Learning objectives
- Describe the electrolyte and acid-base abnormalities associated with pyloric stenosis
- Explain why these electrolyte and acid-base abnormalities need to be corrected preoperatively
- Anesthetic management of a pediatric patient with pyloric stenosis
Definition and mechanisms
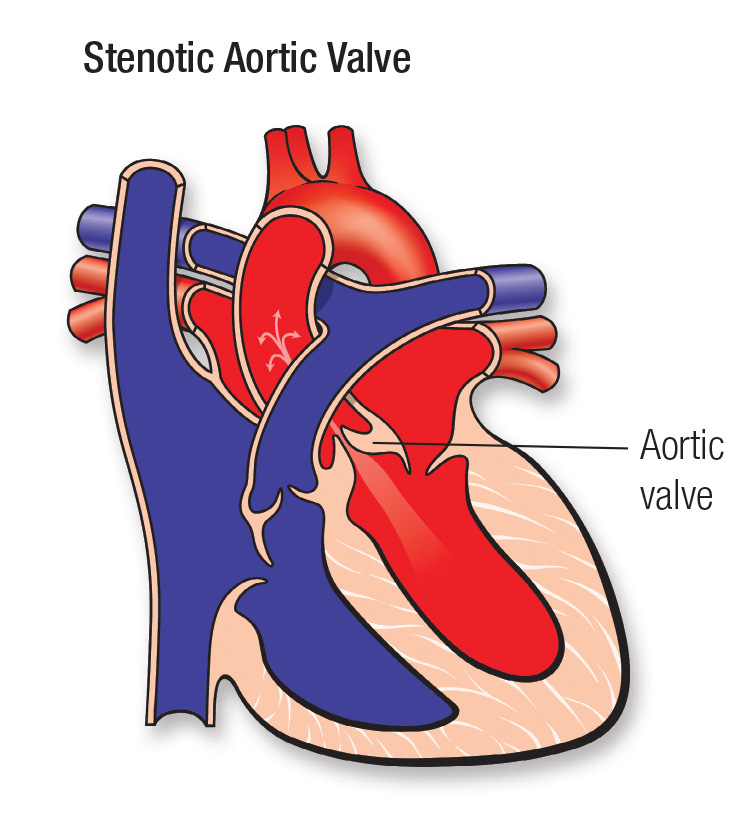
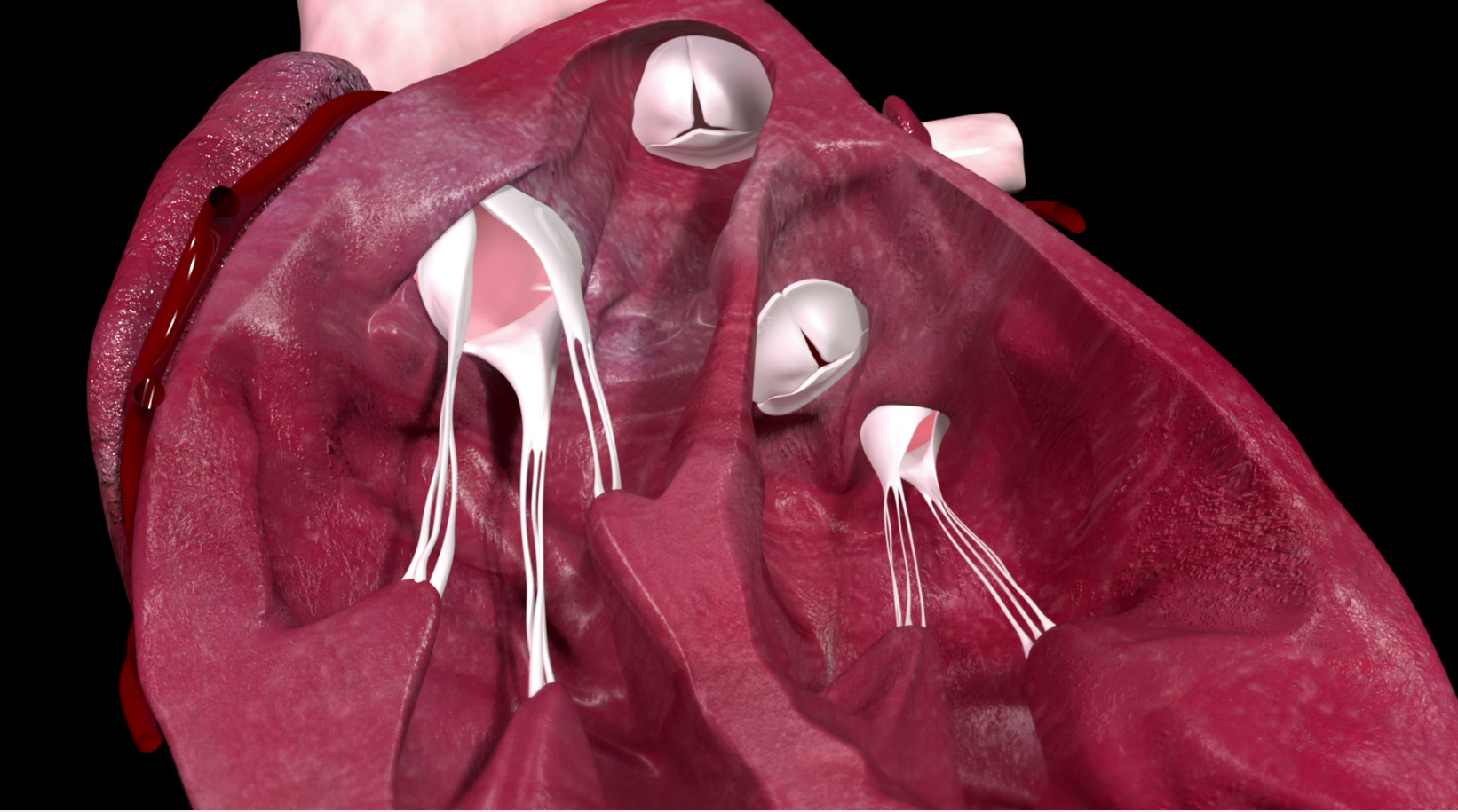
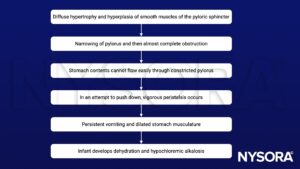
- Pyloric stenosis, or infantile hypertrophic pyloric stenosis, is an uncommon condition in infants characterized by abnormal thickening of the pylorus muscles in the stomach, leading to gastric outlet obstruction
- Typically seen between 2 and 12 weeks of age, patients present with projectile vomiting after feedings, dehydration, and failure to thrive
- The danger of pyloric stenosis comes from the dehydration and electrolyte disturbance rather than the underlying problem itself → infant has to be stabilized by correcting the dehydration and hypochloremic alkalosis with IV fluids
Signs and symptoms
- Symptoms usually appear within 3-5 weeks after birth
- Bile-free projectile vomiting after every feeding
- Persistent hunger
- Stomach contractions (visible peristalsis in the left upper quadrant from left to right)
- Changes in bowel movements
- Weight problems
Complications
- Failure to grow and develop, failure to thrive
- Dehydration, hypovolemia
- Metabolic alkalosis
- Electrolyte abnormalities (hypochloremia, hyponatremia, hypokalemia)
