Learning objectives
- Anesthetic management of spine surgery
Definition and mechanisms
- The scope of spine surgery is vast
- Patients usually present with one of five pathologies at any site from cervical to lumbosacral:
- Major spinal surgery is often associated with major bleeding, infection, and postoperative respiratory complications
- 1% incidence of spinal cord damage
Surgical approach
- The majority of spinal procedures are performed in the prone position
- Exceptions: anterior cervical surgery, thoracic discectomies
- Complications of the prone position:
- Accidental extubation
- Ophthalmic complications (corneal abrasions, postoperative visual loss)
- Peripheral nerve injury (ulnar nerve at the elbow, brachial plexus)
- Pressure injuries (skin necrosis, breast/genital injury)
- Abdominal compression (venous congestion in epidural veins, organ ischemia, impaired ventilation, lower limb thrombosis, and reduced cardiac output)
- Support the patient with pillow, gel pads, and foam bolsters to ensure that:
- The abdomen is free
- The head is at or above the level of the heart in a neutral position using a headrest or a Mayfield head fixator
- The eyes are taped closed, without padding, and free from external pressure, regularly checking them where possible
- The arms are in a natural position no more than 90° abduction with slight internal rotation paying particular attention to the ulnar nerve at
- the elbow
- Specific devices are available to facilitate proning: Montreal mattress, Jackson operating table, Wilson Frame, and the Andrews operating table
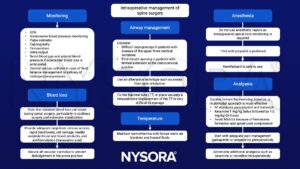
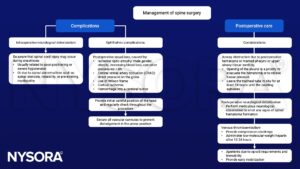
Management
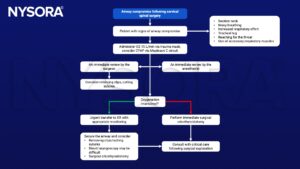
Management of airway compromise following cervical spinal surgery
Suggested reading
- Pollard BJ, Kitchen, G. Handbook of Clinical Anaesthesia. Fourth Edition. CRC Press. 2018. 978-1-4987-6289-2.
- Nowicki R. 2014. Anaesthesia for major spinal surgery. Continuing Education in Anaesthesia Critical Care & Pain. 14;4:147-152.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com


