Arthur Atchabahian, Catherine Vandepitte, Ana M. Lopez, and Jui-An Lin
FACTS
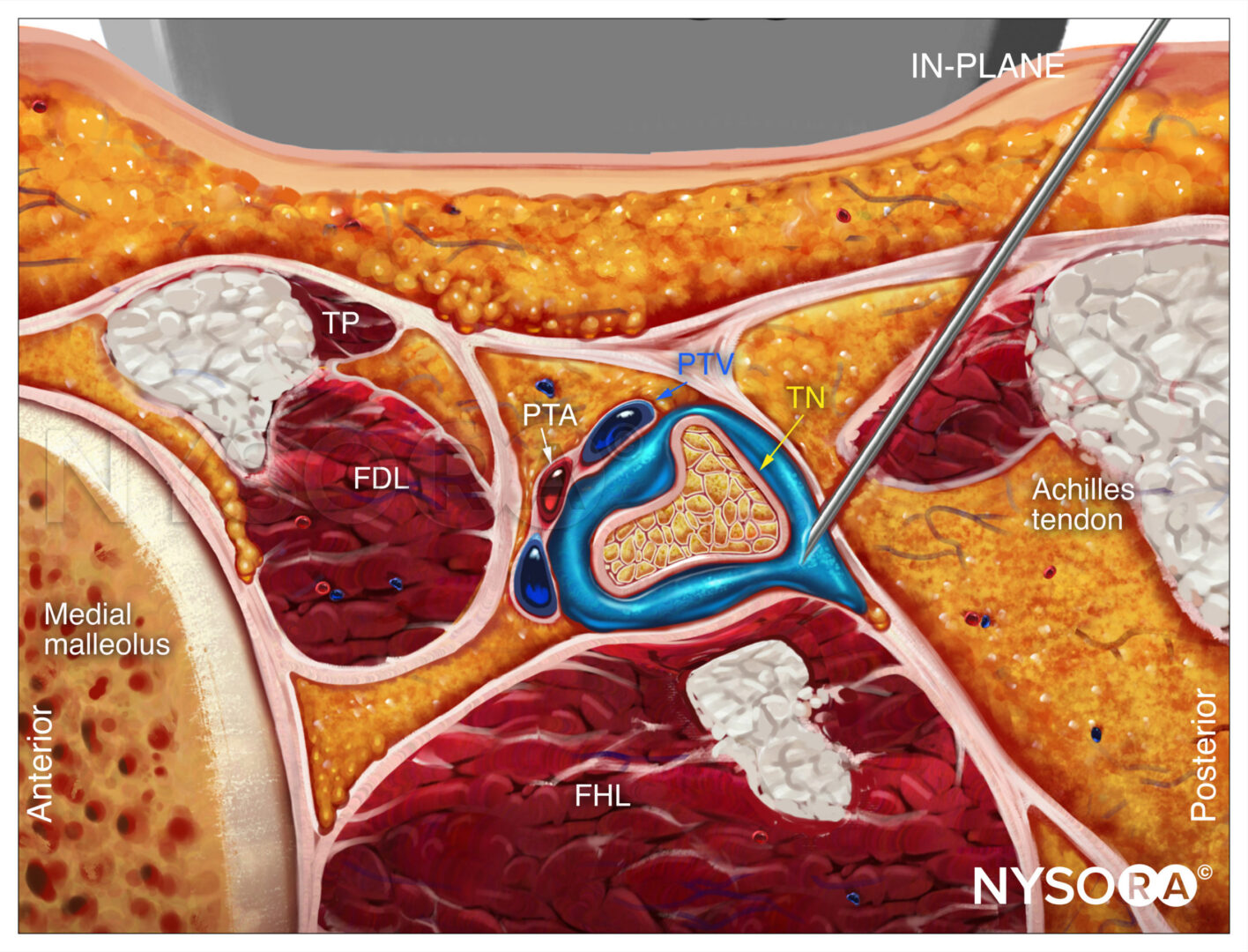
- Indications: foot and ankle surgery, below-knee amputation, analgesia following knee surgery involving the posterior compartment (Figure 1)
- Transducer position:
- Anterior approach: transverse on the proximal medial thigh
- Transgluteal approach: transverse on the posterior buttock, between the ischial tuberosity and greater trochanter
- Subgluteal approach: transverse on the gluteal crease
- Other approaches (eg, parasacral, lateral) have been described but will not be detailed here.
- Goal: local anesthetic spread within the sciatic nerve sheath
- Local anesthetic: 10–20 mL
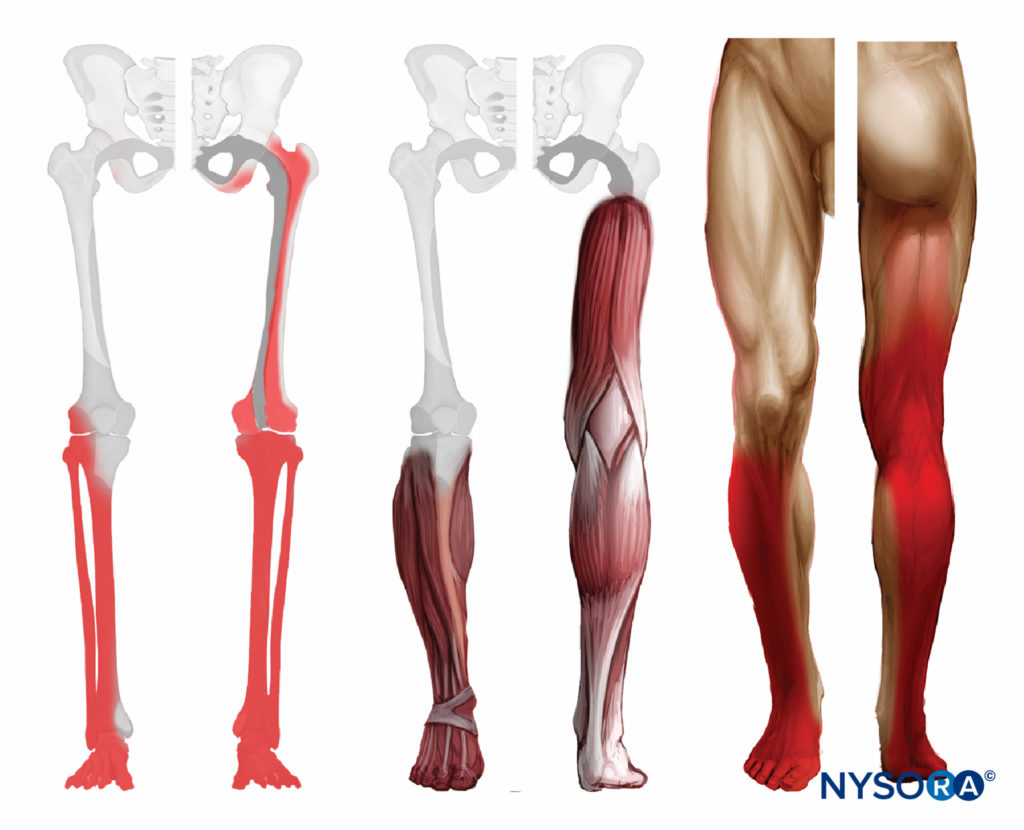
FIGURE 1. Distribution of sensory and motor after sciatic nerve block at gluteal and subgluteal level.
PART I: ANTERIOR APPROACH
GENERAL CONSIDERATIONS
The anterior approach to the sciatic nerve block can be useful in patients who cannot be positioned in the lateral position due to pain, trauma, the presence of external fixation devices that interfere with positioning, or other issues. The ultrasound (US)-guided approach may reduce the risk of femoral artery puncture compared with the landmark-based approach.
