The purpose of this study was to test the hypothesis that femoral nerve block with genitofemoral nerve infiltration provides sufficient analgesia and superior recovery characteristics to spinal anesthesia for long saphenous vein stripping procedures performed in the ambulatory setting.
Based on: “Vloka JD, Hadzic A, Mulcare R, Lesser JB, Kitain E, Thys DM. Femoral nerve block versus spinal anesthesia for outpatients undergoing long saphenous vein stripping surgery. Anesth Analg 1997;84:749-52.”
Abbreviations LSVS – Long saphenous vein stripping; FNB – Femoral nerve block; PACU – Post-anesthesia care unit; SSU – Short stay unit
|
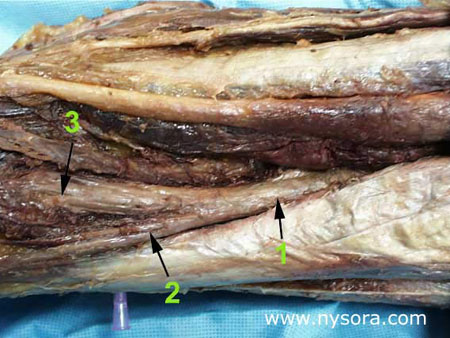
Significance Long saphenous vein stripping (LSVS) is frequently used to treat varicose veins of the lower extremity. Nearly 50,000 saphenous vein phlebectomies are performed in the US annually [1]. Since these procedures result in relatively minor surgical trauma, the speed of recovery from anesthesia can significantly influence time to discharge home. The most prevalent anesthetic techniques, general and neuraxial anesthesia, are associated with some complications and have side-effects that make them less than ideal in the outpatient setting. For general anesthesia these include postoperative nausea and vomiting [2,3], backache [4], sore throat [5], and myalgias [6]. On the other hand, postoperative backache [7], post-dural puncture headache[8,9], slow resolution of the block or the development of postural hypotension [10], can complicate the postoperative course of neuraxial anesthesia and result in delayed discharge. By confining the anesthesia to the region that is being operated upon, nerve block anesthesia can avoid many of the disadvantages of both general and neuraxial anesthesia. However, despite the potential advantages, neuronal block remains infrequently utilized in outpatients. The purpose of this study was to test the hypothesis that femoral nerve block with genitofemoral nerve infiltration provides sufficient analgesia and superior recovery characteristics to spinal anesthesia for long saphenous vein stripping procedures performed in the ambulatory setting. Methods 68 outpatients undergoing LSVS were randomized to receive either femoral nerve block (FNB) or spinal anesthesia. All patients received midazolam 1-2 mg, and some received fentanyl 0-100 µcg intravenously prior to introduction of the anesthetic. Additional doses of midazolam and fentanyl were administered as necessary to allay the anxiety or discomfort not related to surgical instrumentation (positioning, discomfort during blood pressure checking, etc.). In case of specific complaints related to the surgical procedure (i.e., pain on instrumentation), infiltration with local anesthetic was used instead of intravenous supplementation.  Femoral nerve block was performed with patient in the supine position, Figure 1. Using a peripheral nerve stimulator (DualStim®; DX, Professional Instruments, Huston, TX), with the negative electrode connected to the needle and the reference electrode connected to the lateral thigh, contractions of the quadriceps femoris muscle were sought. After the contractions were obtained at 0.6 mA, the current was decreased by a single operator using a foot-controlled unit (Hadzic A, Vloka JD.: U.S. Patent Serial No. No. 08/419, 419 for “Apparatus for Locating and Anesthetizing Peripheral Nerves and a Method Therefor”), at a stimulating current of 0.4 mA or less, 30 mL of 3% chloroprocaine was injected. The solution of chloroprocaine was alkalinized by adding 1 mEq of sodium bicarbonate in the bottle of 30 mL commercially prepared solution of 3% chloroprocaine (Abbott Labs, Chicago, IL).  Branches of the genitofemoral nerve were blocked by subcutaneous injection of 7 mL of 1% lidocaine, Figure 2. Spinal anesthesia was performed using the midline approach, with the patient in the sitting position, aiming for the L2-3 or L3-4 interspace. Following infiltration of the skin with 3 mL of 1% lidocaine, a 24-gauge 90 mm long spinal needle (Pencil point, Gertie MarxTM Spinal Needle, IMD, Inc.Park City, UT) was inserted through a 20 gauge introducer. After aspirating approximately 0.5 mL of cerebrospinal fluid, 65 mg of 5% hyperbaric lidocaine was injected, and the patients were immediately positioned in the supine position. The sensory level of spinal anesthesia was assessed 10 minutes after subarachnoid injection. All anesthetics were administered in the operating room, and all procedures were performed by the same surgeon using the identical surgical technique. Surgical Technique With the patient in the supine position, a 1-2 cm incision was made over the sapheno-femoral vein junction. The long saphenous vein was identified and its branches were ligated. After division flush with the common femoral vein, an internal stripper was