhythmias |
Diagnosis
- Diagnostic scores like the pulmonary embolism rule-out Criteria (PERC) can help to determine whether further investigations for PE are warranted
- D-dimers have a high negative predictive value, meaning that a normal D-dimer level renders acute PE or DVT unlikely
- The positive predictive value of elevated D-dimer levels is low, meaning it isn’t useful as a test to confirm PE
- Use age-adjusted D-dimers (age x 10 µg/l) for patients aged >50 years
- Computed tomographic pulmonary angiography (CTPA) is the gold standard for diagnosing PE

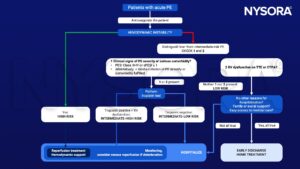
Management
- The pulmonary embolism severity Index (PESI) reliably identifies patients with a low risk for 30-day mortality
- Administer supplemental oxygen to patients with PE and SaO2 <90%
- Initiate mechanical ventilation if necessary and start with non-invasive techniques if possible
- Treat right heart failure in hemodynamically unstable patients with PE
- Fluids
- Vasopressors
- Mechanical circulatory support
- Anticoagulant patients with a high or intermediate clinical probability of PE while awaiting diagnostic test results
- Low-molecular-weight heparin (LMWH) and fondaparinux are preferred over unfractionated heparin UFH for initial anticoagulation in PE
- Administer UFH in patients with overt hemodynamic instability and patients with renal impairment (≤ G4)
- When using vitamin K antagonists:
- Continue anticoagulation with UFH, LMWH, or fondaparinux in parallel with the oral anticoagulant for ≥ 5 days
- Until the INR has been 2.0–3.0 for 2 consecutive days
- Start thrombolysis in patients with high-risk PE
- Perform a thrombectomy if thrombolysis is contraindicated or has failed in patients
Suggested reading
- Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543-603.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com