The actual scanning and needle insertion are performed on the anteromedial aspect of the proximal thigh, rather than the anterior surface, and may require a slight abduction and external rotation of the thigh. This block is not well-suited to catheter insertion because a large needle must traverse several muscles (discomfort during procedure and risk of hematoma), it is an awkward catheter location (medial thigh), and catheter insertion at an approximately perpendicular angle to the sciatic nerve is difficult.
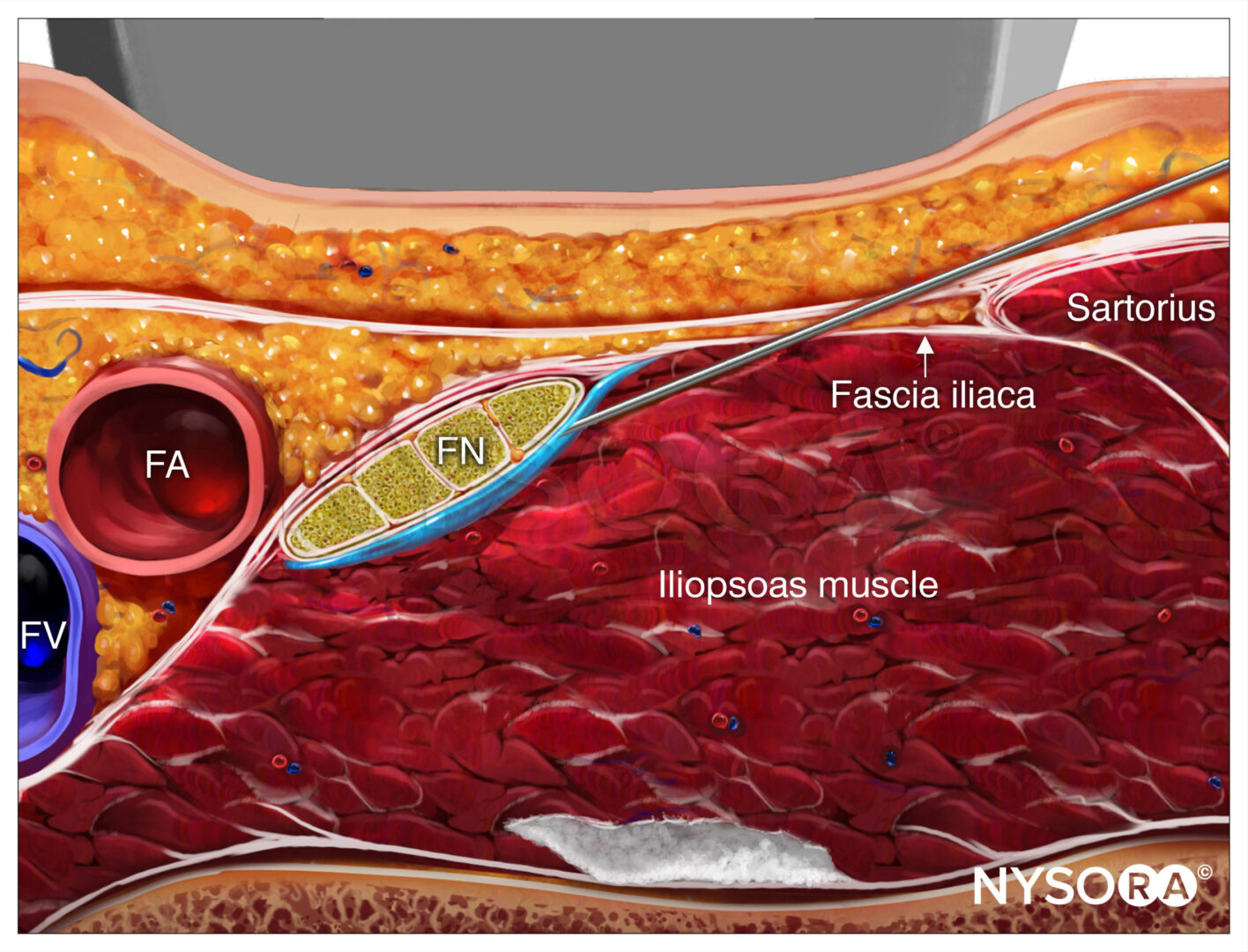
ULTRASOUND ANATOMY
The sciatic nerve is imaged approximately at the level of the minor trochanter. At this location, a curved transducer placed over the anteromedial aspect of the thigh will reveal the musculature of all three fascial compartments of the thigh: anterior, medial, and posterior (Figures 2 and 3). Beneath the sartorius muscle is the femoral artery, and deep and medial to this vessel is the deep artery of the thigh. Both can be identified with color Doppler US for orientation. The femur is seen as a hyperechoic rim with a corresponding shadow beneath the vastus intermedius.
