Learning objectives
- Pathogenesis of right heart failure (RHF)
- Treatment of RHF
- Anesthetic management of RHF
Definition and mechanisms
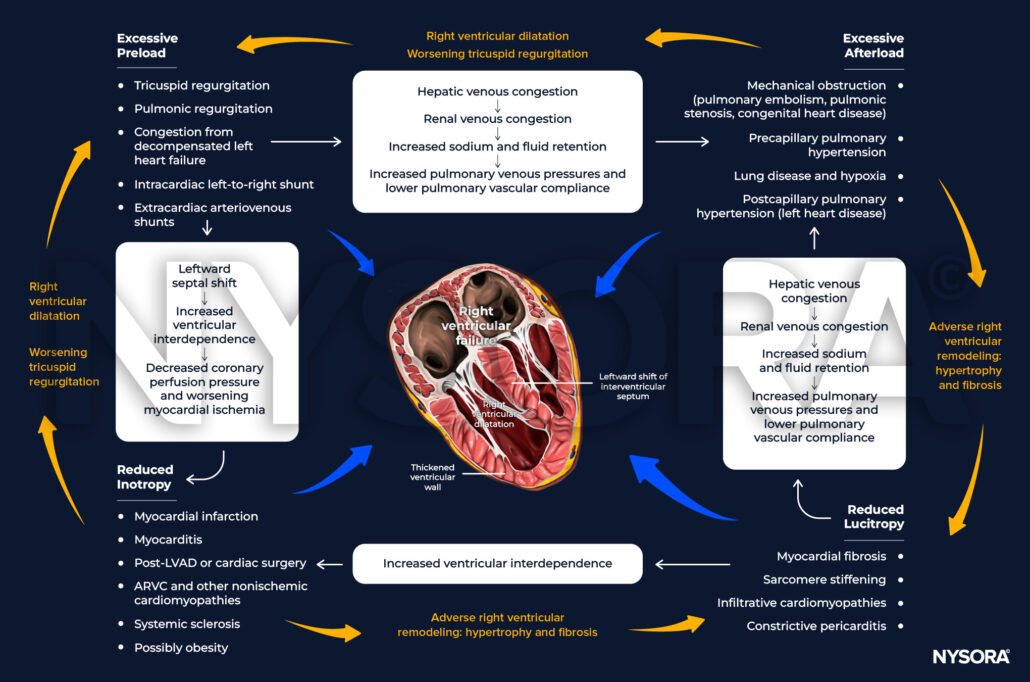
- Right heart failure (RHF) is defined as dysfunction of the right heart structures, predominantly the right ventricle (RV), but also the tricuspid valve and right atrium
- Impaired vena cava flow, resulting in an impaired ability of the right heart to perfuse the lungs at normal central venous pressures, can also cause RHF
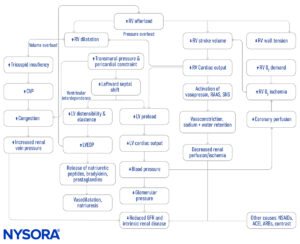
- Ventricular interdependence, the phenomenon whereby the function, volume, or pressure in one ventricle can directly influence that of the other, contributes to right heart failure in case of left ventricular dysfunction
- Vice versa, when RV pressure or volume overload occurs, the RV can affect LV performance and result in a decreased LV preload and contractility
- Elevated filling pressures on the right side of the heart lead to backward failure and systemic venous congestion
- Backward failure:
- Negatively affects the hepatic function
- Causes acute kidney injury and aggravates further fluid retention and worsening RHF
- Fundamental management principles involve optimizing rate, rhythm, perfusion, and preload, whilst maintaining contractility and minimizing afterload
Signs and symptoms
- Breathlessness
- Chest discomfort
- Palpitations
- Swelling
- Elevated jugular venous pressure/jugular venous distention
- Hepatojugular reflux
- Peripheral edema
- Bloating/early satiety/abdominal discomfort
- Hepatosplenomegaly/hepatic pulsation
- Ascites
- Pleural effusion
- Prominent S2 (P2) (PH)
- Right-sided S3 gallop
- TR murmur
- RV heave
- Paradoxical pulse
Causes
Decreased RV contractility RV volume overload RV pressure overload
Acute Sepsis Acidosis
LVAD support Hypoxia
Myocarditis Acute Respiratory Distress Syndrome
Perioperative injury/ischemia (postcardiotomy) Positive pressure ventilation
Pneumonia
Mechanical ventilation
Chronic Right ventricular cardiomyopathy Left heart disease
Arrhythmogenic right ventricular cardiomyopathy Single ventricle
Ebstein anomaly Pericardial disease
Pulmonary regurgitation Pulmonary hypertension (PH)
Transposition of the great arteries Chronic thromboembolic Pulmonary hypertension (PH)
Tricuspid regurgitation (TR) Pulmonary stenosis
Congenital heart disease with a shunt (ASD or anomalous pulmonary venous return) Left-sided valvular heart disease
Restrictive cardiomyopathy
Chronic obstructive pulmonary disease
Right ventricular outflow tract obstruction
Another important mechanism that leads to RHF is intrinsic RV myocardial disease:
- RV ischemia or infarct
- Infiltrative diseases such as amyloidosis or sarcoidosis
- Arrhythmogenic right ventricular dysplasia (ARVD)
- Cardiomyopathy
- Microvascular disease
RHF may be caused by impaired filling which is seen in the following conditions:
- Constrictive pericarditis
- Tricuspid stenosis
- Systemic vasodilatory shock
- Cardiac tamponade
- Superior vena cava syndrome
- Hypovolemia
Diagnosis
- Chest X-ray
- ECG
- echocardiogram
- Blood test (natriuretic peptides)
- MRI/CT
- Cardiac catheterization
