Learning objectives
- Describe the pathophysiology and symptoms of a subarachnoid hemorrhage
- Diagnose and clinically grade a subarachnoid hemorrhage
- Manage patients presenting with a subarachnoid hemorrhage
Background
- Subarachnoid hemorrhage account for 5% of all strokes
- Mortality rate ~50%
- One-third of survivors need lifelong care
- Prompt diagnosis and early treatment are critical
Pathophysiology
- Etiology
- Intracranial aneurysm (85% of cases)
- Arteriovenous malformations
- Trauma
- Moyamoya disease
- Risk factors
- Hypertension
- Atherosclerosis
- Cocaine use
- Alcohol abuse
- Smoking
- Connective tissue disorders
- Coarctation of the aorta
- Congenital conditions (autosomal-dominant polycystic kidney disease, Ehlers Danlos Type 4, familial intracerebral aneurysms)
- Cause
- Hemodynamically induced shear stress (sudden increase in cerebrovascular arterial pressure)
- Aneurysmal rupture leads to blood quickly traversing through the intracranial cisterns and subarachnoid space (within seconds)
- Global cerebral ischemia resulting from increased intracranial pressure, decreased cerebral perfusion, and reduced cerebral blood flow
- Intraventricular bleeding can cause acute ventricular dilatation and hydrocephalus
- Brain tissue oxygen pressure and pH are reduced
- Compensatory hypertension occurs within minutes to hours
- Blood-brain barrier disruption, cerebral edema, and a thromboinflammatory cascade
Signs & symptoms
- Sudden onset of “worst headache of life”
- Loss of consciousness
- Nausea and/or vomiting
- Nuchal rigidity
- Photophobia
- Seizures
- Comatose and hypertensive at presentation
Diagnosis
- Non-contrast cranial CT
- Lumbar puncture in patients with a high index of suspicion and a normal CT scan (red blood cell count, bilirubin level, and xanthochromia)
- CT angiogram and/or digital subtraction angiography to identify the cause
Clinical grading
| Grade | World Federation of Neurologic Surgeons | Hess and Hunt | Fisher (CT scan appearance) |
|---|---|---|---|
| 1 | Glasgow Coma Scale score 15, no motor deficit | Asymptomatic or minimal headache and slight nuchal rigidity | No blood detected |
| 2 | Glasgow Coma Scale score 13-14, no motor deficit | Moderate to severe headache nuchal rigidity, no neurological deficit other than cranial nerve palsy | Diffuse thin layer of subarachnoid blood (vertical layers <1 mm thick) |
| 3 | Glasgow Coma Scale score 13-14 with motor deficit | Drowsy, confusion, or mild neurological deficit | Localized clot or thick layer of subarachnoid blood (vertical layers ≥1 mm thick) |
| 4 | Glasgow Coma Scale score 7-12, with or without motor deficit | Stupor, moderate-to-severe hemiparesis, possibly early decerebrate rigidity and vegetative disturbances | Intracerebral or intraventricular blood with diffuse or no subarachnoid blood |
| 5 | Glasgow Coma Scale score 3-6, with or withour motor deficit | Deep coma, decerebrate rigidity, moribund appearance |
Complications
- Re-bleeding
- Seizures
- Hydrocephalus
- Vasospasm
Management
- Acute management
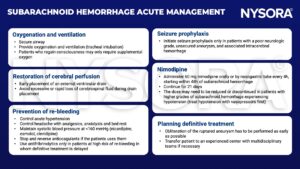
- Treatment options
-
- Endovascular coiling: Preferred in geriatric patients, particularly those with high-grade aneurysmal subarachnoid hemorrhage from the rupture of basilar apex aneurysm
- Surgical clipping: Preferred in patients with large intraparenchymal hematomas, aneurysm of the middle cerebral artery, and in those not likely to be compliant with long-term follow-up
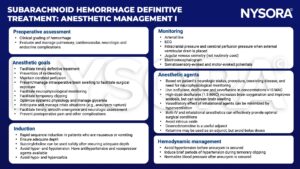
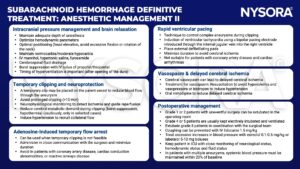
- Anesthetic management
Suggested reading
- Deepak Sharma; Perioperative Management of Aneurysmal Subarachnoid Hemorrhage: A Narrative Review. Anesthesiology 2020; 133:1283–1305
- Kundra S, Mahendru V, Gupta V, Choudhary AK. Principles of neuroanesthesia in aneurysmal subarachnoid hemorrhage. J Anaesthesiol Clin Pharmacol. 2014;30(3):328-337.
- Luoma A, Reddy U. Acute management of aneurysmal subarachnoid haemorrhage. Continuing Education in Anaesthesia Critical Care & Pain. 2013;13(2):52-8.
We would love to hear from you. If you should detect any errors, email us customerservice@nysora.com