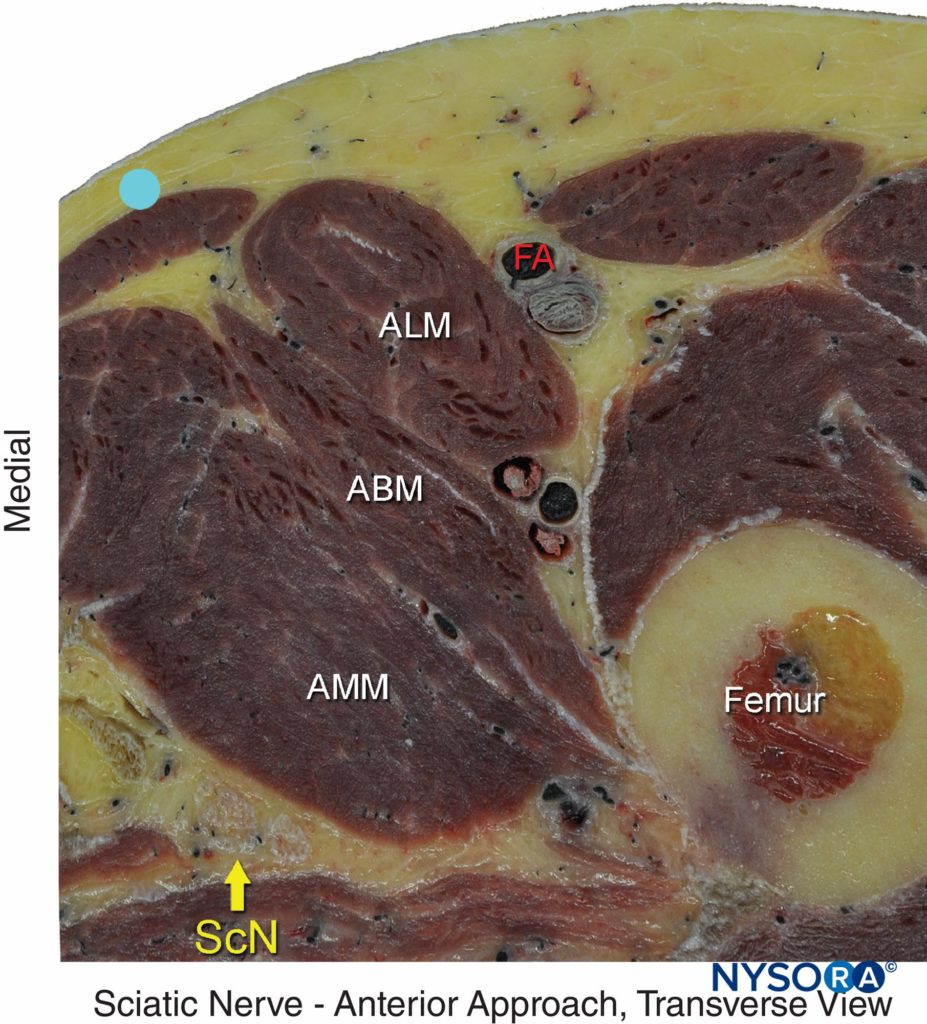
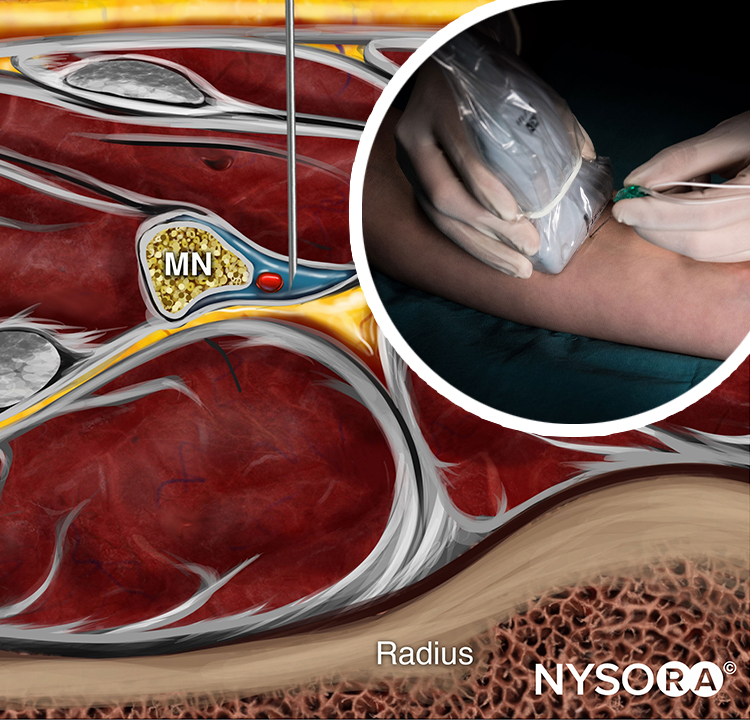
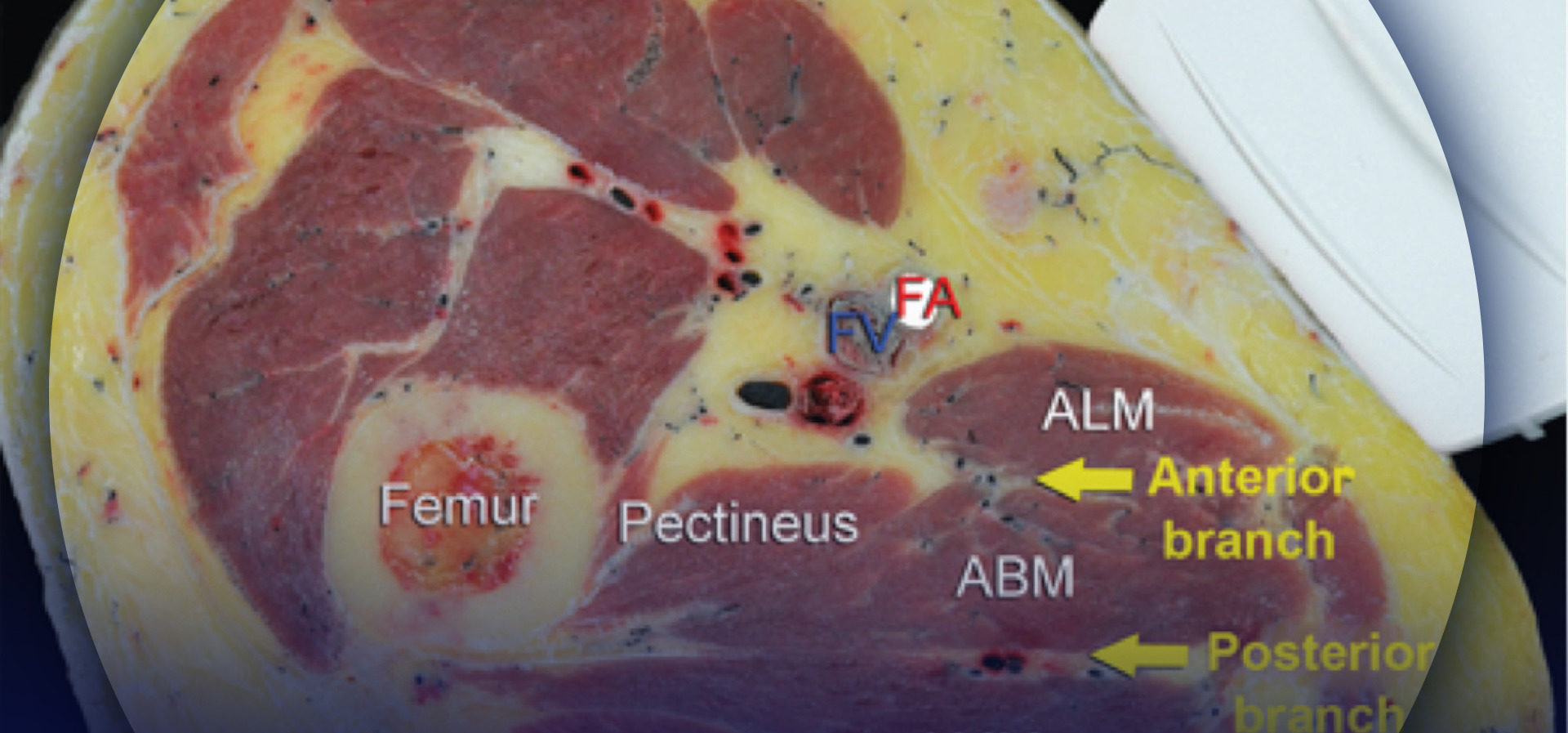
FIGURE 2. Cross-sectional anatomy of the sciatic nerve (ScN). Shown are the femoral artery (FA), adductor longus muscle (ALM), adductor magnus muscle (AMM), adductor brevis muscle (ABM), and femur. The sciatic nerve is seen posterior to
the AMM.
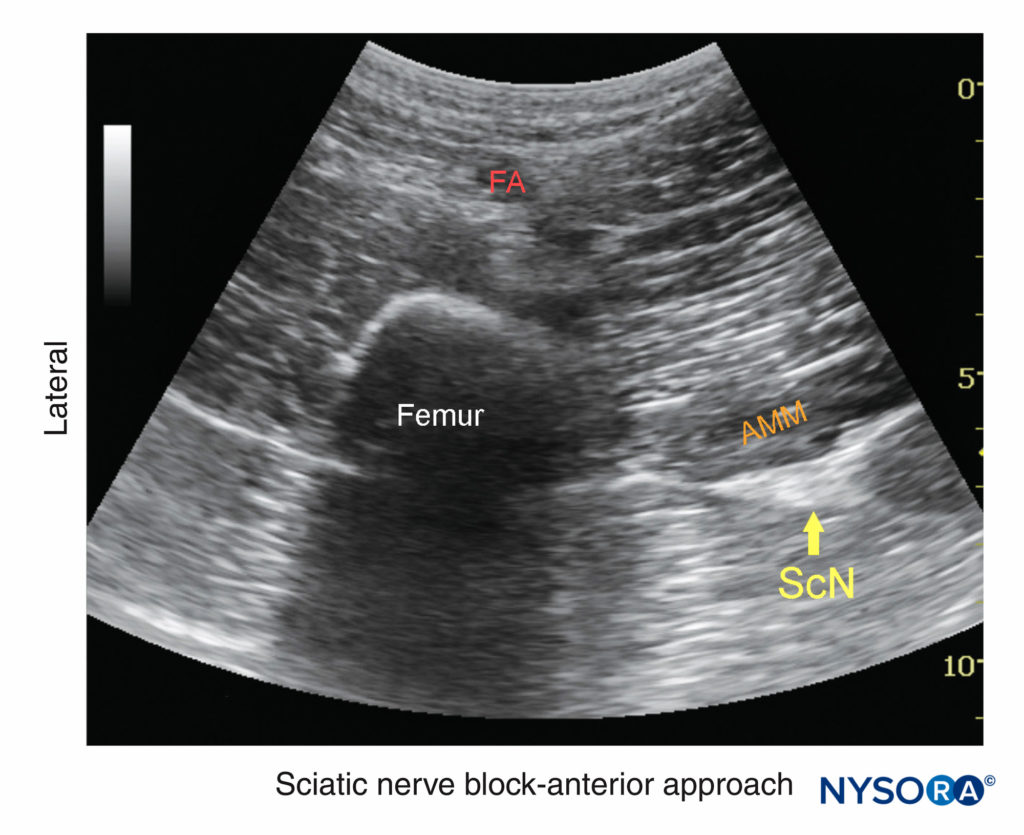
FIGURE 3. Ultrasound anatomy of the sciatic nerve. From superficial to deep, visualized laterally: femoral artery (FA), femur, adductor magnus muscle (AMM), and sciatic nerve (ScN) laterally. The sciatic nerve is typically located at a depth of 6–8 cm. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
Medial to the femur is the adductor magnus muscle, anterior to the hamstring muscles. The sciatic nerve is visualized as a hyperechoic oval structure sandwiched between these two muscle. The nerve is typically visualized at a depth of 6–8 cm (see Figure 3).