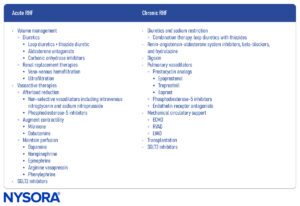
Treatment
Classification Dose (i.v. unless stated) Effects Advantages Disadvantages
Noradrenaline Vasopressor 0.02-0.2 µg/kg/min Vasoconstriction, ↑SVR, ↑myocardial O2 delivery, ↑PVR Cheap, easy to titrate, familiarity Arrhythmias, ↑PVR in higher doses
Vasopressin Vasopressor 1-4 units/min Vasoconstriction, ↑SVR, pulmonary vasodilatation at low doses via endothelial nitric oxide pathway, ↑myocardial O2 delivery Catecholamine-sparing, less ↑PVR than noradrenaline, easy to titrate Expensive, bradycardia, splanchnic ischemia
Dobutamine Inodilator 2.5-10 µg/kg/min Inotropy, ↑contractility, ↓SVR, PVR Easy to titrate, cheap ↑O2 demand, tachyarrhythmias, systemic hypotension
Milrinone Inodilator 0.75-0.75 µg/kg/min Inotropy, ↑contractility, ↓SVR, PVR Pulmonary vasodilatation Systemic hypotension
Levosimendan Inodilator Loading dose: 6-12 µg/kg/min over 10 min followed by infusion of 0.1 µg/kg/min ↑Contractility No effect on myocardial oxygen demand Expensive, tachycardia, hypotension, headache
Sildenafil Pulmonaryvasodilator 10 mg t.d.s.
Oral: 20-100 mg t.d.s↓PVR, ↑Contractility Oral administration for patients with chronic disease Long terminal half-life (4e18 h), ↓SVR
Epoprostenol Pulmonaryvasodilator 1-2 ng/kg/min
Nebulized: 0.2-0.3 ml/min of a 10-20 µg/mil solution↓PVR, ↑V/Qmismatch As efficient as nitric oxide Systemic hypotension with i.v. administration, flushing, headaches
Anesthetic management

Suggested reading
- Houston BA, Brittain EL, Tedford RJ. Right, Ventricular Failure. N Engl J Med. 2023;388(12):1111-1125.
- Price LC, Martinez G, Brame A, et al. Perioperative management of patients with pulmonary hypertension undergoing non-cardiothoracic, non-obstetric surgery: a systematic review and expert consensus statement. Br J Anaesth. 2021;126(4):774-790.
- Murphy, E., Shelley, B., 2019. Clinical presentation and management of right ventricular dysfunction. BJA Education 19, 183–190.
- Cops J, Mullens W, Verbrugge FH, et al. Selective abdominal venous congestion induces adverse renal and hepatic morphological and functional alterations despite a preserved cardiac function. Sci Rep. 2018;8(1):17757.
- Cops J, Mullens W, Verbrugge FH, et al. Selective abdominal venous congestion to investigate cardiorenal interactions in a rat model. PLoS One. 2018;13(5):e0197687. Published 2018 May 29.
- Konstam MA, Kiernan MS, Bernstein D, et al. Evaluation and Management of Right-Sided Heart Failure: A Scientific Statement From the American Heart Association. Circulation. 2018;137(20):e578-e622.
- Murphy, E., Shelley, B., 2018. The right ventricle—structural and functional importance for anaesthesia and intensive care. BJA Education 18, 239–245.
- Gorter TM, van Veldhuisen DJ, Bauersachs J, et al. Right heart dysfunction and failure in heart failure with preserved ejection fraction: mechanisms and management. Position statement on behalf of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20(1):16-37.
- Kevin LG. 2007. Right ventricular failure. Continuing Education in Anaesthesia Critical Care & Pain. 7;3:89-94.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com