Learning objectives
- Recognize the signs and symptoms of strabismus
- Describe the risk factors of strabismus
- Anesthetic management for patients undergoing strabismus surgery
Definition and mechanisms
- Strabismus surgery is surgery of the extraocular muscles (tightening, lengthening, transposing, or shortening the eye muscles) to correct strabismus, the misalignment of the eyes
- It is the most common ophthalmic surgery in pediatric patients
- Strabismus occurs in 3-5% of children worldwide
- Strabismus results from an imbalance in extraocular muscle function → two different images (one from each eye) are transmitted to the brain, resulting in loss of visual depth → in children, the brain may suppress the image from the weaker eye, impairing visual development and leading to amblyopia (decreased vision in a normal healthy eye; lazy eye)
- The prognosis is good if the correction is performed as early as possible (before the child reaches the age of 8 years)
Signs and symptoms
- Strabismus may involve one or both eyes
- The affected eye can deviate outward (exotropia), inward (esotropia), upward (hypertropia), or downward (hypotropia)
- The deviation may be intermittent or constant, large magnitude (large angle) or small magnitude (small angle)
- Diplopia (double vision)
- Loss of stereopsis
- Headache
- Inability to read comfortably
- Fatigue when reading
- Amblyopia (loss of visual acuity)
- Psychosocial issues (interferes with normal eye contact with others)
Risk factors
- Premature birth
- Low birth weight
- Smoking during pregnancy
- Family history
- Down syndrome (29%)
- Cerebral palsy (53%)
- Syndromes with craniofacial dysostosis (up to 90%)
Patient characteristics
- Infantile strabismus needs early surgery (6-12 months) for the best visual outcome
- Rare association with primary muscle diseases and malignant hyperthermia
- Associated syndromes: Apert syndrome, Cri du chat syndrome, Crouzon syndrome, Down syndrome, Goldenhar syndrome, Marfan syndrome, Moebius syndrome, Stickler syndrome, Turner syndrome
Problems
- Airway not accessible because of the microscope’s position
- Avoid suxamethonium
- Can trigger malignant hyperthermia in susceptible patients
- Can cause tonic contracture of extraocular muscles, interferes with forced duction test
- Oculocardiac reflex
- Topical adrenaline is often used to reduce bleeding and may be absorbed systemically, watch dose in small children
- High incidence of postoperative nausea and vomiting (PONV)
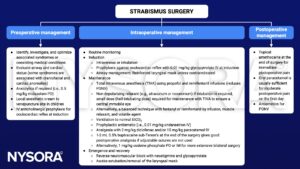
Management
Suggested reading
- Lewis H, James I. Update on anaesthesia for paediatric ophthalmic surgery. BJA Educ. 2021;21(1):32-38.
- Chua AW, Chua MJ, Leung H, Kam PC. Anaesthetic considerations for strabismus surgery in children and adults. Anaesthesia and Intensive Care. 2020;48(4):277-288.
- Pollard BJ, Kitchen G. Handbook of Clinical Anaesthesia. 4th ed. Taylor & Francis group; 2018. Chapter 18 Ophthalmic surgery, Slater RM.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com