For a more comprehensive review of the sciatic nerve distribution, see Functional Regional Anesthesia Anatomy
DISTRIBUTION OF ANESTHESIA
The sciatic nerve block results in anesthesia of the posterior aspect of the knee, hamstring muscles, and entire lower limb below the knee, both motor and sensory block, with the exception of skin on the medial leg and foot (supplied by the saphenous nerve) (Figure 1). The skin of the posterior aspect of the thigh is supplied by the posterior femoro cutaneous nerve, which deviates away from in the sciatic nerve proximal to the level of the anterior approach, and is therefore not blocked. Unless the surgical incision involves the posterior thigh, the lack of anesthesia in its distribution is of little clinical consequence, as pain caused by a thigh tourniquet, for example, is due more to muscle ischemia than to pressure on the skin.
EQUIPMENT
The equipment recommended for a sciatic nerve block using the anterior approach is as follows:
- Ultrasound machine with curved (phased array) transducer (2–8 MHz), sterile sleeve, and gel
- Standard nerve block tray
- One 20-mL syringe containing local anesthetic
- A 100- or 120-mm, 21-gauge, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Sterile gloves
- Injection pressure monitor
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
The anterior approach to the sciatic nerve block is performed with the patient in the supine position. The hip is abducted to facilitate transducer and needle placement (Figures 4 and 5). When feasible, the hip and knee should be somewhat flexed to facilitate exposure. If nerve stimulation is to be used at the same time (this is recommended), exposure of the calf and foot are required to observe motor responses. In either case, it is useful to expose the entire thigh to appreciate the distance from the groin to the knee.

FIGURE 4. Transducer position to visualize the sciatic nerve using the anterior approach. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
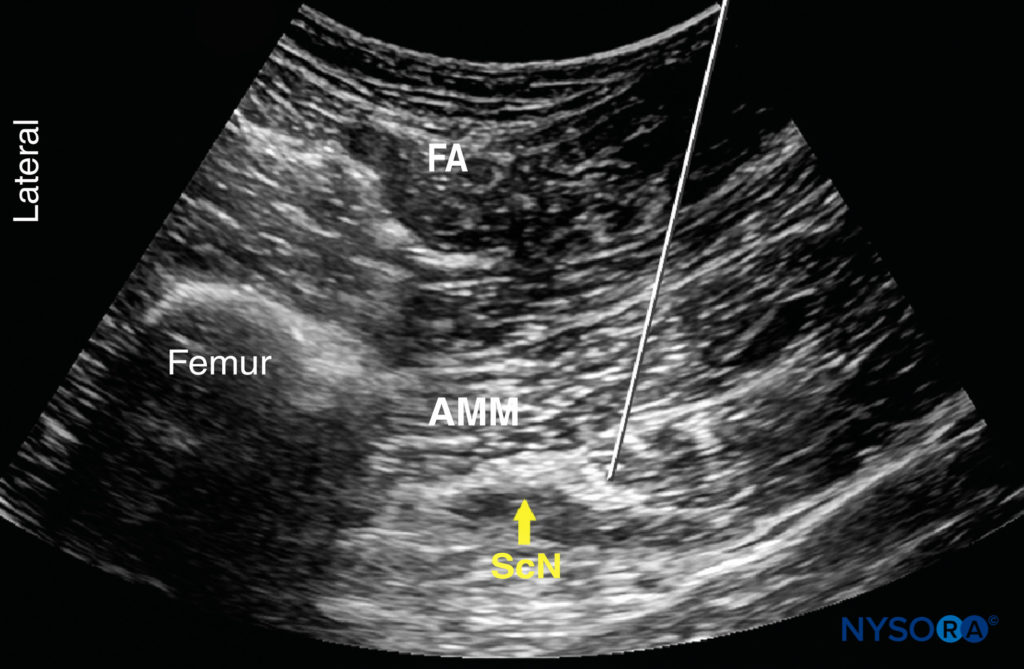
FIGURE 5. Simulated needle path using an out-of-plane technique to reach the sciatic nerve (ScN) using the anterior approach. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
GOAL
The goal is to place the needle tip immediately adjacent to the sciatic nerve, between the adductor magnus muscle and biceps femoris muscle.
TECHNIQUE
With the patient in the proper position, the skin is disinfected and the transducer positioned to identify the sciatic nerve. If the nerve is not immediately apparent, sliding and tilting the transducer proximally or distally can be useful to improve the contrast and bring the nerve “out of the background” from the musculature. If the patient is able to dorsiflex and/or plantar flex the ankle, this maneuver often causes the nerve to move within the intermuscular plane, facilitating identification. The needle is inserted in plane from the medial aspect of the thigh, or out of plane, and advanced toward the sciatic nerve (see Figure 5).
An in-plane approach may prove less practical due to the steep angle of the needle and the use of a curved (nonlinear) probe. If nerve stimulation is used (1.0 mA, 0.1 msec), the contact of the needle tip with the sciatic nerve is usually associated with a motor response of the calf or foot. Once the needle tip is in the proper position, 1–2 mL of local anesthetic is injected to confirm the adequate distribution of injectate. Such injection helps delineate the sciatic nerve within its muscular tunnel, and it should displace the sciatic nerve away from the needle. An improper spread of local anesthetic or nerve displacement may require an adjustment of the needle tip position.
In an adult patient, 10–15 mL of local anesthetic is usually adequate for successful block (Figure 6). Although a single injection of such volume of local anesthetic suffices, it may be beneficial to inject two to three smaller aliquots at different locations to ensure the spread of local anesthetic around the sciatic nerve.