passed retrograde and retrieved through an incision in the proximal medial leg. After ligation of the distal long saphenous vein, the upper long saphenous vein was stripped from the groin to the proximal leg in the cephalad-caudad direction. The incisions were closed with staples. Following the operation, the patients were taken to the post-anesthesia care unit PACU (Phase 1 recovery) for observation. Recovery was assessed using a postanesthetic recovery score (Aldrete score) [11] and clinical criteria (stable vital signs, able to sit up without dizziness and/or nausea, alert and oriented, tolerable or no pain). The assessments were done upon arrival to the PACU and every 15 minutes thereafter until discharge from the PACU to the short stay unit SSU (Phase 2 recovery). The patients met the criteria for transfer from the PACU to the SSU after they stayed a minimum of 30 minutes in the PACU and achieved a postanesthetic discharge score of 9 or more. PACU time was calculated from the moment the patient was admitted to the PACU until transfer to the SSU. In the SSU, patients were assessed for discharge readiness (home readiness) every 30 minutes. Home readiness was defined as: stable vital signs, ability to ambulate and dress with minimal assistance, ability to tolerate liquids orally with minimal nausea and vomiting and ability to void. SSU time was defined as the time from admission to the (PACU) for observation, and then transferred to the short stay unit (SSU) prior to discharge home. Hospital time was defined from the time the patient entered the operating room until the home readiness criteria were met. The treatment of pain in the PACU consisted of intravenously administered Morphine sulfate 1 to 2 mg every 5 to 10 minutes if the patients experienced pain and requested pain medication, while in the SSU patients received acetaminophen 300 mg with codeine 30 mg on demand. Decisions regarding the need for pain treatment, transfer to the SSU and discharge home were made by anesthesiologists and nurses blinded to the study goals. The patients were instructed to take acetaminophen 300 mg with codeine 30 mg every 3-4 hours as needed for pain at home. Data collected included: patient demographics, time from start of anesthesia (patient in the operating room) to surgical incision, time from introduction of the block to surgical incision, duration of stay in the PACU and in the SSU, postoperative complications, incidence of pain requiring therapy, and requirement for analgesics in the hospital and at home during the first postoperative 24 hours. Study patients were called 24 hours after surgery by a physician blinded to the type of anesthesia. Their responses to questions regarding experiences during block placement, surgery, recovery, postoperative pain and development of any complications were recorded. Specific questions were asked regarding the presence of backache, headache, leg paresthesias and the amount of analgesics taken at home during the first 24 postoperative hours. Patient satisfaction with the anesthetic technique was obtained during the same telephone interview by asking the patients whether they would choose the same type of anesthesia for another operation, or recommend it to their friends. Statistical analyses included Student’s t tests and chi-square tests. P-values less than 0.05 were considered significant. Results Thirty-six patients received FNB with alkalinized 3% chloroprocaine 3% and 32 patients received spinal anesthesia with 5% hyperbaric lidocaine (mean level obtained was T10). The mean age of the studied population was 46 +/- 12 years, with no significant differences in demographic characteristics between the groups (Table 1). None of the patients were lost to follow-up. After entering the operating room (start of anesthesia care), the mean time to the start of surgery was 21 +/- 5 minutes in the FNB and 20 +/- 6 minutes in the spinal group (non-significant (N.S.)). Following completion of the blocks, the mean time to incision was 8 +/- 5 minutes in the FNB and 10 +/- 6 minutes in the spinal group (N.S.). Mean doses of intravenously administered analgesia/sedation were fentanyl 105 +/- 60 mcg and midazolam 2.8 +/- 1.5 mg in the FNB group and fentanyl 49 +/- 54 mcg and midazolam 2.5 +/- 0.9 mg in the spinal group (p Table 1. Demographic characteristics
The incidence of pain that required treatment prior to discharge home and incidence of post-operative complications are shown in Table1. Significantly fewer patients required pain treatment in the FNB group than in the spinal anesthesia group (p Five (16%) patients in the spinal group reported having headaches 24 hours after the operation vs. none in FNB group (pTable 2describes the reasons for refusal of the spinal anesthesia in the future. Table 2.: Reasons for refusal of the spinal anesthesia in the future.