- Stomach irritation
- Jaundice
Risk factors
- First-born male children
- Preterm birth
- Cesarean section
- Family history
- Smoking during pregnancy
- Bottle feeding
- Early antibiotic use (e.g., erythromycin to treat whooping cough)
- White and Hispanic children
Pathophysiology
Treatment
- Correction of dehydration and hypochloremic alkalosis before surgery with IV fluids → accomplished within 24-48 hours
- Surgery: Pyloromyotomy
Management
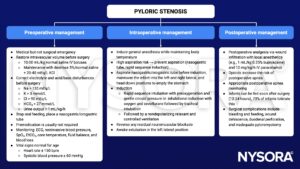
Keep in mind
- Vomiting associated with pyloric stenosis results in hypochloremia, hyponatremia, hypokalemia, metabolic alkalosis, and dehydration, all of which have to be corrected before general anesthesia and surgery
- Empty the stomach using a nasogastric or orogastric tube before induction of anesthesia
- Ensure an adequate depth of anesthesia with a complete neuromuscular block before laryngoscopy to minimize the risk of regurgitation and pulmonary aspiration
Suggested reading
- Craig R, Deeley A. Anaesthesia for pyloromyotomy. BJA Educ. 2018;18(6):173-177.
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 24 Paediatrics, Lomas B.
- Houck PJ. PYLORIC STENOSIS. In: Houck PJ, Haché M, Sun LS. eds. Handbook of Pediatric Anesthesia. McGraw Hill; 2015. Accessed February 14, 2023. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=1189§ionid=70363285
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com