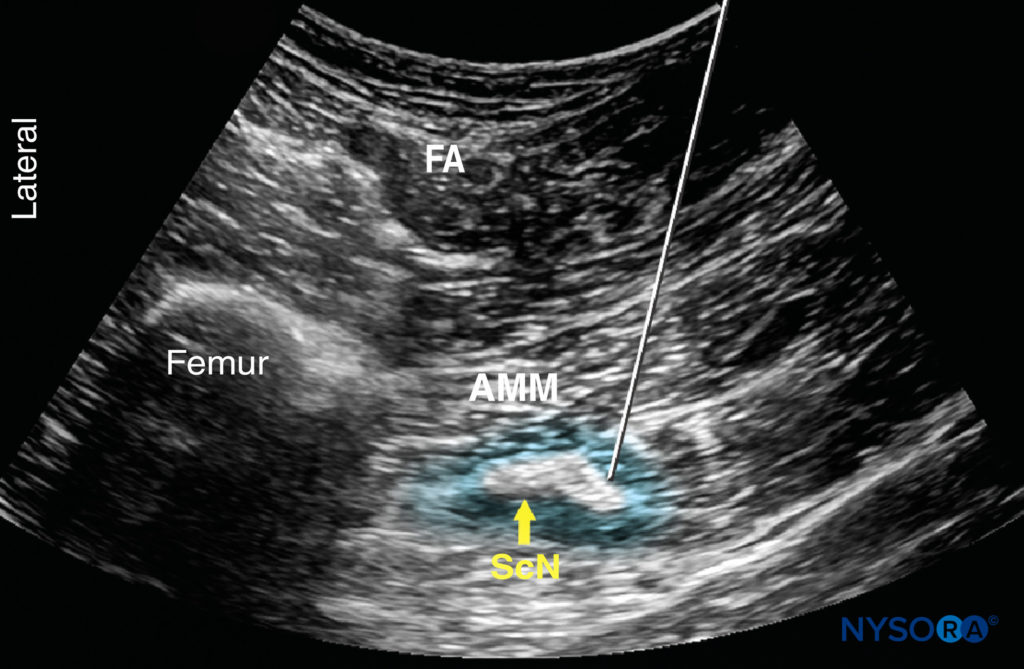
FIGURE 6. Simulated needle path (1) using an out-of-plane technique with proper local anesthetic distribution (blue-shaded area) to anesthetize the sciatic nerve (ScN). (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
The block dynamics and perioperative management are similar to those described in the nerve stimulator technique section.
NYSORA Tips
• Insertion of the needle in an out-of-plane manner using hydro-dissection is often a more practical way to accomplish this block compared to an in-plane approach.
Continue reading Ultrasound-Guided Popliteal Sciatic Block.
SUGGESTED READINGS
- Bruhn J, van Geffen GJ, Gielen MJ, Scheffer GJ: Visualization of the course of the sciatic nerve in adult volunteers by ultrasonography. Acta Anaesthesiol Scand 2008;52:1298–1302.
- Chan VW, Nova H, Abbas S, McCartney CJ, Perlas A, Xu DQ: Ultrasound examination and localization of the sciatic nerve: a volunteer study. Anesthesiology 2006;104:309–314.
- Chantzi C, Saranteas T, Zogogiannis J, Alevizou N, Dimitriou V: Ultrasound examination of the sciatic nerve at the anterior thigh in obese patients. Acta Anaesthesiol Scand 2007;51:132.
- Danelli G, Ghisi D, Ortu A: Ultrasound and regional anesthesia technique: are there really ultrasound guidance technical limits in sciatic nerve blocks? Reg Anesth Pain Med 2008;33:281–282.
- Dolan J: Ultrasound-guided anterior sciatic nerve block in the proximal thigh: an in-plane approach improving the needle view and respecting fascial planes. Br J Anaesth 2013;110:319–320.
- Domingo-Triado V, Selfa S, Martinez F, et al: Ultrasound guidance for lateral midfemoral sciatic nerve block: a prospective, comparative, randomized study. Anesth Analg 2007;104:1270–1274.
- Fredrickson MJ, Kilfoyle DH: Neurological complication analysis of 1000 ultrasound guided peripheral nerve blocks for elective orthopaedic surgery: a prospective study. Anaesthesia 2009;64:836–844.
- Gnaho A, Eyrieux S, Gentili M: Cardiac arrest during an ultrasound-guided sciatic nerve block combined with nerve stimulation. Reg Anesth Pain Med 2009;34:278.
- Gray AT, Collins AB, Schafhalter-Zoppoth I: Sciatic nerve block in a child: a sonographic approach. Anesth Analg 2003;97:1300–1302.
- Hamilton PD, Pearce CJ, Pinney SJ, Calder JD: Sciatic nerve block: a survey of orthopaedic foot and ankle specialists in North America and the United Kingdom. Foot Ankle Int 2009;30:1196–1201.
- Latzke D, Marhofer P, Zeitlinger M, et al: Minimal local anaesthetic volumes for sciatic nerve block: evaluation of ED 99 in volunteers. Br J Anaesth 2010;104:239–244.
- Oberndorfer U, Marhofer P, Bosenberg A, et al: Ultrasonographic guidance for sciatic and femoral nerve blocks in children. Br J Anaesth 2007;98: 797–801.
- Ota J, Sakura S, Hara K, Saito Y: Ultrasound-guided anterior approach to sciatic nerve block: a comparison with the posterior approach. Anesth Analg 2009;108:660–665.
- Panhuizen IF, Snoeck MM. van de Blokkade N: Ischiadicus via echogeleide anterieure benadering [Ultrasound-guided anterior approach to sciatic nerve block]. Ned Tijdschr Geneeskd 2011;155:A2372.
- Pham Dang C, Gourand D: Ultrasound imaging of the sciatic nerve in the lateral midfemoral approach. Reg Anesth Pain Med 2009;34:281–282.
- Saranteas T: Limitations in ultrasound imaging techniques in anesthesia: obesity and muscle atrophy? Anesth Analg 2009;109:993–994.
- Saranteas T, Chantzi C, Paraskeuopoulos T, et al: Imaging in anesthesia: the role of 4 MHz to 7 MHz sector array ultrasound probe in the identification of the sciatic nerve at different anatomic locations. Reg Anesth Pain Med 2007;32:537–538.
- Saranteas T, Chantzi C, Zogogiannis J, et al: Lateral sciatic nerve examination and localization at the mid-femoral level: an imaging study with ultrasound. Acta Anaesthesiol Scand 2007;51:387–388.
- Saranteas T, Kostopanagiotou G, Paraskeuopoulos T, Vamvasakis E, Chantzi C, Anagnostopoulou S: Ultrasound examination of the sciatic nerve at two different locations in the lateral thigh: a new approach of identification validated by anatomic preparation. Acta Anaesthesiol Scand 2007; 51:780–781.
- Sites BD, Neal JM, Chan V: Ultrasound in regional anesthesia: where should the “focus” be set? Reg Anesth Pain Med 2009;34:531–533.
- Tsui BC, Dillane D, Pillay J, Ramji AK, Walji AH: Cadaveric ultrasound imaging for training in ultrasound-guided peripheral nerve blocks: lower extremity. Can J Anaesth 2007;54:475–480.
- Tsui BC, Ozelsel TJ: Ultrasound-guided anterior sciatic nerve block using a longitudinal approach: “expanding the view.” Reg Anesth Pain Med 2008;33:275–276.
- van Geffen GJ, Bruhn J, Gielen M: Ultrasound-guided continuous sciatic nerve blocks in two children with venous malformations in the lower limb. Can J Anaesth 2007;54:952–953.
PART II: POSTERIOR APPROACH
GENERAL CONSIDERATIONS
With the transgluteal approach, the sciatic nerve is approached deep to the gluteus maximus muscle, where it is identified between two osseous landmarks (the ischial tuberosity and the greater trochanter). To obtain view of the sciatic nerve and the osseous structures at this level, the curvilinear probe is typically needed.
With the subgluteal approach, the nerve is just below the level of the gluteal crease where the nerve lies more superficial and can be imaged even with a linear probe. The preference of one approach over the other is based on the patient’s anatomical characteristics and the operator’s personal preference. The subgluteal approach may be a better choice for most patients and indications, including the obese patients.