Discussion In this study, FNB resulted in faster recovery, fewer complications, and better patient satisfaction than spinal anesthesia in outpatients undergoing LSVS. FNB results in anesthesia in the antero-medial thigh and medial aspect of the lower leg. This distribution covers the entire operative field, except the inguinal region, where sensory innervation is derived from the branches of the genito-femoral nerve. Since rapid recovery and ability to ambulate is essential in outpatient surgery, we chose chloroprocaine for FNB. Thirty mL of alkalinized 3% chloroprocaine resulted in a rapid onset of anesthesia that allowed the operation to proceed an average of eight minutes following introduction of the block. The first sign of successful block was the inability of the patient to extend the leg at the knee joint. This was then followed by onset of surgical anesthesia in the described distribution. One hour after the block was performed, the motor component of the block had dissipated, allowing for early ambulation. The remaining sensory block after FNB with 3% chloroprocaine provided longer lasting postoperative analgesia as evidenced by decreased need for analgesics in the PACU/SSU and the first 12 hours postoperatively in patients in the FNB than in the spinal anesthesia group. Although the pain on injection of chloroprocaine has been traditionally considered as one of the disadvantages when using this local anesthetic for neuronal block, none of our patients reported discomfort on injection, despite relatively light premedication. It is possible that the pain on injection is due to the acidic pH of commercially prepared chloroprocaine, which could be reduced or avoided by adjusting the pH. Taylor et al. reported successful use of FNB for LSVS operation in 1981 [12]. The authors used 20 mL of 1% lidocaine for FNB and infiltration of local anesthetic at the sapheno-femoral vein junction, but the recovery times were not reported. Since then, the authors in a subsequent reply to a comment have recommended use of 0.5% bupivacaine for the same operation [13]. In our experience, 1% lidocaine and 0.5% bupivacaine both result in motor block when used for FNB, frequently lasting over three hours when 1% lidocaine is used, and over 56 hours when 0.5 % bupivacaine is used. Since the motor block interferes with early ambulation, we consider these techniques less suitable for modern outpatient surgery. The relatively high incidence of mild to moderate backache (53%) and back pain with a radicular component (16%) after spinal anesthesia with 5% hyperbaric lidocaine is of concern. The appearance of these symptoms after spinal anesthesia has been attributed to the loss of protective muscle tone during positioning on the operating room table and to the use of hyperbaric 5% lidocaine [7]. At the time our project was initiated, the concerns regarding the use of hyperbaric lidocaine in spinal anesthesia had not been widely publicized. The symptoms suggestive of transient radicular irritation in two of our patients, again, leads to the question of the appropriateness of using lidocaine for spinal anesthesia in outpatients[7]. Since FNB does not result in complete anesthesia of the lower extremity as spinal anesthesia does, patients frequently express anxiety when the surgeon is manipulating the leg even in the absence of surgical stimuli. Thus, although the quality of anesthesia did not appear to differ between the groups, the patients in the FNB group received significantly more fentanyl. Verbal reassurance and short-acting intravenously administered sedatives before the surgical manipulation is begun is very important here, as it is with most other regional anesthesia techniques. Additionally, local infiltration of the area of the incision in the groin may occasionally be needed. It should be recognized, however, that discomfort on surgical manipulation in this area is due to incomplete block of the genitofemoral nerve and not a failure to achieve block of the femoral nerve. In summary, optimal anesthetic management for outpatient surgery requires that the anesthesia be handled expeditiously, with minimal residual postoperative anesthetic effects and side-effects that may interfere with early discharge home. Our results show that FNB using 3% chloroprocaine results in excellent anesthesia in outpatients undergoing LSVS. When compared to spinal anesthesia with 5% hyperbaric lidocaine, this technique resulted in a more favorable recovery, higher patient satisfaction and fewer complications. REFERENCES: 1. Graves E. Detailed diagnoses and procedures, National Hospital Discharge Survey, 1992. Series 13: data from the National Health Survey. Vital Health Stat 13 1994;118:1-281. 2. Watcha MF, White PF. Postoperative nausea and vomiting. Anesthesiology 77:162-184, 1992. 3. Palazzo MGA, Strunin L. Anesthesia and emesis. I: etiology. Can Anaesth Soc J 1984;31:178-87. 4. Dahl JB, Schultz P, Anker-Moller E, et al. Spinal anaesthesia in young patients using a 29-gauge needle: Technical considerations and an evaluation of postoperative complaints compared with general anaesthesia. Br J Anaesth 1990;64:178-2. 5. Monroe MC, Gravenstein N, Saga-Rumley S. Postoperative sore throat: effect of oropharyngeal airway in orotracheally intubated patients. Anesth Analg 1990;70:512-6. 6. Philip B. Ambulatory anesthesia. Semin Surg Oncol 1990;6:177-83. 7. Schneider M, Ettlin T, Kaufmann M, et al. Transient neurologic toxicity after hyperbaric subarachnoid anesthesia with 5% lidocaine. Anesth Analg 1993;76:1154-7. 8. Carbaat PAT, van Crevel H. Lumbar puncture headache: controlled study on the preventive effect on 24 hours’ bed rest. Lancet 1981;2(8256):1133-35. 9. Cruickshank RH, Hopkinson JM. Fluid flow through dural puncture sites. An in vitro comparison of needle point types. Anaesthesia 1989;44:415-8. 10. Pflug AE, Aasheim GM, Foster C. Sequence of return of neurological function and criteria for safe ambulation following subarachnoid block (spinal anaesthetic). Can Anaesth Soc J 1978; 25(2):133-9. 11. Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg 1970;49:924-34. 12. Taylor EW, Fielding JW, Keighley MR, Alexander-Williams J. Long saphenous vein stripping under local anaesthesia. Ann R Coll of Surg of Engl 1981;63:206-7. 13. Taylor EW, Fielding JW, Keighley MR, Alexander-Williams J. Comment to the letter: Long saphenous vein stripping under local anaesthesia. Ann R Coll of Surg of Engl 1981;63:364. |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||