ULTRASOUND ANATOMY
At the transgluteal level, the sciatic nerve is visualized in the short axis between the two hyperechoic bony prominences of the ischial tuberosity and the greater trochanter of the femur (Figures 7 and 8). The gluteus maximus muscle is seen as the most superficial muscular layer bridging the two osseous structures, typically several centimeters thick. The sciatic nerve is located immediately deep to the gluteus maximus muscle and superficial to the quadratus femoris muscle. Often, it is slightly closer to the ischial tuberosity than to the greater trochanter. At this location in the thigh, it is seen as an oval or roughly triangular hyperechoic structure. At the subgluteal level, the sciatic nerve is positioned between the long head of the biceps femoris muscle and the posterior surface of the adductor magnus.
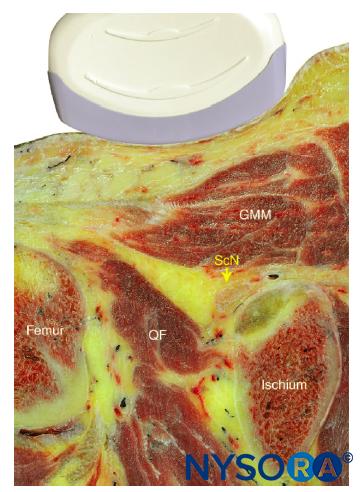
FIGURE 7. Cross-sectional anatomy of the sciatic nerve at the transgluteal level. The sciatic nerve (ScN) is seen between the greater trochanter of the femur and the ischial tuberosity, just deep to the gluteus maximus (GMM) and superficial to the quadratus fermoris (QF) muscles. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
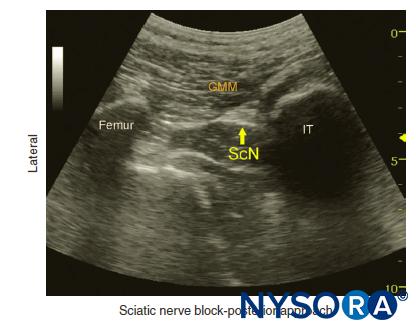
FIGURE 8. Ultrasound image demonstrating the sonoanatomy of the sciatic nerve (ScN). The ScN often assumes an ovoid or triangular shape and is positioned deep to the gluteus maximus muscle (GMM) between the ischial tuberosity (IT) and femur. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
DISTRIBUTION OF ANESTHESIA
Sciatic nerve block results in anesthesia of the entire lower limb below the knee (both motor and sensory block), with the exception of the skin on the medial leg and foot, which is innervated by the saphenous nerve. Both the transgluteal and subgluteal approaches provide motor block of the hamstring muscles. The skin of the posterior aspect of the thigh, supplied by the posterior femorocutaneous nerve, is not by the subgluteal, and when indicated, the posterior femoro cutaneous nerve can be anesthetized separately. For a more comprehensive review of the sciatic nerve distribution, see Functional Regional Anesthesia Anatomy.
EQUIPMENT
The equipment recommended for a sciatic nerve block using the transgluteal or subgluteal approach is as follows:
- Ultrasound machine with curved (phase array) transducer (2–8 MHz), sterile sleeve, and gel
- Standard nerve block tray
- One 20-mL syringe containing local anesthetic
- A 100-mm, 21- to 22-gauge, short-bevel, insulated stimulating needle
- Peripheral nerve stimulator
- Sterile gloves
Clinical Pearl
• Although a linear transducer occasionally can be used for smaller-size patients undergoing transgluteal approach, a curved transducer permits the operator to visualize a wider field, including the osseous landmarks. The ischial tuberosity and greater trochanter are not seen in the same image when using a linear transducer.
Learn more about Equipment for Peripheral Nerve Blocks
LANDMARKS AND PATIENT POSITIONING
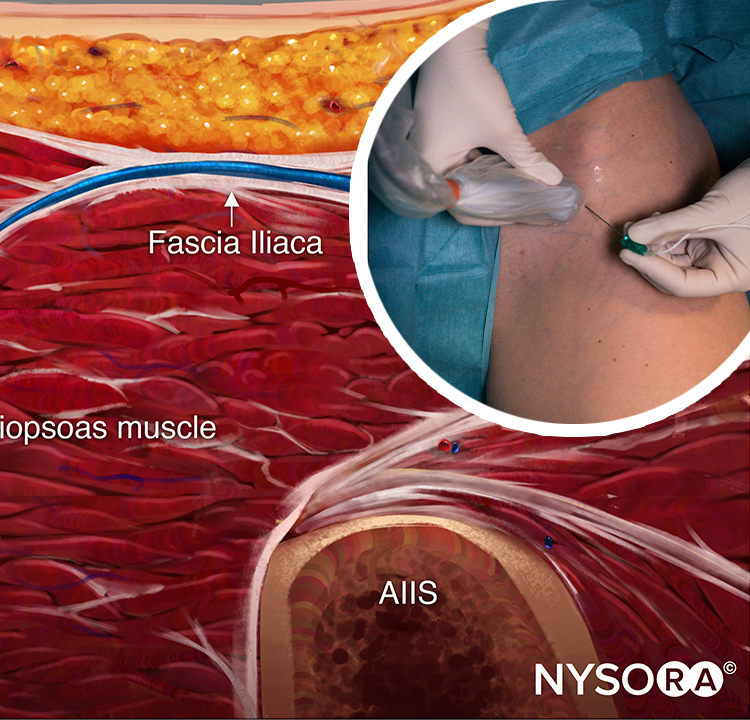
For either the transgluteal or subgluteal approach, the patient is placed in a lateral decubitus position (Figures 9 and 10). The limbs are flexed at the hip and knee. When nerve stimulation is used simultaneously (recommended), exposure of the hamstrings, calf, and foot is required to detect and interpret motor responses.

FIGURE 9. Transducer position and needle insertion for subgluteal approach to sciatic nerve block.

FIGURE 10. Transgluteal approach to sciatic block: patient position, transducer (curved) placement, and needle insertion. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
The osseous prominences of the greater trochanter and ischial tuberosity are palpated and, if desired, marked with a skin marker. The initial transducer position is in the depression between the two bony structures.
GOAL
The goal is to place the needle tip adjacent to the sciatic nerve, deep to the gluteus maximus muscle (the transgluteal technique) and to deposit 15–20 mL of local anesthetic until adequate spread adjacent to the nerve is visualized.
TECHNIQUE
The description of the technique in this chapter will focus primarily on the transgluteal approach. However, since the subgluteal approach is performed just a few centimeters more distally and is technically simpler to perform, the block can be accomplished using either approach by following the general guidelines provided here and by referring to Figure 9 and Figure 11.
The skin is disinfected and the transducer is positioned to identify the sciatic nerve (see Figure 10). Tilting the transducer proximally or distally can help improve the contrast and bring the nerve “out of the background” of the musculature. Often, the nerve is better imaged after the injection of local anesthetic. Alternatively, sliding the transducer slightly proximal or distal can improve the quality of the image and allow for better visualization.
Once identified, the needle is inserted in plane, typically from the lateral aspect of the transducer, and advanced toward the sciatic nerve. If nerve stimulation is used (1.0 mA, 0.1 msec), the passage of the needle through the fascia on the anterior aspect of the gluteus maximus muscle often is associated with a motor response of the calf or foot.
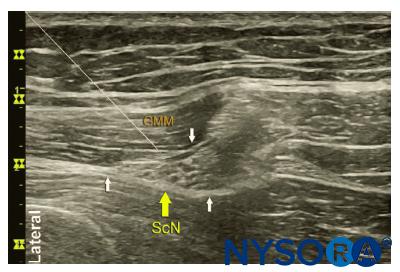
FIGURE 11. The sciatic nerve (ScN) as seen in the subgluteal position (using a linear transducer) and simulated needle path to the interfacial plane (white arrows) between the gluteus maximus muscle (GMM) and the adductor magnus. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
Once the needle tip is positioned adjacent to the nerve (Figure 12), and after careful aspiration to rule out an intravascular needle placement, 1–2 mL of local anesthetic is injected to visualize the proper injection site. Such injection often displaces the sciatic nerve away from the needle; therefore, an additional advancement of the needle 1–2 mm toward the nerve may be necessary to ensure proper local anesthetic spread. Additional needle repositions and injections may be necessary. Ensuring the absence of high resistance to injection to reduce the risk of intrafascicular injection is of utmost importance because the needle tip is difficult to visualize due to the steep angle and depth of the needle placement.
Although a single injection of 15-20 mL of local anesthetic typically suffices, it may be beneficial to inject two to three smaller aliquots at different locations to ensure the spread of local anesthetic solution around the sciatic nerve.
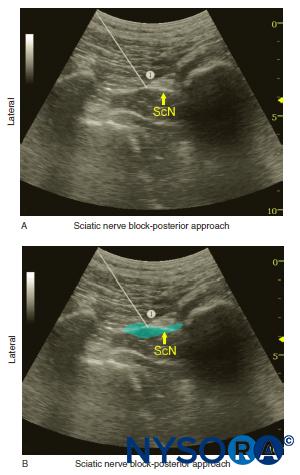
FIGURE 12. (a) Simulated needle path (1) to reach the sciatic nerve (ScN) using an in-plane technique and transgluteal approach. The needle is shown passing through the gluteus muscle with its tip positioned at the lateral aspect of the sciatic nerve. (b) Simulated needle path (1) and local anesthetic distribution (blueshaded area) to block the ScN with the transgluteal approach. (Reproduced with permission from Hadzic A: Hadzic’s Peripheral Nerve Blocks and Anatomy for Ultrasound-Guided Regional Anesthesia, 2nd ed. New York: McGraw-Hill, 2011.)
TIPS
• Never inject against high resistance (> 15 psi) because this may signal an intraneural injection. Even experts may miss signs of intraneural injection.
• While some authors have suggested that intraneural injection is safe for the sciatic nerve, given the high proportion of connective tissue relative to the fascicles, it is best avoided since reliable block can be obtained by injecting around the nerve. The ability to distinguish the sciatic nerve from its soft tissue surroundings often is improved after the injection of local anesthetic; doing so can be used as a marker to identify the nerve when injection begins.
CONTINUOUS ULTRASOUND-GUIDED SUBGLUTEAL SCIATIC BLOCK
The goal of the continuous sciatic nerve block is similar to that of the non–US-based techniques: to place the catheter within the vicinity of the sciatic nerve between the gluteus maximus and quadratus femoris muscles. The procedure is similar to the previously described in the continuous ultrasound-guided block section in Ultrasound-Guided Cervical Plexus Block.
Advancement of the needle in plane in a lateral-to-medial direction until the tip is adjacent to the nerve and deep to the gluteus maximus fascia should ensure appropriate catheter location. Proper placement of the needle also can be confirmed by obtaining a motor response of the calf or foot, at which point 4–5 mL of local anesthetic is injected. This small dose of local anesthetic serves to ensure adequate local anesthetic distribution as well as to make the catheter advancement easier. This first phase of the procedure does not significantly differ from the single-injection technique.
Alternatively, the catheter can be inserted using a longitudinal view. With this approach, after successful imaging of the sciatic nerve in the cross-sectional view, the transducer is rotated 90 degrees so that the sciatic nerve is visualized in the longitudinal view. However, this approach requires significantly greater US imaging skills.
The catheter is secured by either taping it to the skin or tunneling. A common infusion strategy consists of ropivacaine 0.2% at a rate of 5 mL/minute with a patient-controlled bolus of 5 mL/h.
Follow the link for additional information about Continuous Peripheral Nerve Blocks
REFERENCES
- Abdallah FW, Chan VW, Koshkin A, Abbas S, Brull R: Ultrasoundguided sciatic nerve block in overweight and obese patients: a randomized comparison of performance time between the infragluteal and subgluteal space techniques. Reg Anesth Pain Med 2013;38:547–552.
- Meng S, Lieba-Samal D, Reissig LF, et al: High-resolution ultrasound of the posterior femoral cutaneous nerve: visualization and initial experience with patients. Skeletal Radiol 2015;44:1421–1426.
- Krediet AC, Moayeri N, Bleys RL, Groen GJ: Intraneural or extraneural: diagnostic accuracy of ultrasound assessment for localizing low-volume injection. Reg Anesth Pain Med 2014;39:409–413.
- Hara K, Sakura S, Yokokawa N, Tadenuma S: Incidence and effects of unintentional intraneural injection during ultrasound-guided subgluteal sciatic nerve block. Reg Anesth Pain Med 2012;37:289–293.
- Sala-Blanch X, López AM, Pomés J, Valls-Sole J, García AI, Hadzic A: No clinical or electrophysiologic evidence of nerve injury after intraneural injection during sciatic popliteal block. Anesthesiology 2011;115: 589–595.
- Abbas S, Brull R: Ultrasound-guided sciatic nerve block: description of a new approach at the subgluteal space. Br J Anaesth 2007;99:445–446.
- Abdallah FW, Brull R: Is sciatic nerve block advantageous when combined with femoral nerve block for postoperative analgesia following total knee arthroplasty? A systematic review. Reg Anesth Pain Med 2011;36: 493–498.
- Abdallah FW, Brull R: Sciatic nerve block for analgesia after total knee arthroplasty: the jury is still out. Reg Anesth Pain Med 2012;37: 122–123.
- Abdallah FW, Chan VW, Gandhi R, Koshkin A, Abbas S, Brull R: The analgesic effects of proximal, distal, or no sciatic nerve block on posterior knee pain after total knee arthroplasty: a double-blind placebo-controlled randomized trial. Anesthesiology 2014;121:1302–1310.
- Barrington MJ, Lai SL, Briggs CA, Ivanusic JJ, Gledhill SR: Ultrasound-guided midthigh sciatic nerve block—a clinical and anatomical study. Reg Anesth Pain Med 2008;33:369–376.
- Benzon HT, Katz JA, Benzon HA, Iqbal MS: Piriformis syndrome: anatomic considerations, a new injection technique, and a review of the literature. Anesthesiology 2003;98:1442–1448.
- Bruhn J, Moayeri N, Groen GJ, et al: Soft tissue landmark for ultrasound identification of the sciatic nerve in the infragluteal region: the tendon of the long head of the biceps femoris muscle. Acta Anaesthesiol Scand 2009;53:921–925.
- Bruhn J, van Geffen GJ, Gielen MJ, Scheffer GJ: Visualization of the course of the sciatic nerve in adult volunteers by ultrasonography. Acta Anaesthesiol Scand 2008;52:1298–1302.
- Cao X, Zhao X, Xu J, Liu Z, Li Q: Ultrasound-guided technology versus neurostimulation for sciatic nerve block: a meta-analysis. Int J Clin Exp Med 2015;8:273–80.
- Chan VW, Nova H, Abbas S, McCartney CJ, Perlas A, Xu DQ:. Ultrasound examination and localization of the sciatic nerve: a volunteer study. Anesthesiology 2006;104:309–314.
- Chantzi C, Saranteas T, Zogogiannis J, Alevizou N, Dimitriou V: Ultrasound examination of the sciatic nerve at the anterior thigh in obese patients. Acta Anaesthesiol Scand 2007;51:132.
- Danelli G, Ghisi D, Fanelli A, et al: The effects of ultrasound guidance and neurostimulation on the minimum effective anesthetic volume of mepivacaine 1.5% required to block the sciatic nerve using the subgluteal approach. Anesth Analg 2009;109:1674–1678.
- Danelli G, Ghisi D, Ortu A: Ultrasound and regional anesthesia technique: are there really ultrasound guidance technical limits in sciatic nerve blocks? Reg Anesth Pain Med 2008;33:281–282.
- Dillow JM, Rosett RL, Petersen TR, Vagh FS, Hruschka JA, Lam NC: Ultrasound-guided parasacral approach to the sciatic nerve block in children. Paediatr Anaesth 2013;23:1042–1047.
- Domingo-Triado V, Selfa S, Martinez F, et al: Ultrasound guidance for lateral midfemoral sciatic nerve block: a prospective, comparative, randomized study. Anesth Analg 2007;104:1270–1274.
- Fredrickson MJ, Kilfoyle DH: Neurological complication analysis of 1000 ultrasound guided peripheral nerve blocks for elective orthopaedic surgery: a prospective study. Anaesthesia 2009;64:836–844.
- Gnaho A, Eyrieux S, Gentili M: Cardiac arrest during an ultrasound-guided sciatic nerve block combined with nerve stimulation. Reg Anesth Pain Med 2009;34:278.
- Gray AT, Collins AB, Schafhalter-Zoppoth I: Sciatic nerve block in a child: a sonographic approach. Anesth Analg 2003;97:1300–1302.
- Hamilton PD, Pearce CJ, Pinney SJ, Calder JD: Sciatic nerve block: a survey of orthopaedic foot and ankle specialists in North America and the United Kingdom. Foot Ankle Int 2009;30:1196–1201.
- Hara K, Sakura S, Yokokawa N: The role of electrical stimulation in ultrasound-guided subgluteal sciatic nerve block: a retrospective study on how response pattern and minimal evoked current affect the resultant block. J Anesth 2014;28:524–531.
- Karmakar MK, Kwok WH, Ho AM, Tsang K, Chui PT, Gin T: Ultrasoundguided sciatic nerve block: description of a new approach at the subgluteal space. Br J Anaesth 2007;98:390–395.
- Keplinger M, Marhofer P, Marhofer D, et al: Effective local anaesthetic volumes for sciatic nerve block: a clinical evaluation of the ED99. Anaesthesia 2015;70:585–590.
- Krediet AC, Moayeri N, Bleys RL, Groen GJ: Intraneural or extraneural: diagnostic accuracy of ultrasound assessment for localizing low-volume injection. Reg Anesth Pain Med 2014;39:409–413.
- Latzke D, Marhofer P, Zeitlinger M, et al: Minimal local anaesthetic volumes for sciatic nerve block: evaluation of ED 99 in volunteers. Br J Anaesth 2010;104:239–244.
- Marhofer P, Harrop-Griffiths W, Willschke H, Kirchmair L: Fifteen years of ultrasound guidance in regional anaesthesia: Part 2—recent developments in block techniques. Br J Anaesth 2010;104:673–683.
- Meng S, Lieba-Samal D, Reissig LF, et al: High-resolution ultrasound of the posterior femoral cutaneous nerve: visualization and initial experience with patients. Skeletal Radiol 2015;44:1421–1426.
- Moayeri N, van Geffen GJ, Bruhn J, Chan VW, Groen GJ: Correlation among ultrasound, cross-sectional anatomy, and histology of the sciatic nerve: a review. Reg Anesth Pain Med 2010;35:442–449.
- Murray JM, Derbyshire S, Shields MO: Lower limb blocks. Anaesthesia 2010;65(Suppl 1):57–66.
- Oberndorfer U, Marhofer P, Bosenberg A, et al: Ultrasonographic guidance for sciatic and femoral nerve blocks in children. Br J Anaesth 2007;98: 797–801.
- Osaka Y, Kashiwagi M, Nagatsuka Y, Miwa S: Ultrasound-guided medial midthigh approach to sciatic nerve block with a patient in a supine position. J Anesth 2011;25:621–624.
- Ota J, Sakura S, Hara K, Saito Y: Ultrasound-guided anterior approach to sciatic nerve block: a comparison with the posterior approach. Anesth Analg 2009;108:660–665.
- Pham Dang C, Gourand D: Ultrasound imaging of the sciatic nerve in the lateral midfemoral approach. Reg Anesth Pain Med 2009;34: 281–282.
- Ponde V, Desai AP, Shah D: Comparison of success rate of ultrasound-guided sciatic and femoral nerve block and neurostimulation in children with arthrogryposis multiplex congenita: a randomized clinical trial. Paediatr Anaesth 2013;23:74–78.
- Quah VY, Hocking G, Froehlich K: Influence of leg position on the depth and sonographic appearance of the sciatic nerve in volunteers. Anaesth Intensive Care 2010;38:1034–1037.
- Reinoso-Barbero F, Saavedra B, Segura-Grau E, Llamas A: Anatomical comparison of sciatic nerves between adults and newborns: clinical implications for ultrasound guided block. J Anat 2014;224:108–112.
- Salinas FV: Ultrasound and review of evidence for lower extremity peripheral nerve blocks. Reg Anesth Pain Med 2010;35:S16–25.
- Saranteas T: Limitations in ultrasound imaging techniques in anesthesia: obesity and muscle atrophy? Anesth Analg 2009;109:993–994.
- Saranteas T, Chantzi C, Paraskeuopoulos T, et al: Imaging in anesthesia: the role of 4 MHz to 7 MHz sector array ultrasound probe in the identification of the sciatic nerve at different anatomic locations. Reg Anesth Pain Med 2007;32:537–538.
- Saranteas T, Chantzi C, Zogogiannis J, et al: Lateral sciatic nerve examination and localization at the mid-femoral level: an imaging study with ultrasound. Acta Anaesthesiol Scand 2007;51:387–388.
- Saranteas T, Kostopanagiotou G, Paraskeuopoulos T, Vamvasakis E, Chantzi C, Anagnostopoulou S: Ultrasound examination of the sciatic nerve at two different locations in the lateral thigh: a new approach of identification validated by anatomic preparation. Acta Anaesthesiol Scand 2007;51: 780–781.
- Sites BD, Neal JM, Chan V: Ultrasound in regional anesthesia: where should the “focus” be set? Reg Anesth Pain Med 2009;34:531–533.
- Taha AM: A simple and successful sonographic technique to identify the sciatic nerve in the parasacral area. Can J Anaesth 2012;59:263–267.
- Tammam TF: Ultrasound-guided infragluteal sciatic nerve block: a comparison between four different techniques. Acta Anaesthesiol Scand 2013;57: 243–248.
- Tran DQ, Muñoz L, Russo G, Finlayson RJ: Ultrasonography and stimulating perineural catheters for nerve blocks: a review of the evidence. Can J Anaesth 2008;55:447–457.
- Tsui BC, Dillane D, Pillay J, Ramji AK, Walji AH: Cadaveric ultrasound imaging for training in ultrasound-guided peripheral nerve blocks: lower extremity. Can J Anaesth 2007;54:475–480.
- Tsui BC, Finucane BT: The importance of ultrasound landmarks: a “traceback” approach using the popliteal blood vessels for identification of the sciatic nerve. Reg Anesth Pain Med 2006;31:481–482.
- Tsui BC, Ozelsel TJ: Ultrasound-guided anterior sciatic nerve block using a longitudinal approach: “expanding the view.” Reg Anesth Pain Med 2008; 33:275–276.
- van Geffen GJ, Bruhn J, Gielen M: Ultrasound-guided continuous sciatic nerve blocks in two children with venous malformations in the lower limb. Can J Anaesth 2007;54:952–953.
- van Geffen GJ, Gielen M: Ultrasound-guided subgluteal sciatic nerve blocks with stimulating catheters in children: a descriptive study. Anesth Analg 2006;103:328–333.
- Young DS, Cota A, Chaytor R: Continuous infragluteal sciatic nerve block for postoperative pain control after total ankle arthroplasty. Foot Ankle Spec 2014;7:271–276.